Abstract
Purpose
To compare the outcomes between laparoscopic total extraperitoneal (TEP) repair and prolene hernia system (PHS) repair for inguinal hernia.
Methods
A retrospective analysis of 237 patients scheduled for laparoscopic TEP or PHS repair of groin hernia from 2005 to 2009 was performed.
Results
The mean age was 52.3 years in TEP group and 55.7 years in PHS group. Of 119 TEP cases, 98 were indirect inguinal hernia, 15 direct type, 5 femoral hernia and 1 complex hernia; Of 118 PHS cases, 100 indirect, 18 direct type. All in TEP group were performed under general anesthesia and 64% of PHS group were performed under spinal or epidural anesthesia. Preoperatively, 10 cases of recurrent inguinal hernia were involved in our study (4 in TEP, 6 in PHS group). The mean operative time was similar in both groups (74.8 in TEP, 71.2 in PHS group), however mean hospital stay (1.6 days in TEP, 3.2 days in PHS group, P = 0.018) and mean usage of analgesics (0.54 times in TEP, 2.03 times in PHS group, P < 0.01), complications (36 cases in TEP, 6 cases in PHS group, P < 0.01) showed statistical differences. There is only 1 case of postoperative recurrence inguinal hernia in PHS group but it has no statistical significance (P = 0.314).
Inguinal hernia repair is one of the most common procedures in field of general surgery. There have been various methods for inguinal hernia repair, but recently, so called 'tension-free repair' is the procedure of choice [1] due to its low recurrence rate. These tension-free repair procedures can be roughly categorized into two groups; laparoscopic and open anterior approach. As laparoscopic hernia repair, total extraperitoneal (TEP) repair, transabdominal preperitoneal (TAPP) repair, and intraperitoneal onlay mesh (IPOM) repair are well known. Among them, TEP is accepted as the most ideal method because it can avoid entry into the peritoneal cavity, which can cause intraperitoneal complication such as bowel injury or obstruction [2]. And among open tension-free methods, such as Lichtenstein's operation, repair using mesh plug or prolene hernia system (PHS), PHS repair is becoming an accepted and popular technique because of shorter operating time, about 10%, and it's low recurrence rate [3,4].
A retrospective analysis of 237 patients scheduled for laparoscopic TEP or PHS repair of unilateral inguinal hernia from August 2005 to August 2009 was performed. In study duration, 15 patients who had bilateral inguinal hernia and 11 patients who had TAPP repair performed, 4 patients who had IPOM repair performed were excluded from this data. Also, the patients who had shorter than 12 months of follow up were excluded. A total of 237 (TEP, 119; PHS, 118) patients were involved. Until 2007, we had mainly performed PHS repair method, but thereafter, have performed laparoscopic TEP repair, except in the following cases; the anesthesiologist recommended that the patient was not suitable for general anesthesia, the patient didn't want TEP repair due to cost. All operations were performed by a single surgeon. Outcome was compared in demographics and perioperative details with postoperative data.
In all procedures, we opened the inguinal canal under oblique incision and the hernia sac was identified and isolated from spermatic cord. In indirect type, the sac reducted to the peritoneal cavity without ligation. In direct type, after reducting the sac without ligation the preperitoneal space was made digitally in a blunt manner. Underlay patch of mesh (PHS, monofilament knitted polypropylene; Ethicon Inc., Somerville, MA, USA) was located in the prepared preperitoneal space without any fixation and determined that it was well-located under view. The onlay patch of mesh was located around the spermatic cord and well positioned with some fixation.
A laparoscopic TEP repair is performed using a three-port technique. To create the pre-peritoneal space, a 15 mm skin transverse incision is made at the inferior edge of umbilicus. The incision is carried down to the contralateral side of the anterior sheath of the rectus abdominis muscle. Then, a small incision is made in the anterior sheath to expose the rectus abdominis muscle. A channel between the rectus muscle and the posterior sheath is created with peanuts in Kelly, so that a small tunnel is made in the direction to pubis between the rectus abdominis muscle and the peritoneum. Using spacemaker dissection balloon (Autosuture, Norwlk, CT, USA), the pre-peritoneal space is developed. Finally, another 5 mm port is placed 2 cm superior to symphysis pubis in the midline and another 5 mm port is placed in the middle between the 2 existing ports.
