Abstract
Purpose
Most outcome studies of bypass surgery are limited to five years of follow-up. However, as human life expectancy has increased, analyses of more long-term outcomes are needed. The aim of this study is to evaluate 10-year outcomes of anatomical bypasses in aortoiliac occlusive disease.
Methods
From 1996 to 2009, 92 patients (82 males and 10 females) underwent aortic anatomical bypasses to treat aortoiliac occlusive disease at Samsung Medical Center. The patients were reviewed retrospectively. Kaplan-Meier survival analyses were performed using PASW ver. 18.0 (IBM Co).
Results
A total of 72 patients (78.3%) underwent aorto-femoral bypasses (uni- or bi-femoral), 15 patients (16.3%) underwent aorto-iliac bypasses (uni- or bi-iliac), and 5 patients (5.4%) underwent aorto-iliac and aorto-femoral bypasses. The overall primary patency rates of the 92 patients were 86.2% over 5 years and 77.6% over 10 years. The 10-year limb salvage rate and overall survival rate were 97.7% and 91.7%, respectively.
Aortoiliac occlusive disease is a relatively rare artery occlusive disease compared to infrainguinal arterial occlusive disease [1]. Leriche and Morel [2] first described this disease in 1948. The main treatment is surgical revascularization. In the past, endarterectomy was the only treatment of choice, but with the development of artificial vascular graft materials, anatomical bypass graft surgery has now become common. Axillo-femoral bypass should be considered in patients at high risk for laparotomy surgery or in whom the aortic approach is difficult due to previous abdominal surgery [3]. Endovascular treatment for atherosclerotic occlusive disease has recently emerged as a non-surgical option, but this procedure may be applied in relatively few patients. Thus, aorto-iliac bypass remains the most popular treatment for aortoiliac occlusive disease.
Ten-year long-term outcomes of this disease are rarely reported in the literature [4]. The aim of this study is to evaluate the 10-year long-term outcomes of anatomical bypass in aortoiliac occlusive disease.
From 1996 to 2009, 111 patients were surgically treated for aortoiliac occlusive disease at Samsung Medical Center. Of this group, 92 patients underwent aortic anatomical bypasses, including 82 male and 10 female patients. Nineteen patients who underwent extra-anatomical bypasses were excluded from this study. Types of prosthetic graft were selected according to surgeon preference. Patient charts were reviewed retrospectively. All patients were examined for patency of graft by duplex ultrasound at 1, 3, and 6 months postoperatively. Thereafter, duplex scan and/or CT angiography were undertaken every 6 to 12 months.
Statistical analyses were performed using PASW ver. 18.0 (IBM Co., Armonk, NY, USA). The patency rates of grafts, limb salvage rates and overall survival rates were analyzed using Kaplan-Meier survival analysis.
The median follow-up period was 41.5 months (range, 1 to 155.8 months). Twenty-eight patients were receiving medical therapy due to co-existing coronary heart disease, nine patients had coronary artery stenting, and three patients received coronary artery bypass grafts (CABGs) before the anatomical bypass surgery. Eight patients had undergone distal lower extremity bypass surgeries and two patients had undergone distal limb amputations due to ischemic tissue loss (Table 1).
The indications for bypass surgery were clinically classified into three categories. There were 72 patients with moderate to severe claudication, 15 patients with ischemic tissue loss, and 5 patients with rest pain (Table 1).
Seventy-three patients had infrarenal occlusions and 19 patients had juxtarenal occlusions. The surgical approach was transperitoneal in 90 patients and retroperitoneal in 2 patients. Median hospital stays were 13 days, and there were no immediate postoperative mortalities. The bypasses were aorto-femoral (uni- or bi-femoral) in 72 patients (78.3%), aorto-iliac (uni- or bi-iliac) in 15 patients (16.3%), and aorto-iliac and aorto-femoral in 5 patients (5.4%) (Table 2).
