Abstract
Parathyroid carcinoma is a rare disease in pediatric patients. We present a case of a 13-year-old girl who presented to the Thyroid Department for an asymptomatic palpable neck mass for 1 year. The high levels of calcium, ionized calcium, and parathyroid hormone level along with parathyroid scintigraphy studies suggested primary hyperparathyroidism. Parathyroid carcinoma was confirmed by biopsy and pathologic examination after resection. Six months postoperatively, persistent hypercalcemia and multiple lung metastases were found on computed tomography. Bilateral lung wedge resection was performed. En bloc resection for primary parathyroid carcinoma and aggressive resection of metastatic disease is the most effective treatment to control hypercalcemia.
Parathyroid carcinoma is a very rare cause of primary hyperparathyroidism in children. In adults, the incidence is 1 to 5% [1,2], but in children, the incidence is not exactly known. Several articles have reported sporadic cases of parathyroid carcinoma occurring in pediatric patients [2-7]. This patient is the eighth reported case of parathyroid carcinoma occurring in a child under the age of 16 years.
A previously healthy 13-year-old girl was admitted to our Thyroid Department for an asymptomatic palpable thyroid mass. There was no family history of multiple endocrine neoplasia. A 4 cm hard mass was palpable in the right lobe of the thyroid gland.
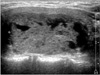
Her total serum calcium was 12.0 mg/dL (normal, 7.8 to 10 mg/dL), ionized calcium 1.52 mM/L (normal, 0.96 to 1.4 mM/L), phosphorus 2.6 mg/dL (normal, 2.9 to 4.3 mg/dL), alkaline phosphatase 2,700 IU/L (normal, 25 to 100 IU/L), intact parathyroid hormone (iPTH) level was 8,368 pg/mL (normal, 15 to 65 pg/mL). Ultrasonography of the neck showed a 4 cm multifocal cystic mass in the right thyroid gland (Fig. 1). On 99mTc-sestamibi scintigraphy, an increased uptake in the right lobe of the thyroid gland was found. Kidneys, ureters, and bladder X-rays were unremakable. All the growth plates were closed on hand radiograph. Bone mineral density showed severe osteoporosis (T score, -4.17). She was subsequently diagnosed with primary hyperparathyroidism.
During neck exploration, a 35 × 30 × 20 mm firm oval tumor was found behind and adherent to the right lobe of the thyroid gland. The contralateral parathyroid gland appeared normal. An en bloc resection of the tumor, along the right lobe of the thyroid gland was performed and the central lymph node was removed. The tumor weighed 22 g. On section it appeared grayish-yellow while histologically there were capsular, vascular and perineural invasion (Fig. 2). No tumor was present in the one regional lymph node. The findings were consistent with parathyroid carcinoma.
The patient underwent a chest computed tomography (CT) scan to evaluate for metastasis. On chest CT scan, multiple scattered subpleural nodules in both lower lung lobes were found and we considered them to be benign nodules such as an inflammatory granuloma rather than metastases.
The patient recovered without any problems. The total serum calcium and iPTH levels decreased to 8.4 mg/dL and 49.48 pg/mL on the first postoperative day, and was 9.9 mg/dL, 70.99 pg/mL two weeks, respectively. Six months postoperatively, her calcium and parathyroid hormone levels increased to 9.7 mg/dL and 297.8 pg/mL, respectively. On chest CT scan, 7 small well-defined nodules suspicious for hematogenous parathyroid carcinoma metastases appeared with increasing size bilaterally compared to her previous CT scan (Fig. 3). Bilateral lung wedge resection was performed by a thoracic surgeon and 8 metastatic nodules were removed. Histopathologic examination confirmed the diagnosis of metastatic parathyroid carcinoma. Six months later, her CT scan showed new multiple metastatic nodules in both lungs. Four years later, her calcium and parathyroid hormone levels increased to 12.4 mg/dL and 191.5 pg/mL. Bisphosphonates were used to control hypercalcemia, but improvement in bone mineral density was noted with no other symptoms present.
