Abstract
Purpose
An inflamed appendix can be removed either openly (open appendectomy [OA]) or laparoscopically (laparoscopic appendectomy [LA]). Surgical-site infection (SSI) is a representative healthcare-associated infection and can impose serious economic burdens on patients as well as affect morbidity and mortality rates. The aim of this study was to compare LA with OA in terms of SSI.
Methods
The medical records of 749 patients (420 males; mean age, 33 years) who underwent appendectomy (OA, 431; LA, 318) between September 1, 2008 and April 29, 2010 were retrospectively reviewed for demographic and pathologic characteristics, recovery of bowel movement, length of hospital stay, and postoperative complications.
Results
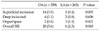
The frequency of purulent/gangrenous or perforated appendicitis was not significantly different between LA and OA groups (83% [263/318 cases] vs. 83% [359/431 cases], P = 0.183). The time to first flatus after surgery was not significantly different between the two groups (1.38 ± 1.07 days for LA, 1.33 ± 0.90 days for OA, P = 0.444), but the length of hospital stay was significantly shorter in LA group than in OA group (3.37 ± 0.12 days vs. 3.83 ± 0.12 days, P = 0.006). The frequency of overall SSI was not significantly different between the two groups (2.8% for LA, 4.6% for OA, P = 0.204), but that of superficial incisional SSI was significantly lower in LA group (0.6% vs. 3.9%, P = 0.016).
Open appendectomy (OA), which was described first by McBurney [1] in 1894, has been accepted as the gold standard of appendectomy for around 100 years. However, since its introduction by Semm [2] in 1983, laparoscopic appendectomy (LA) has been conducted more frequently than OA due to its advantages of being minimally invasive [2-4]. In particular, more attention has been paid to recent remarkable innovative development and improvement in laparoscopic equipments, instruments and techniques. Laparoscopic surgery, as mentioned in many studies, allows for safe and aesthetic operations [3-5] and can shorten the length of hospital stay, accelerate postoperative recovery and produce less pain [6,7]. However, LA may necessitate higher medical costs due to the use of specialized equipments and instruments and may show a higher possibility of intra-abdominal abscess, especially in severe appendicitis, such as perforated appendicitis [8-12]. Surgicalsite infection (SSI) is known to be a representative healthcare-associated infection and may impose serious economic burdens on patients as well as increase morbidity and mortality rates [13-15]. The present study compared and analyzed LA and OA especially in terms of SSI.
This present study included 749 cases diagnosed as appendicitis and operated on at Seoul National University Hospital (n = 191) and Seoul National University Bundang Hospital (n = 558) from September 1, 2008 to April 29, 2010. The subjects consisted of 420 males and 329 females, and their mean age was 33.32 ± 20.80 years (range, 2 to 92 years).
OA was performed through right lower quadrant transverse muscle-splitting incision. The thread ties were placed on the base of the appendix. The tied-off appendiceal stump was dunk in again with purse-string suture. For LA, three ports were used. One 10-mm port for laparoscope entered at the inferior margin of umbilicus with either a vertical or semicircular transverse incision. Two additional 5-mm ports entered at the left lower quadrant and at the suprapubic area. Mesoappendiceal tissue was dissected and divided with monopolar electrocautery or ultrasonic scissor. Before transection of appendix, stump was doubly ligated with endoloops as an easy, safe and cost-effective procedure [16]. Transected appendix was retrieved via umbilical port. And the surgeons decided cautiously whether or not to insert a Jackson-Pratt drain bag in severe forms of appendicitis, such as suppurative, gangrenous, or perforated appendicitis.
The severity of illness (hyperemia, suppuration, gangrene/perforation, or abscess formation) was determined through the final pathologic reports. Each patient's medical records were reviewed in terms of operation time, time to the start of a normal diet, length of hospital stay, postoperative complications (wound, abscess, ileus, etc), and readmission within 30 days of surgery.
