Abstract
Tuberculosis primarily affecting the appendix is extremely rare and the diagnosis is difficult. Here, we report the case of a 14-year-old healthy boy presenting with right lower quadrant abdominal pain. On computed tomography, the distended appendix with 3.3 × 2.7 cm mass located at the right side of the right iliac artery was detected. There was neither bowel wall thickening nor active lung lesion. After laparoscopic appendectomy with mass excision, histopathological examination revealed chronic granulomatous inflammation, with caseous necrosis of the appendix. We made a diagnosis of primary tuberculosis of appendix and administrated anti-tuberculosis medication.
The registration system and the active vaccination since 1962 have continuously declined the incidence of tuberculosis (TB) in Korea. Despite of these efforts, the incidence of TB in Korea is high among the Organization for Economic Cooperation and Development countries. In 2009, in Korea, the reported TB cases per 100,000 were 74.3, and the actual incidence is presumed as 90 cases per 100,000 [1]. According to data from the registration center, extra pulmonary TB was 22.3% of reported TB cases in 2009 [1]. The proportion of extra pulmonary TB shows increased tendency since 2003. Of extra pulmonary cases, the primary TB of appendix is extremely rare and was reported sporadically. The reported incidence of primary TB in performed appendectomies varies from 0.1 to 3.0%, and it is 1.5 to 30% of all patients who were diagnosed with TB [2]. Herein, we report the case of a child with primary tuberculous appendicitis accompanied with mesenteric mass.
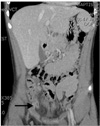
A 14 year-old boy complained of intermittent right lower quadrant abdominal pain for one day. He had no medical history and received all vaccinations, including BCG (bacille de Calmette-Guerin) vaccine, as scheduled. One month prior to admission, he started a baseball camp training in his school. He did not experience febrile sensation, weight loss or cough. On physical examination, tenderness at Mc Burney's point was noted. There was neither muscular guarding nor palpable mass. Laboratory findings showed that the white blood cell count and the C-reactive protein were within normal range. The chest X-ray didn't reveal any active lung lesion. Abdominal computed tomography revealed diffuse enlargement of the entire appendix (about 12 mm), with cystic change at the tip of the appendix (Fig. 1). Also, the abnormal calcified mass was detected on abdominal computed tomography. The 3.3 × 27 cm mass was located at the right side of the right iliac artery, inferior to the second portion of the duodenum and anterior to the right psoas muscle (Fig. 2). It was accompanied by internal necrosis and was assumed to be the lymph-node from the mesentery. There was no abnormal wall thickening of the small bowel or the colon.
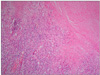
We decided to perform laparoscopic appendectomy and excision of the mesenteric mass. Under general anesthesia, the patient underwent laparoscopic exploration. We used three trocars, as follows: a 12-mm trocar at the infra umbilical portion, a 5-mm trocar at the left lower abdominal quadrant, and a 5-mm trocar at the suprapubic portion. We found no ascites. The appendix was diffusely enlarged and distended, and it showed suppurative change (Fig. 3). The stump was ligated by polydioxanone (PSD II, Ethicon Inc., Somerville, NJ, USA) endo-loop. The epiploicae of the colon showed yellowish change, with calcification. The intra-abdominal mass was protruded from the mesentery, was adjacent to the second portion of the duodenum and showed as a yellowish, calcified mass. It was dissected from the mesentery by hook and Harmonic scalpel. After specimen retrieval, the necrotic material from the mesenteric lymph-node showed cheese-like changes. We obtained the acid-fast bacteria (AFB) stain and culture from the specimen. The AFB stain and culture revealed growth of the Mycobacterium tuberculosis complex. From the histologic diagnosis, both the appendix and the mesenteric lymph-node showed chronic granulomatous inflammation, with caseous necrosis (Fig. 4). The Mantoux test was positive. The AFB stain from sputum was negative. The patient was discharged uneventfully, five days after surgery. Anti-TB medication was prescribed for 9 months. Currently, he quit the medication and is doing well.
TB can affect all organ systems, and the most commonly affected region is the lung [3]. Of extra-pulmonary locations of TB, bones and the urinary system are the most frequently affected (30% and 24%, respectively), followed by lymph nodes (13%) [3]. Abdominal TB may involve the gastrointestinal tract, peritoneum, lymph nodes, or solid organ; however, peritoneum and abdominal lymph nodes are the most common sites. In the pediatric literature, abdominal TB has been described infrequently, in 2 of 1,000 and 5 of 1,700 patients in industrialized countries [4,5].