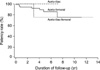
In the aorto-femoral bypass cases, the 5-year and 10-year primary patency rate were 85.3% and 74.6%, respectively. In the aorto-iliac bypass cases, the 5-year and 10-year primary patency rates were both 100%. In the aorto-iliac and aorto-femoral bypass cases, the 5-year and 10-year primary patency rates were both 75.0%. There were no significant differences among the three groups (P = 0.512) (Fig. 1).
Two graft materials were used, polytetrafluoroethylene (PTFE) in 79 (85.9%) and Dacron in 13 (14.1%). The 5-year primary patency rates for PTFE and Dacron were 86.4% and 82.1%, respectively, and the 10-year primary patency rates were 75.6% and 82.1%, respectively. However, these differences were not significant (P = 0.698) (Fig. 2).
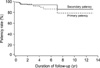
During follow-up, grafts were occluded in nine patients. Recurrent symptoms were 4 patients with claudication, 3 rest pain, 1 paralysis and 1 skin color change in foot. There were 8 procedures to rescue of graft-failure; 2 thrombolysis, 2 stent insertion, 1 thrombectomy with patch angioplasty, 2 thrombectomy with bypass graft and 1 interposition graft. In a patient undergone aorto-bifemoral bypass and below the knee amputation in right leg, conservative management was performed due to long segmental occlusion from descending thoracic aorta to left femoral artery. The 5-year and 10-year overall primary patency rates were 86.2% and 77.6%, respectively, and the secondary patency rates at 5 years and 10 years were 91.6% and 83.3%, respectively (Fig. 3). Statistical analysis of the variables such as age, gender and comorbidities failed to detect predictors of graft failure. Two patients underwent lower extremity amputations after bypass surgery. The 10-year overall limb salvage rate was therefore 97.7% (Fig. 4).
Four patients died due to acute myocardial infarction (one patient) or malignancy (three patients: stomach cancer, lung cancer, and pancreatic cancer). The 10-year overall survival rate was 91.7% (Fig. 5).
The management options for aortoiliac occlusive disease are surgical or non-surgical management. The surgical treatment of aortoiliac occlusive disease can be divided into two categories, direct anatomical bypass vs. extra-anatomical bypass [5]. Direct anatomical bypasses are aorto-iliac bypasses or aorto-femoral bypasses, while extra-anatomical bypasses are axillo-femoral bypasses. Some high-risk patients underwent extra-anatomical bypass surgeries (e.g., axillo-femoral bypass) or endovascular revascularization [3,6]. Because patency outcomes after extra-anatomical bypass were less favorable than after anatomical bypass, the treatment of choice in aortoiliac occlusive disease is anatomical bypass surgery [7]. Recently, a totally laparoscopic approach and robotic-assisted laparoscopic approach were used for the treatment of aortoiliac occlusive disease, but the indications for laparoscopy are limited [8,9]. In any case, this study analyzed the long-term outcomes of direct anatomical bypasses alone, not in comparison with extra-anatomical bypass surgery.
The primary patency rates of aortic bypass graft reconstruction are good compared to infrainguinal arterial bypass graft reconstruction [4]. We observed good results (5-year primary patency rate of 86.2% and 10-year primary patency rate of 77.6%) in the present study, but these outcomes were not compared directly to infrainguinal leg bypass outcomes.
We observed no significant differences in patency rates between PTFE and Dacron in this study (P = 0.698). This result agrees with previous studies that did not detect significant differences between artificial graft materials in patients who underwent aorto-femoral bypass and femoropopliteal bypass [10,11].
Some patients experienced symptoms of sexual dysfunction due to aortoiliac occlusive disease [12-14]. Improvement of sexual function is expected after revascularization. However, we did not evaluate pre- and post-operative male sexual function in our study. Due to the limitations of retrospective study design, further evaluation of sexual function is needed.
The most common cause of death in peripheral artery occlusive disease is cardiovascular disease [15]. In our study, 28 patients (30.4%) also had coronary artery disease, but only one patient died of acute myocardial infarction. This low rate of death was probably due to coronary intervention and the management of coronary artery disease.