In most direct inguinal hernias, the loosened transversalis fascia is fixed to Cooper's ligament with a 5 mm spiral tack (Tyco Healthcare, Norwalk, CT, USA) to reduce dead space. In indirect inguinal hernias, the sac is completely isolated and reducted. In addition, in femoral hernias, the sac is completely reducted. A 15 × 10 cm polyester mesh (Parietex, sofradim, Trevoux, France) is placed and anchored with 5 mm spiral tacks (Tyco Healthcare); the mesh is fixed in Cooper's ligament routinely, and, occasionally, there are additional fixations.
The operative time was recorded from skin incision to skin closure. Hematoma was defined as presence of ecchymosis on operative site. Scrotal swelling was included only when the patient complained during follow-up, and seroma was defined as the case in which the aspirated fluid was over 5 mL. Sustained pain was defined if operative site pain was sustained 3 months after surgery. The length of hospital stay was defined as the total number of nights spent in the hospital after surgery. Recurrence after operation was diagnosed upon physical examination. The patients were followed up in the outpatient hernia clinic department regularly. Some patients were followed up by phone call; but if not available by phone, the last follow up findings were used for data. Patients who had shorter than 12 months of follow up were excluded from our data.
Chi-square test was used for analysis of independency of data in both group, and the mean data was compared by independent t-test. Data collected in the database were analyzed using SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA). A P-value less than 0.05 was considered as significant.
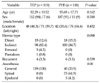
As Table 1 shows, the mean follow up duration was 32 months (range, 13 to 58 months). The mean age of TEP group was 52.3 ± 19.5 (range, 15 to 87) and 55.7 ± 17.7 years (range, 17 to 90 years) in PHS group. The male to female sex ratio of the 237 patients was 112:7 in TEP group and 107:11 in PHS group. One hundred and forty-seven cases were right side inguinal hernia (TEP, 7 1; PHS, 76) and 90 cases were left side (TEP, 48; PHS, 42). Indirect types were 82%, and there were 5 cases of femoral hernia and 1 case of pantaloon hernia in TEP group only. All TEP group surgeries were performed under general anesthesia. But 34% of cases in PHS group were performed under general anesthesia, and other cases under spinal or epidural anesthesia. Preoperatively, 10 cases of recurrent hernia were involved in our study (4 in TEP, 6 in PHS group).
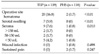
Peri-operative data is shown in Table 2. The mean operation time in TEP and PHS group was 74.8 ± 36.5 (range, 30 to 290) and 71.2 ± 33.2 minutes (range, 25 to 225 minutes) respectively; it was similar between the two groups. The hospital stay in TEP and PHS groups were 1.6 ± 1.5 (range, 1 to 11) and 3.2 ± 6.9 days (range, 1 to 15 days), respectively; shorter in TEP than in PHS group (P = 0.018). The times of analgesics usage were 0.5 ± 0.5 (range, 0 to 1) and 2.0 ± 2.8 (range, 0 to 21); less use in TEP than in PHS group (P < 0.01). However, postoperative complications more frequently occurred in TEP (36 cases, 30.3%) than in PHS (6 cases, 5.1%) group (P < 0.01). Only one recurrence was detected during follow up period in PHS group, but it did not show any statistical significance.
Table 3 describes the details of postoperative complication in each group. The operative site hematoma was detected in 20 cases (16.8%), scrotal swelling in 7 cases (5.9%) and seroma in 9 cases (7.6%) of TEP group. On the other hand, there were only 2 hematoma and 1 seroma in PHS group. Therefore, the hematoma, swelling and seroma were more frequently detected in TEP than in PHS group (P < 0.01, P < 0.01, P = 0.010, respectively). No patient suffered from sustained pain in TEP group, but 2 patients suffered in PHS group (P = 0.247). There were no other serious complications in either group.