TB of the appendix was first reported in 1837 by Corbin [6]. The incidence of primary tuberculous appendicitis was reported as 0.26% by Mittal et al. [7], 0.6% by Singh et al. [8], 2.3% by Gupta [7] in India and 0.13% by Sohn et al. [6] in Korea. In Japan, until 2010, primary TB of the appendix was observed in only 11 out of 29 cases of all TB of appendix [9]. It seems that primary tuberculous appendicitis is extremely rare. The cause of this rarity may be explained by the fact that the intestinal contents do not make direct contact with the luminal mucosa of appendix. As early as 1914, William J Mayo said that the appendix is an interesting organ because, although it has abundant lymphoid tissue as adenoid or Peyer's patch, was little involved in TB [10].
The mechanism of appendicular involvement in TB is not clear. It has been suggested that the appendix was primarily infected either hematogenously, from a distant focus which was not clinically detectable, or by direct contact with contaminated sputum or food. Also, the appendix was secondarily infected from: 1) direct invasion of adjacent organs, such as the ileocecal region or the urinary system, 2) retrograde lymphatic spread from distant lesions in either the ileum or the ascending colon, and 3) via appendicular serositis or periappendicitis, in peritoneal TB [2,6,8].
The clinical presentation is neither specific nor pathognomic. This makes pre-operative diagnosis difficult and delayed, resulting in a high percentage of complicated appendicitis. Borow and Friedman suggested three clinical features: 1) the chronic form-mild to moderate right quadrant abdominal pain, with nausea and vomiting, 2) the acute form-sudden onset of right quadrant abdominal pain, 3) the latent form [8,9].
The diagnosis is usually made by histopathological examination of the appendectomy specimen. It showed typical granuloma, with caseous necrosis surrounding the epithelioid cells and the Langhans giant cells. In this case, the appendix and the mesenteric mass also showed the TB infection. The mesenteric mass accompanying primary tuberculous appendicitis was first reported in this case. We could not ascertain the route of infection of the mesenteric lymph node. We considered that the mesenteric lymphnode involvement did not require further evaluation of intestinal TB, and we administered anti-TB medication. The regimen for anti-TB medication was the standard four drug chemotherapy, including isoniazid, rifampin, pyrazinamide and ethambutol. The anti-TB medication after appendectomy is known to decrease the incidence of the usual complications, such as stump blowout or fecal fistula [7].
In conclusion, abdominal TB can present with a variety of conditions. The primary appendicitis with mesenteric mass is extremely rare. The involvement of the mesenteric lymph node presenting with abdominal mass was possible with primary tuberculous appendicitis. It was confirmed by laparoscopic excision and was required anti-TBc medication.
Figures and Tables
References
1. Korea Centers for Disease Control & Prevention. Annual report on the notified tuberculosis patients in Korea 2009. 2010. Seoul: Korea Centers for Disease Control & Prevention.
2. Bobrow ML, Friedman S. Tuberculous appendicitis. Am J Surg. 1956. 91:389–393.
3. Raviglione MC, Snider DE Jr, Kochi A. Global epidemiology of tuberculosis. Morbidity and mortality of a worldwide epidemic. JAMA. 1995. 273:220–226.
4. Snider DE Jr, Rieder HL, Combs D, Bloch AB, Hayden CH, Smith MH. Tuberculosis in children. Pediatr Infect Dis J. 1988. 7:271–278.
5. Tinsa F, Essaddam L, Fitouri Z, Brini I, Douira W, Ben Becher S, et al. Abdominal tuberculosis in children. J Pediatr Gastroenterol Nutr. 2010. 50:634–638.
6. Sohn BH, Choi SO, Park WH. Tuberculosis of the appendix associated with as acute suppurative inflammatory reaction: a case report. J Korean Surg Soc. 1997. 53:927–930.
7. Mittal VK, Khanna SK, Gupta NM, Aikat M. Isolated tuberculosis of appendix. Am Surg. 1975. 41:172–174.
8. Singh MK, Arunabh , Kapoor VK. Tuberculosis of the appendix: a report of 17 cases and a suggested aetiopathological classification. Postgrad Med J. 1987. 63:855–857.
9. Ito N, Kawamoto S, Inada K, Nagao S, Kanemaru T, Noda N, et al. Primary tuberculosis of the appendix in a young male patient: report of a case. Surg Today. 2010. 40:668–671.
10. Park SW, Lee HL, Lee OY, Jeon YC, Han DS, Youn BC, et al. A case of appendicular tuberculosis presenting as acute appendicitis. Korean J Gastroenterol. 2007. 50:388–392.




 ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download