In conclusion, most outcome studies of bypass surgery are limited to five years of follow-up. However, as human life expectancy has increased, analyses of more long-term outcomes are needed. A total of 72 patients (78.3%) underwent aorto-femoral bypasses (uni- or bi-femoral), 15 patients (16.3%) underwent aorto-iliac bypasses (uni- or bi-iliac), and 5 patients (5.4%) underwent aorto-iliac and aorto-femoral bypasses. The overall primary patency rates of 92 patients were 86.2% over 5 years and 77.6% over 10 years. The 10-year limb salvage rate and overall survival rate were 97.7% and 91.7%.
Figures and Tables
References
1. Szilagyi DE, Elliott JP Jr, Smith RF, Reddy DJ, McPharlin M. A thirty-year survey of the reconstructive surgical treatment of aortoiliac occlusive disease. J Vasc Surg. 1986. 3:421–436.
2. Leriche R, Morel A. The syndrome of thrombotic obliteration of the aortic bifurcation. Ann Surg. 1948. 127:193–206.
3. Park UJ, Kim DI. Thromoboagiitis obliterans (TAO). Int J Stem Cells. 2010. 3:1–7.
4. de Vries SO, Hunink MG. Results of aortic bifurcation grafts for aortoiliac occlusive disease: a meta-analysis. J Vasc Surg. 1997. 26:558–569.
5. Brewster DC. Current controversies in the management of aortoiliac occlusive disease. J Vasc Surg. 1997. 25:365–379.
6. Kashyap VS, Pavkov ML, Bena JF, Sarac TP, O'Hara PJ, Lyden SP, et al. The management of severe aortoiliac occlusive disease: endovascular therapy rivals open reconstruction. J Vasc Surg. 2008. 48:1451–1457.e3.
7. Kim IH, Kim DI, Huh SH, Lee BB, Kim DK, Do YS, et al. Clinical experiences of the arterial bypass in aortoiliac occlusive disease. J Korean Surg Soc. 2001. 61:600–603.
8. Di Centa I, Coggia M, Cerceau P, Javerliat I, Alfonsi P, Beauchet A, et al. Total laparoscopic aortobifemoral bypass: short- and middle-term results. Ann Vasc Surg. 2008. 22:227–232.
9. Novotny T, Dvorak M, Staffa R. The learning curve of robot-assisted laparoscopic aortofemoral bypass grafting for aortoiliac occlusive disease. J Vasc Surg. 2011. 53:414–420.
10. Davidovic L, Vasic D, Maksimovic R, Kostic D, Markovic D, Markovic M. Aortobifemoral grafting: factors influencing long-term results. Vascular. 2004. 12:171–178.
11. Takagi H, Goto SN, Matsui M, Manabe H, Umemoto T. A contemporary meta-analysis of Dacron versus polytetrafluoroethylene grafts for femoropopliteal bypass grafting. J Vasc Surg. 2010. 52:232–236.
12. Miles JR Jr, Miles DG, Johnson G Jr. Aortoiliac operations and sexual dysfunction. Arch Surg. 1982. 117:1177–1181.
13. Cormio L, Edgren J, Lepantalo M, Lindfors O, Nisen H, Saarinen O, et al. Aortofemoral surgery and sexual function. Eur J Vasc Endovasc Surg. 1996. 11:453–457.
14. Flanigan DP, Schuler JJ, Keifer T, Schwartz JA, Lim LT. Elimination of iatrogenic impotence and improvement of sexual function after aortoiliac revascularization. Arch Surg. 1982. 117:544–550.
15. Hertzer NR, Beven EG, Young JR, O'Hara PJ, Ruschhaupt WF 3rd, Graor RA, et al. Coronary artery disease in peripheral vascular patients: a classification of 1000 coronary angiograms and results of surgical management. Ann Surg. 1984. 199:223–233.




 ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download