Statistical analyses were performed using SPSS ver. 17.0 (SPSS Inc., Chicago, IL, USA), and Student's t-test or Pearson's chi-square test was used. A P-value of <0.05 was considered to be statistically significant. SSI was defined according to the Center of Disease Control guideline. Fascia abscess and intra-abdominal abscess were reclassified as deep incisional SSI and organ/space SSI, respectively [17].
Appendectomies were performed openly in 431 patients (OA group) and laparoscopically in 318 patients (LA group). The mean age was younger and body mass index (BMI) was higher significantly in the LA group than in the OA group, but the other demographic and pathologic parameters were not significantly different between the two groups (Table 1). The mean operation time was longer by 6 minutes in the LA group than in the OA group (65.93 ± 31.55 minutes vs. 60.14 ± 33.55 minutes, P = 0.017). Time to the first flatus after operation was not significantly different between the two groups, but the length of hospital stay was significantly shorter in the LA group than in the OA group (3.37 ± 0.12 days vs. 3.83 ± 0.12 days, P = 0.006). Postoperative ileus developed in 3 cases (0.7%) in the LA group and 7 cases (1.9%) in the OA group, but the difference was not statistically significant (P = 0.422) (Table 2). The overall SSI rate was not different between the two groups (2.8% for the OA group vs. 4.6% for the LA group, respectively, P=0.204), but the superficial SSI rate was significantly lower in the LA group (3.2% vs. 0.6%, P = 0.016) (Table 3). In addition, the difference in the superficial SSI rate was more significant in severe forms of appendicitis, such as suppurative, gangrenous or perforated appendicitis (Table 4).
The patients were re-classified by the symptoms or signs of the patients, radiologic and operative findings into 1) minimal or localized peritonitis group (n = 682) and 2) diffuse peritonitis group (n = 67). The ratio of patients with diffuse peritonitis was not significantly different between LA and OA (9.1% [29/318 cases] in LA group vs. 8.8% [38/431 cases] in OA group, P = 0.886). And also in mild or localized peritonitis group, the rate of SSI was not significantly different between LA and OA (2.8% [8/289 cases] in LA group vs. 3.1% [12/393 cases] in OA group, P = 0.827). However, in diffuse peritonitis group, the rate of SSI was significantly higher in OA group (3.4% [1/29 cases] in LA group vs. 21.1% [8/38 cases] in OA group, P = 0.036).
Readmission within 30 days of surgery was observed in 2 cases (0.6%) in the LA group and 9 cases (2.1%) in the OA group, but the difference was not statistically significant. Of the 9 patients in the OA group, 2 were hospitalized due to ileus and 7 due to SSI, while the 2 patients in the LA group were hospitalized due to SSI.
Laparoscopic surgery allows for safe and aesthetic operation [3-5] and it is also known to accelerate postoperative recovery and to produce less pain [6]. In the current study, the time to the first flatus after surgery was not significantly different between the two groups. The reason for this may be that the appendectomy is such a minor operative procedure that the recovery of gastrointestinal motility is not significantly affected. However, the length of hospital stay was significantly shorter in the LA group.
The mean age of the patients was significantly younger in the LA group than in the OA group in this study. This may be explained by the fact that young people are usually more concerned about aesthetic outcomes. The frequency of LA was significantly higher in females aged <25 years than in those aged ≥25 years (19% [60/318 cases] vs. 12% [51/431 cases], P = 0.007), which suggests that young patients favored the minimally invasive operation.
Operation time was significantly longer in the LA group than in the OA group. Khan et al. [18] reported that the median operation time was 51.3 minutes in the LA group and 40.6 minutes in the OA group. Bennett et al. [5] showed similar results based on a meta-analysis of 22 studies. The longer operation time in the LA group than in the OA group may be explained by the additional time required for the preparation of the laparoscopic equipment, and a steep learning curve for the laparoscopic procedure when performed by a novice. If a novice overcomes the learning curve and becomes familiar with the laparoscopic procedure, the operation time of LA can be shortened.
