Abstract
Purpose
Stress poses a serious risk for training surgeons since their performance and well-being in reflected in patients' health. This study focuses on measuring the stress of training surgeons and at the same time evaluates prospectively the results of an innovative program that uses alternative techniques to combat the effects of stress.
Methods
The study was a pilot randomized controlled trial, with a duration of 6 months. Participants were allocated to a control and an intervention group. Trainees then completed three questionnaires, quality of life, perceived stress scale (PSS) and job content questionnaire serving as a baseline measurement. Only the intervention group used diaphragmatic breathing and progressive muscular relaxation techniques, twice a day, for 20 minutes each, and for a total period of eight weeks. At the end of the study, the same questionnaires were completed again by both groups.
Results
The sample of the study included 28 and 32 trainees in the control and the intervention group, respectively. The Cronbach's α value for the PSS stress-measuring questionnaire was 0.772. The intervention group presented statistically significant lower values of stress (30.50, P < 0.05) in comparison to the control group (27.54).
Conclusion
The medical community, and especially surgeons, have been reluctant up to now to embrace interventional programs that go beyond the traditional use of medication in order to address stress related issues. The positive results and feedback from small studies, such as ours, can provide the driving force for further research that will give us solid, evidence-based, answers.
Surgeons in our opinion have always been an example of an individual who is determined, professional, being able to control himself under adverse circumstances and willing to work extra hours, beyond any schedule or program. These characteristics may be true for most surgeons but there is always a price to be paid. The effects of the surgical profession on trainees and consultants have only recently started to be unveiled, following an increased number of studies examining the consequences on other professional groups. Stress related problems have been the area of investigation for many scientists but surgeons were one of the last to take this matter seriously. This could explain the scarcity of published studies, even today, concerning the surgical profession and stress. Undoubtedly, stress poses a serious risk for everyone, especially training surgeons since their performance and well-being is reflected in patients' health. Even less attention has been given to programs designed to prevent and decrease the deleterious effects of stress. This study tries to measure the stress of training surgeons and at the same time implements an innovative program to combat its effects.
The study was a pilot randomized controlled trial and its duration was 4 months, from November 2010 to March 2011. The inclusion criteria included surgical trainees that worked in a public hospital in Greece and that were in their first 4 years out of the six years in total required in order to complete the Training Program of General Surgery in Greece. Exclusion criteria were the use of anti-psychotic medication, previous history of psychiatric illness, already using other relaxation techniques, and being on a psychological counseling program. After the initial approach and a thorough briefing about the study, trainees gave informed consent, being able to abandon the study at any stage. Participants were allocated to a control group and an intervention group based on a well-known and used randomization method (random integer generator). After group assignment, analytical information concerning the definition of stress, its causes and its effects on health were given. Trainees were then asked to complete three distinct questionnaires serving as a baseline measurement. The first questionnaire is a multi-purpose questionnaire designed to measure health and well-being and has been validated in the Greek population (C. Darviri). The second questionnaire is perceived stress scale (PSS), which measures stress, and the third questionnaire was the well-known job content questionnaire (JCQ), which measures job-demand and control.
The intervention group was administered with an audio CD that contained instructions on using diaphragmatic breathing and progressive muscular relaxation techniques. The suggested use was twice a day for a period of eight weeks. Compliance to the study and guidance was provided through regular telephone sessions every week. At the end of the study, all data provided in the intervention group were also given to the control group for future use.
Statistical analysis was done using IBM SPSS ver. 18.0 (IBM Co., New York, NY, USA) software. Statistical analysis was based on the t-test parametric testing of independent samples and on the non-parametric testing of Mann-Whitney. The reason for using both of the tests is that some factors satisfy the normality and homogeneity assumptions, while others don't. In order to test the normality, the one sample Klomogorov-Smirnov test was employed. A level of significance less than 0.05% was accepted as statistically significant.
In total, 100 surgical residents were approached in order to be included in the study. Thirty-eight were excluded, two of which were due to non-compliance with the inclusion criteria, and 26 trainees refused to participate. The remaining sixty-two, were randomized into two groups, thirty-two were allocated to the intervention group while thirty were allocated to the control group. Due to attrition during the course of the study, the study was completed by 28 out of the 32 trainees in the intervention group and by 24 out of 30 in the control group (Fig. 1).
There were 58 men and 4 women. The mean age was 37 years old, ranging from 30 to 45 years old. The percentage of married trainees was 47.32%, 37.50% was single, 13.39% were living with their partner and 1.79% was divorced. Almost half of the trainees (48.21%) had at least one child, with 53.70% of them saying that they have 1 child, 38.89% having two children and 3.70%, respectively, for three and four children. Most trainees were in their 4th year of residence (58.04%), with 25% being in their third year.
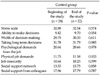
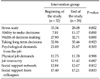
Cronbach's α coefficient of reliability for the PSS questionnaire was acceptable (0.772) and similar values were obtained for the JCQ questionnaire as illustrated in Table 1.
As is evident from Table 2, control group at the beginning and at the end of the study did not present major-statistically significant changes. The PSS stress scale revealed a value of 32.88 before and 32.54 after, with all other parameters also remaining fairly stable. On the other hand the intervention group presented a statistically significant drop in its stress levels, 28.08 from 33.34 (P < 0.05). Also, the intervention group improved significantly its ability to make decisions, 11.17 from 7.81 (P < 0.05), and the breadth of the decision making 32.71 from 27.90 (P < 0.05) (Table 3).
