Abstract
Purpose
The aim of this study was to investigate the incidence and spectrum of malignant tumors in Korean neurofibromatosis type 1 (NF1) patients.
Methods
We retrospectively reviewed 125 patients who were diagnosed with NF1 at a single institution from 1995 to 2010. The incidence, location, histologic type, and radiologic findings of malignant tumors as well as development of multiple primary tumors were analyzed.
Results
Eighteen malignant tumors occurred in 16 patients (12.8%) among 125 Korean NF1 patients; 9 carcinomas, 8 sarcomas and 1 central nervous system (CNS) tumor. Five tumors were of nervous system origin and 13 were non-nervous system tumors. The locations of the tumors were as follow: 1 CNS, 2 lung, 3 breast, 3 stomach, 3 small bowel, 1 colon, 1 liver, 1 uterus, 1 neck, and 2 in extremities. Three malignant peripheral nerve sheath tumors (MPNSTs) occurred at the neck and extremity, and one in the liver. All three gastrointestinal stromal tumors (GISTs) had multiple tumors in the jejunum, and one MPNST and one pheochromocytoma were accompanied in two GISTs. Multiple primary tumors, benign or malignant were reported in 4 patients (25.0%), synchronously or metachronously.
Neurofibromatosis type 1 (NF1) is one of the cancer predisposing syndrome and malignant tumors developed four times as often in the NF1 patient group as in the general population [1]. Gastrointestinal stromal tumor (GIST), somatostatinoma and breast cancer are commonly related to NF1, in addition to nervous system tumors such as malignant peripheral nerve sheath tumor (MPNST) or optic nerve gliomas [2]. But, the evidence underlying the tumorigenesis of these NF1-related tumors are inadequate and it is controversial which types of tumor are NF1-related. In particular, there are few studies in Korea. Thus, we performed this study to investigate the incidence and spectrum of malignant tumors in Korean NF1 patients.
One hundred twenty five patients were diagnosed with NF1 in a single institution from 1995 to 2010. We used criteria for NF1 established by the National Institute of Health Consensus Development Conference in 1987 [3]. The diagnosis of NF1 was made on the basis of clinical features requiring the presence of at least two of the following criteria: six of more café-au-lait macules over 5 mm in greatest diameter in prepubertal individuals and over 15 mm in greatest diameter in postpubertal individuals; two or more neurofibromas of any type or one plexiform neurofibroma; axillary or inguinal freckling; optic pathway glioma; two or more Lisch nodules; bony dysplasia; or a first-degree relative with NF1. The mean age of patients was 31 years (range, 0 to 88 years), and 62 patients were female. The medical records of patients were retrospectively reviewed and the incidence, location, histologic type, radiologic findings of malignant tumors, development of multiple primary tumors, and survival period after diagnosis of malignant tumors were analyzed.
Eighteen malignant tumors developed in 16 patients (12.8%) among 125 Korean NF1 patients and 17 malignant tumors in 15 patients (16.1%) among 93 adults over 18 years old. The mean age of the patients at the time of diagnosis of malignant tumors was 51 years (range, 14 to 73 years), and nine patients were female.
The types of malignant tumors were as follows: 9 carcinomas, 8 sarcomas, and 1 central nervous system (CNS) tumor. Five tumors were nervous system origin and 13 were non-nervous system tumor. The locations of tumors were as follow: 1 CNS, 2 lung, 3 breast, 3 stomach, 3 small bowel, 1 colon, 1 liver, 1 uterus, 1 neck, and 2 in the extremities (Table 1). Three MPNSTs developed at the neck and extremity and one in the liver (Fig. 1). All three GISTs had multiple tumors in the jejunum (Fig. 2), and 1 MPNST and 1 pheochromocytoma were accompanied in 2 GISTs (Fig. 3).
NF1, also known as von Recklinghausen disease, is an autosomal dominant disorder that results from germ-line mutations in the NF1 gene located at chromosome 17q11.2 [4]. NF1 reduce the average life expectancy by 10 to 15 years and malignant tumors are the most common cause of death. Malignant tumors occur in 3 to 15% of NF1 patients and the high incidence of neoplasms is related with mutation of the NF1 gene. Neurofibromin, the protein encoded by the NF1 gene, is a negative regulator of the Ras-MAPK pathway which functions as a GTPase-activating protein for Ras by catalyzing the hydrolysis of active Ras-GTP to an inactive Ras-GDP, and NF1 gene is thus considered as a tumor suppressor gene. Additional somatic inactivation of the wild type NF1 allele results in complete loss of functional neurofibromin activity, and cell proliferation and differentiation are activated [5].