Parathyroid carcinoma is a very rare disease, especially in pediatrics. It usually occurs in middle-aged individuals during their third through sixth decades of life. Until now, only 6 cases have been reported of parathyroid carcinoma occurring within the age range of 8 to 15 years [2-7]. The clinical manifestations of parathyroid carcinoma in pediatric patients include palpable neck mass, bone pain, weakness, pancreatitis, malaise, polyuria, polydipsia, nausea, and vomiting. A common clinical manifestation among the reported patients was a palpable neck mass, as seen in our patient. Although there was severe osteoporosis with hypercalcemia in our patient, she remained asymptomatic. Most patients reported had severe hypercalcemia, with total serum calcium levels greater than 13 mg/dL without metastasis. Although there were bilateral lung metastases, in our patient, the total calcium level only mildly increased, but markedly elevated levels of PTH and alkaline phosphatase were seen. A palpable neck mass with hypercalcemia and markedly elevated levels of PTH in pediatric patients should raise concern for parathyroid carcinoma. It is difficult to differentiate between parathyroid adenoma and parathyroid carcinoma preoperatively. Parathyroid carcinoma is normally confirmed by histopathologic examination after operation. The histologic criteria for parathyroid carcinoma includes a trabecular pattern, mitotic figures, and capsular and blood vessel invasion [3]. Since it is usually not diagnosed preoperatively, it is important that parathyroid carcinoma be considered intraoperatively when the tumor adheres to surrounding structures, including the thyroid gland, strap muscles, and the recurrent laryngeal nerve [8,9]. If it is suspicious, aggressive treatment should be considered. Surgery is the most important treatment for parathyroid carcinoma. En bloc resection with ipsilateral thyroid lobectomy, avoiding rupture of the tumor capsule and spillage of tumor cell, at the first operation is the only curative treatment, and aggressive initial treatment is important to reduce local recurrence and improve the prognosis [2]. Considering that there have been several reports of metastasis and recurrence after operation, total calcium and iPTH levels should be monitored frequently. In our patient, the lung nodule on chest CT scan was considered to be a benign nodule because of normalization of total calcium and iPTH after operation. However, after 6 months, metastatic parathyroid carcinoma was suspected because of increased total calcium and iPTH levels with increased nodule size on follow-up CT scan. Metastatic parathyroid carcinoma was confirmed after bilateral lung wedge resection. Recurrence and systemic metastases occurs in up to 52% of patients with parathyroid carcinoma [8]. Like our patient's case, the lung is the most frequent site of metastases [8] while metastases to the bone, liver and brain can also occur [3,8]. When metastases are found, metastasectomy is recommended to reduce hypercalcemia because severe hypercalcemia and its metabolic complications are associated with increased mortality [2]. Since the growth rate of parathyroid carcinoma is slow, repeated resection of metastatic carcinoma is recommended. Chemotherapeutic agents, adjuvant radiotherapy and medical management, including calcitonin, mithramycin, and bisphosphonates, may be used for patients with uncontrollable hypercalcemia with unresectable or widespread metastatic disease. However, these treatment have little efficacy in parathyroid carcinoma [9,10].
In conclusion, parathyroid carcinoma is an infrequent disease in pediatric patients. Preoperatively, if there is severe hypercalcemia, elevated parathyroid hormone levels and palpable neck mass in a pediatric patient, parathyroid carcinoma should be suspected. En bloc resection of a primary parathyroid carcinoma is the initial treatment of choice. Hypercalcemia related metabolic complications are associated with increased mortality. Even if metastasis or recurrence is detected, aggressive resection of the metastatic parathyroid carcinoma is the most effective treatment to control hypercalcemia and improve survival.
Figures and Tables
References
1. van Heerden JA, Weiland LH, ReMine WH, Walls JT, Purnell DC. Cancer of the parathyroid glands. Arch Surg. 1979. 114:475–480.
2. Fujimoto Y, Obara T, Ito Y, Kanazawa K, Aiyoshi Y, Nobori M. Surgical treatment of ten cases of parathyroid carcinoma: importance of an initial en bloc tumor resection. World J Surg. 1984. 8:392–400.
3. Schantz A, Castleman B. Parathyroid carcinoma: a study of 70 cases. Cancer. 1973. 31:600–605.
4. Young TO, Saltzstein EC, Boman DA. Parathyroid carcinoma in a child: unusual presentation with seizures. J Pediatr Surg. 1984. 19:194–196.
5. McHenry CR, Rosen IB, Walfish PG, Cooter N. Parathyroid crisis of unusual features in a child. Cancer. 1993. 71:1923–1927.
6. Meier DE, Snyder WH 3rd, Dickson BA, Margraf LR, Guzzetta PC Jr. Parathyroid carcinoma in a child. J Pediatr Surg. 1999. 34:606–608.
7. Hamill J, Maoate K, Beasley SW, Corbett R, Evans J. Familial parathyroid carcinoma in a child. J Paediatr Child Health. 2002. 38:314–317.
8. Holmes EC, Morton DL, Ketcham AS. Parathyroid carcinoma: a collective review. Ann Surg. 1969. 169:631–640.
9. Shane E. Clinical review 122: Parathyroid carcinoma. J Clin Endocrinol Metab. 2001. 86:485–493.
10. Bukowski RM, Sheeler L, Cunningham J, Esselstyn C. Successful combination chemotherapy for metastatic parathyroid carcinoma. Arch Intern Med. 1984. 144:399–400.




 ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download