The psychological and physical demands of the job, job insecurity, and social and colleague support presented minor, non-statistically significant changes.
Job related stress is currently evaluated in a wide array of professions. The medical profession, especially its community, has been reluctant, until recently, to investigate in depth the phenomenon in its own backyard. The published literature, so far, indicates that stress poses a considerable risk on doctors' health [1-3]. In regards to surgeons it has already been shown that at over 50 years old, they present at least one major health related issue and that only half of them are satisfied with their job [4]. In a large study in 2001 from the University of Michigan, in 582 surgical trainees surveyed, 32% presented signs of emotional burnout and 13% suffered from depersonalization [5]. The effect of stress on cognitive abilities, performance and physical skills has been a matter of great interest as it is intimately related to patient care and well-being [6-14]. The overall impression is that although cognitive abilities remain unchanged, stress can diminish the physical skills that are indispensable in the operating theatres. Even less attention has been given to potential programs or techniques able to minimize stress related issues. The logical explanation to that comes from the fact that doctors in the first place are quite "shy" on admitting their own stress and are obviously much more reluctant in following interventional, non-pharmaceutical based programs. Individually, of course, every surgeon comes up with a strategy to decrease his/her own stress levels to the extent that this is possible [15]. A very common example of such a technique is that when confronted with an unexpected bleeding intraoperatively, experienced surgeons will simply apply pressure and take a minute to gather their thoughts and make up a new plan. This study's goal is to provide trainees with easy, drug free, techniques that can improve their stress and thus their quality of life and their professional development. Any such program needs time and consistency in order to be effective. In fact, Rowe [16], have shown in 1999 that the beneficial effects of a program designed to fight stress disappear over time if the techniques do not become a daily routine. This particular study has tried to address the stress related issues of the surgical trainees in the Greek setting. The small number of participants cannot be heavily criticized when taking into account the fact that the authors initially approached 100 trainees, which is a very considerable number in the Hellenic setting. The positive results obtained undoubtedly suffer in the light of the limited number of participants. However, the observed reduction in the levels of stress do provide a good trend of how useful such interventional programs can be.
The authors acknowledge the limitations of this study in terms of its sample size but feel that it is important to put the spotlight on a problem that has remained unexplored for many years. Hopefully, more researchers will look into the use interventional techniques such as diaphragmatic breathing and progressive muscular relaxation for the benefit of their application in the surgical community.
Figures and Tables
References
1. Buddeberg-Fischer B, Klaghofer R, Stamm M, Siegrist J, Buddeberg C. Work stress and reduced health in young physicians: prospective evidence from Swiss residents. Int Arch Occup Environ Health. 2008. 82:31–38.
2. Schmidt TS, Dembroski TM, Bluümchen G. Biological and psychological factors in cardiovascular disease. 1986. Berlin: Springer.
3. Theorell T. Berkman LF, Kawachi I, editors. Social epidemiology. Social epidemiology. 2000. New York: Oxford University Press;95–117.
4. Harms BA, Heise CP, Gould JC, Starling JR. A 25-year single institution analysis of health, practice, and fate of general surgeons. Ann Surg. 2005. 242:520–526.
5. Campbell DA Jr, Sonnad SS, Eckhauser FE, Campbell KK, Greenfield LJ. Burnout among American surgeons. Surgery. 2001. 130:696–702.
6. Bartle EJ, Sun JH, Thompson L, Light AI, McCool C, Heaton S. The effects of acute sleep deprivation during residency training. Surgery. 1988. 104:311–316.
7. Browne BJ, Van Susteren T, Onsager DR, Simpson D, Salaymeh B, Condon RE. Influence of sleep deprivation on learning among surgical house staff and medical students. Surgery. 1994. 115:604–610.
8. Deaconson TF, O'Hair DP, Levy MF, Lee MB, Schueneman AL, Codon RE. Sleep deprivation and resident performance. JAMA. 1988. 260:1721–1727.
9. Godellas CV, Huang R. Factors affecting performance on the American Board of Surgery in-training examination. Am J Surg. 2001. 181:294–296.
10. Goldman LI, McDonough MT, Rosemond GP. Stresses affecting surgical performance and learning. I. Correlation of heart rate, electrocardiogram, and operation simultaneously recorded on videotapes. J Surg Res. 1972. 12:83–86.
11. Grantcharov TP, Bardram L, Funch-Jensen P, Rosenberg J. Laparoscopic performance after one night on call in a surgical department: prospective study. BMJ. 2001. 323:1222–1223.
12. Haynes DF, Schwedler M, Dyslin DC, Rice JC, Kerstein MD. Are postoperative complications related to resident sleep deprivation? South Med J. 1995. 88:283–289.
13. Light AI, Sun JH, McCool C, Thompson L, Heaton S, Bartle EJ. The effects of acute sleep deprivation on level of resident training. Curr Surg. 1989. 46:29–30.
14. Taffinder NJ, McManus IC, Gul Y, Russell RC, Darzi A. Effect of sleep deprivation on surgeons' dexterity on laparoscopy simulator. Lancet. 1998. 352:1191.
15. Wetzel CM, Kneebone RL, Woloshynowych M, Nestel D, Moorthy K, Kidd J, et al. The effects of stress on surgical performance. Am J Surg. 2006. 191:5–10.
16. Rowe MM. Teaching health-care providers coping: results of a two-year study. J Behav Med. 1999. 22:511–527.




 ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download