The spectrum of NF1 related tumors shows selective patterns. MPNST and CNS tumors, such as optic nerve glioma or astrocytoma, are the most common NF1 associated tumors. GIST, rhabdomyosarcoma, somatostatinoma, breast cancer and pheochromocytoma are also known as common tumors in NF1 patients. Some types of NF1-related tumors show different clinic-pathologic features from those of sporadic cases. Most NF1-related GISTs have multiple tumors in small intestine, and mutations of KIT or PDGFRA are rare [6]. Multiple primary tumors, synchronous or metachronous, are more common in NF1 patients with cancer, thus careful staging and postoperative surveillance is needed [7]. However, the estimation of the frequencies of specific tumors in NF1 patients is difficult and the incidence might be overestimated because most cohort studies are based on hospital data. Although malignant tumors are an important cause of mortality in NF1, studies for NF1-related tumors are inadequate and the mechanism underlying tumorigenesis remains obscure. Therefore, a large cohort study is needed to investigate the incidence and spectrum of NF1-related tumors, in addition to genetic study for finding out of underlying patho-mechanism.
We have searched journals from the web site "http://koreamed.org" using keywords "neurofibromatosis" and "von Recklinghausen disease" to investigate the pattern of malignant tumors in Korean NF1 patients. Three hundred twelve articles were founded from 1972 to 2011 and 82 cases of NF1 patients with malignant tumors were reported from 64 studies (Table 2). MPNSTs are the most frequent malignant tumors associated with NF1 and the lifetime risk of MPNST in NF1 patients is 8 to 13%. NF1 associated MPNSTs tend to occur at a younger age than those without the syndrome, often metastasize in an early phase of the disease and have a poor prognosis. Thirty one MPNSTs including four cases of this study were reported from 21 articles [8-10]. The distribution of MPNSTs shows similar patterns with other studies: 5 head and neck, 9 trunk (including 2 cases of breast), 6 extremities, 3 intra-thoracic, 2 intra-abdominal, 5 retro-peritoneum, and 1 spine. The lifetime risk of GISTs is 6% for NF1 patients, and the NF1-related GISTs show different clinic-pathologic characteristics from those of sporadic one. Seventeen GISTs including 3 cases in this study were reported from 10 articles [11-13]. Fourteen (82%) developed in female patients and all occurred in the jejunum multiply. All GISTs were positive to CD117 and 8 from 9 tumors had wild type KIT and PDGFRA. In children with NF1, the most common neoplasm apart from neurofibroma, is CNS tumors such as optic nerve glioma, and CNS tumors occur in approximately 15% of children with NF1. Eight CNS tumors including one from this study were reported from 6 articles [14]. Pheochromocytoma is a rare tumor of the adrenal gland that affects about 1% of NF1 patients and 8 pheochromocytomas were reported from 6 articles [15,16]. Ten multiple primary tumors (12.2%), benign or malignant, were found in 82 NF1 patients.
In this study, 18 malignant tumors developed in 16 patients (12.8%) among 125 Korean NF1 patients and we could confirm that Korean NF1 patients also had a high risk of developing malignant tumors. The types of tumors were similar with other studies. Uncommon tumors in Korean such as MPNST, GIST, and CNS tumors are probably NF1-related tumors. But, we cannot exclude the chance concomitance of two diseases for common tumors such as stomach, lung and colon cancer [17-20]. In NF1 patients, late diagnosis of malignant tumors with metastasis is common, and patients tend to refuse active treatment due to the economic reason and multiple primary tumors frequently develop. So, malignant tumors in NF1 patients usually have poor prognosis. This study has selection bias and the limitation in estimating the incidence of malignant tumors because this study was based on hospital data. But, this study might help in estimating the spectrum of malignant tumors in Korean NF1 patients.
In conclusion, Korean NF1 patients had a high risk of developing malignant tumors. The common malignant tumors in Koreans such as breast, lung, and colon cancer developed frequently in addition to the NF1-related tumors such as MPNST or GIST. But, a large population based cohort study is needed to confirm the incidence and spectrum of malignant tumors in Korean NF1 patients, because there are relatively few numbers of malignant tumors in NF1 patients in a single institution.