BMI was significantly higher in the LA group than in the OA group. Obesity is known to be a risk factor for surgical-site infection and BMI is used to define obesity. Higher BMI tends to correlate with higher SSI rate [19]. However, in the present study, the overall SSI rate was not significantly different between the two groups, and the superficial SSI rate was rather significantly lower in the LA group. The difference in the superficial SSI rate was more evident in severe forms of appendicitis, such as suppurative, gangrenous, or perforated appendicitis. SSI may occur anywhere from the skin to the organ/space in both the LA and OA groups. However, the superficial SSI, which only involves the skin or subcutaneous tissue, is rare in the LA group because of the unique nature of the laparoscopic procedure. Shalak et al. [8] mentioned systematic extraction of grossly infected appendices with a bag. The extraction bag (Lap-bag, Sejong Medical, Paju, Korea), which was used in all cases in the LA group, allows the surgical wounds to avoid direct contact with the infected appendices or inflamed tissues around the appendices. On the other hand, the wounds are vulnerable to the infections or inflammations in the OA group. When laparoscopic surgeons manipulate lesions inside the abdominal cavity, the bag decreases the risk of superficial SSI by keeping the skin or subcutaneous tissue a safe distance from the lesions. The protection may be eminent in severe forms of appendicitis, such as suppurative, gangrenous, or perforated appendicitis.
However, organ/space SSI incidence was higher in the LA group than in the OA group (3 cases [1.1%] vs. 2 cases [0.6%]), although the difference was not statistically significant. This finding leads to a concern about the possibility of complications of LA such as intra-abdominal abscess, as mentioned in previous studies [9,10,20,21]. Markides et al. [22] also emphasized the surgeon's discretion and laparoscopic experience in complicated appendicitis, while concluding no difference with regard to intra-abdominal abscess complication rates (level 3a evidence) in their systematic review and meta-analysis. Therefore, when LA is conducted, the surrounding area of the pelvis should be carefully explored. Abscess should be sufficiently aspirated or the insertion of drains should be considered.
The current study has some limitations in that the enrolled patients were not randomized to the OA and LA groups. Our patients underwent operation by several surgeons with varying degrees of surgical skills. To remove these limitations, well-designed randomized controlled trials with a larger number of patients should be carried out. However, such trials would be practically infeasible due to the continued growth of the popularity of LA as mentioned previously [18].
Figures and Tables
References
1. McBurney C. IV. The incision made in the abdominal wall in cases of appendicitis, with a description of a new method of operating. Ann Surg. 1894. 20:38–43.
2. Semm K. Endoscopic appendectomy. Endoscopy. 1983. 15:59–64.
3. Moberg AC, Berndsen F, Palmquist I, Petersson U, Resch T, Montgomery A. Randomized clinical trial of laparoscopic versus open appendicectomy for confirmed appendicitis. Br J Surg. 2005. 92:298–304.
4. Sauerland S, Lefering R, Neugebauer EA. Laparoscopic versus open surgery for suspected appendicitis. Cochrane Database Syst Rev. 2004. (4):CD001546.
5. Bennett J, Boddy A, Rhodes M. Choice of approach for appendicectomy: a meta-analysis of open versus laparoscopic appendicectomy. Surg Laparosc Endosc Percutan Tech. 2007. 17:245–255.
6. Aziz O, Athanasiou T, Tekkis PP, Purkayastha S, Haddow J, Malinovski V, et al. Laparoscopic versus open appendectomy in children: a meta-analysis. Ann Surg. 2006. 243:17–27.
7. Kim CB, Kim MS, Hong JH, Lee HY, Yu SH. Is laparoscopic appendectomy useful for the treatment of acute appendicitis in Korea? A meta-analysis. Yonsei Med J. 2004. 45:7–16.
8. Shalak F, Almulhim SI, Ghantous S, Yazbeck S. Laparoscopic appendectomy: burden or benefit? A single-center experience. J Laparoendosc Adv Surg Tech A. 2009. 19:427–429.