Bassini's procedure [8] was standard procedure for repair of inguinal hernia until tension-free hernia repair procedure using mesh was introduced by Lichtenstein and Shulman [9]. The tension-free hernia repair method was developed and now there are various methods such as plane mesh, plug mesh, PHS repair, and laparoscopic TEP, TAPP, IPOM repair. Of these, the PHS repair was introduced by Gilbert et al. [4] in 1999, and has become a popular procedure because it is easy to perform when; the anatomy is not clear [10], there is decreased operating time [3], low recurrent rate [4], and/or it could prevent femoral hernia [10]. And laparoscopic TEP repair has been considered as the laparoscopic procedure of choice for inguinal hernia [11] because of the following; high recurrence rate after IPOM [12], TEP can avoid entry into the peritoneal cavity [2], the incidence of serious complications is lower after TEP than TAPP [11].
We have compared these two popular procedures for inguinal hernia; there was no difference in demographic features between the two groups. All TEP repairs and 34% of PHS repairs were performed under general anesthesia, but no postoperative complication related to general or spinal anesthesia was observed.
Many authors have reported that the operating time for laparoscopic hernia repair procedure could be longer than open [13,14], and in some [7] it was the same. In our results, the operative time was similar between the two groups. Variation of the operative time can be influenced by the operator or author (his or her operative style, habit, tendency). In our data, all operations were performed by a single surgeon, so, we could say there was no difference in the operative time between laparoscopic hernia repair and open hernia repair.
Hospital stay was shorter in TEP group (1.6 days) than PHS group (3.1 days). Other authors have reported that TEP repair results in a quicker return to normal functional status [15], and an improved quality-of-life outcome [16]. However, hospital stay was not decided by only patients' physical condition but surgeon's preference, secondary gain such as private insurance, the hospital's turn over rate of sickbed, psychological effect, and traditional beliefs.
The amount of postoperative intravenous or intramuscular analgesics use was lower in TEP group (0.54 times) than PHS group (2.03 times). Recently, Blinman [17] reported very interesting results; even though the sum of incision is same, the total tensions are not equal, so conventional incisions are subject to more total tension than combination of trocar incisions. In this point of view, our result is understandable. And even breakup of incision may have cosmetic effects.
There were no serious complications in both groups. However, minor complications were detected more frequently in TEP group (36 cases, 30.3%) than PHS group (6 cases, 5.1%). Operative site hematoma was the most common complication (16.8%) after TEP repair, but subsided spontaneously without any intervention or medication. Although operative site hematoma was a minor complication, since laparoscopic operation should be considered as a cosmetic standpoint, careful dissection of preperitoneal space, and delicate bleeding control might be required to prevent it. Postoperative scrotal swelling occurred in 7 cases of TEP repair; they were resolved without any intervention. On the other hand, a total of 10 cases of seroma were detected (9 cases of TEP, 1 case of PHS) and aspiration was done; after that there was no recurrence of seroma. There have been reports about the risk factors of seroma formation after laparoscopic TEP [18,19]: large hernia defects, scrotal extension of the hernia, potential cavity exists between the mesh and the transversalis fascia, male gender, and indirect type.
The present study came from a single surgeon's results, so there may be bias; this result cannot be adopted by all surgeons. However, a single surgeon's results has a strong point; coherent standards were applied to postoperative outcomes such as operative time, hospital stay, and amount of analgesics.
In conclusion, laparoscopic TEP repair and PHS hernia repair had acceptably low recurrence rates and similar operating times. The advantage of TEP repair was shorter hospital stay, lower analgesics use, and cosmetic effect. However, the TEP repair had more minor postoperative complications than those of PHS repair.