9. Hart R, Rajgopal C, Plewes A, Sweeney J, Davies W, Gray D, et al. Laparoscopic versus open appendectomy: a prospective randomized trial of 81 patients. Can J Surg. 1996. 39:457–462.
10. Minné L, Varner D, Burnell A, Ratzer E, Clark J, Haun W. Laparoscopic vs open appendectomy. Prospective randomized study of outcomes. Arch Surg. 1997. 132:708–711.
11. Ingraham AM, Cohen ME, Bilimoria KY, Pritts TA, Ko CY, Esposito TJ. Comparison of outcomes after laparoscopic versus open appendectomy for acute appendicitis at 222 ACS NSQIP hospitals. Surgery. 2010. 148:625–635.
12. Tuggle KR, Ortega G, Bolorunduro OB, Oyetunji TA, Alexander R, Turner PL, et al. Laparoscopic versus open appendectomy in complicated appendicitis: a review of the NSQIP database. J Surg Res. 2010. 163:225–228.
13. Varela JE, Wilson SE, Nguyen NT. Laparoscopic surgery significantly reduces surgical-site infections compared with open surgery. Surg Endosc. 2010. 24:270–276.
14. Kirkland KB, Briggs JP, Trivette SL, Wilkinson WE, Sexton DJ. The impact of surgical-site infections in the 1990s: attributable mortality, excess length of hospitalization, and extra costs. Infect Control Hosp Epidemiol. 1999. 20:725–730.
15. Herwaldt LA, Cullen JJ, Scholz D, French P, Zimmerman MB, Pfaller MA, et al. A prospective study of outcomes, healthcare resource utilization, and costs associated with postoperative nosocomial infections. Infect Control Hosp Epidemiol. 2006. 27:1291–1298.
16. Sahm M, Kube R, Schmidt S, Ritter C, Pross M, Lippert H. Current analysis of endoloops in appendiceal stump closure. Surg Endosc. 2011. 25:124–129.
17. Mangram AJ, Horan TC, Pearson ML, Silver LC, Jarvis WR. Guideline for Prevention of Surgical Site Infection, 1999. Centers for Disease Control and Prevention (CDC) Hospital Infection Control Practices Advisory Committee. Am J Infect Control. 1999. 27:97–132.
18. Khan MN, Fayyad T, Cecil TD, Moran BJ. Laparoscopic versus open appendectomy: the risk of postoperative infectious complications. JSLS. 2007. 11:363–367.
19. Cantürk Z, Cantürk NZ, Cetinarslan B, Utkan NZ, Tarkun I. Nosocomial infections and obesity in surgical patients. Obes Res. 2003. 11:769–775.
20. Guller U, Hervey S, Purves H, Muhlbaier LH, Peterson ED, Eubanks S, et al. Laparoscopic versus open appendectomy: outcomes comparison based on a large administrative database. Ann Surg. 2004. 239:43–52.
21. Golub R, Siddiqui F, Pohl D. Laparoscopic versus open appendectomy: a metaanalysis. J Am Coll Surg. 1998. 186:545–553.
22. Markides G, Subar D, Riyad K. Laparoscopic versus open appendectomy in adults with complicated appendicitis: systematic review and meta-analysis. World J Surg. 2010. 34:2026–2040.
23. Wei HB, Huang JL, Zheng ZH, Wei B, Zheng F, Qiu WS, et al. Laparoscopic versus open appendectomy: a prospective randomized comparison. Surg Endosc. 2010. 24:266–269.
24. Varlet F, Tardieu D, Limonne B, Metafiot H, Chavrier Y. Laparoscopic versus open appendectomy in children--comparative study of 403 cases. Eur J Pediatr Surg. 1994. 4:333–337.
25. Moore DE, Speroff T, Grogan E, Poulose B, Holzman MD. Cost perspectives of laparoscopic and open appendectomy. Surg Endosc. 2005. 19:374–378.




 ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download