Figures and Tables
References
1. Eklund AS, Montgomery AK, Rasmussen IC, Sandbue RP, Bergkvist LA, Rudberg CR. Low recurrence rate after laparoscopic (TEP) and open (Lichtenstein) inguinal hernia repair: a randomized, multicenter trial with 5-year follow-up. Ann Surg. 2009. 249:33–38.
2. Takata MC, Duh QY. Laparoscopic inguinal hernia repair. Surg Clin North Am. 2008. 88:157–178.
3. Kingsnorth AN, Wright D, Porter CS, Robertson G. Prolene Hernia System compared with Lichtenstein patch: a randomised double blind study of short-term and mediumterm outcomes in primary inguinal hernia repair. Hernia. 2002. 6:113–119.
4. Gilbert AI, Graham MF, Voigt WJ. A bilayer patch device for inguinal hernia repair. Hernia. 1999. 3:161–166.
5. Hallén M, Bergenfelz A, Westerdahl J. Laparoscopic extraperitoneal inguinal hernia repair versus open mesh repair: long-term follow-up of a randomized controlled trial. Surgery. 2008. 143:313–317.
6. The MRC Laparoscopic Groin Hernia Trial Group. Laparoscopic versus open repair of groin hernia: a randomised comparison. Lancet. 1999. 354:185–190.
7. Vidović D, Kirac I, Glavan E, Filipović-Cugura J, Ledinsky M, Bekavac-Beslin M. Laparoscopic totally extraperitoneal hernia repair versus open Lichtenstein hernia repair: results and complications. J Laparoendosc Adv Surg Tech A. 2007. 17:585–590.
8. Bassini E. Nuovo metodo per la cura radicale hernia inguinale. Atti Conger Assoc Med. 1887. 2:179.
9. Lichtenstein IL, Shulman AG. Ambulatory outpatient hernia surgery. Including a new concept, introducing tension-free repair. Int Surg. 1986. 71:1–4.
10. Awad SS, Fagan SP. Current approaches to inguinal hernia repair. Am J Surg. 2004. 188:6A Suppl. 9S–16S.
11. McCormack K, Scott NW, Go PM, Ross S, Grant AM. EU Hernia Trialists Collaboration. Laparoscopic techniques versus open techniques for inguinal hernia repair. Cochrane Database Syst Rev. 2003. (1):CD001785.
12. Kingsley D, Vogt DM, Nelson MT, Curet MJ, Pitcher DE. Laparoscopic intraperitoneal onlay inguinal herniorrhaphy. Am J Surg. 1998. 176:548–553.
13. Khoury N. A randomized prospective controlled trial of laparoscopic extraperitoneal hernia repair and mesh-plug hernioplasty: a study of 315 cases. J Laparoendosc Adv Surg Tech A. 1998. 8:367–372.
14. Chung RS, Rowland DY. Meta-analyses of randomized controlled trials of laparoscopic vs conventional inguinal hernia repairs. Surg Endosc. 1999. 13:689–694.
15. Lal P, Kajla RK, Chander J, Saha R, Ramteke VK. Randomized controlled study of laparoscopic total extraperitoneal versus open Lichtenstein inguinal hernia repair. Surg Endosc. 2003. 17:850–856.
16. Myers E, Browne KM, Kavanagh DO, Hurley M. Laparoscopic (TEP) versus Lichtenstein inguinal hernia repair: a comparison of quality-of-life outcomes. World J Surg. 2010. 34:3059–3064.
17. Blinman T. Incisions do not simply sum. Surg Endosc. 2010. 24:1746–1751.
18. Lau H, Lee F. Seroma following endoscopic extraperitoneal inguinal hernioplasty. Surg Endosc. 2003. 17:1773–1777.
19. Choi YY, Kim Z, Hur KY. Swelling after laparoscopic total extraperitoneal repair of inguinal hernias: review of one surgeon's experience in 1,065 cases. World J Surg. 2011. 35:43–46.




 ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download