Figures and Tables
Fig. 1
Radiologic appearance of malignant peripheral nerve sheath tumors in different locations. (A) Neck magnetic resonance imaging shows a 7.5 × 5.2 × 3.2 cm sized, heterogeneously high signal mass at right carotid space on T2 weighted image. (B) Pelvic computed tomography (CT) scan shows huge, enhancing mass at left buttock with bony erosion of sacrum, coccyx, and ilium. (C) Abdominal CT scan shows bulky, enhancing mass at right posterior segment of liver.

Fig. 2
Radiologic and gross appearance of small bowel gastrointestinal stromal tumor. (A) Abdominal computed tomography scan shows large, jejunal mass with several smaller masses. (B) Resected segment of jejunum shows main tumor and numerous small nodular masses (Reprinted from Namgung H. J Korean Surg Soc 2011;81:276-80, with permission of the Korean Surgical Society).
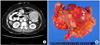
Fig. 3
Radiologic appearance of pheochromocytoma. Abdominal computed tomography scan shows large, well-defined, heterogeneously enhancing mass at right retroperitoneum. (A) Axial view. (B) Coronal view.

References
1. Zoller ME, Rembeck B, Oden A, Samuelsson M, Angervall L. Malignant and benign tumors in patients with neurofibromatosis type 1 in a defined Swedish population. Cancer. 1997. 79:2125–2131.
2. Korf BR. Malignancy in neurofibromatosis type 1. Oncologist. 2000. 5:477–485.
3. Neurofibromatosis. Conference statement. National Institutes of Health Consensus Development Conference. Arch Neurol. 1988. 45:575–578.
4. Jett K, Friedman JM. Clinical and genetic aspects of neurofibromatosis 1. Genet Med. 2010. 12:1–11.
5. Brems H, Beert E, de Ravel T, Legius E. Mechanisms in the pathogenesis of malignant tumours in neurofibromatosis type 1. Lancet Oncol. 2009. 10:508–515.
6. Miettinen M, Fetsch JF, Sobin LH, Lasota J. Gastrointestinal stromal tumors in patients with neurofibromatosis 1: a clinicopathologic and molecular genetic study of 45 cases. Am J Surg Pathol. 2006. 30:90–96.
7. Sorensen SA, Mulvihill JJ, Nielsen A. Long-term follow-up of von Recklinghausen neurofibromatosis. Survival and malignant neoplasms. N Engl J Med. 1986. 314:1010–1015.
8. Kang MJ, Kang H, Kim HO, Park YM. A case of malignant peripheral sheath tumor arising from neurofibromatosis type 1. Ann Dermatol. 2008. 20:32–36.
9. Gu B, Park JW, Jang LC, Kim SH, Bae IH, Park WY, et al. Retroperitoneal malignant peripheral nerve sheath tumors complicated with type I neurofibromatosis. J Korean Surg Soc. 2006. 71:365–370.
10. Kim DH, Lee SS, Lee SH, Lee DW. A case of malignant peripheral nerve sheath tumor of the neck associated with neurofibromatosis type I. Korean J Otorhinolaryngol-Head Neck Surg. 2010. 53:657–660.
11. Kang DY, Park CK, Choi JS, Jin SY, Kim HJ, Joo M, et al. Multiple gastrointestinal stromal tumors: Clinicopathologic and genetic analysis of 12 patients. Am J Surg Pathol. 2007. 31:224–232.
12. Namgung H. Gastrointestinal stromal tumor with KIT mutation in neurofibromatosis type 1. J Korean Surg Soc. 2011. 81:276–280.
13. Seo SO, Oh HJ, Kim KH, Choi CS, Seo GS, Kim TH, et al. A case of duodenal GIST accompanied with neurofibromatosis-1, presenting with gastrointestinal bleeding. Korean J Gastrointest Endosc. 2007. 35:254–257.
14. Myong NH, Lee SS, Shu YL, Chi JG. Optic nerve glioma with neurofibromatosis. Korean J Pathol. 1993. 27:524–530.
15. Yi HS, Kim SH, Kim J, Bae EJ, Hong S, Park IB, et al. Mutational analysis of the NF1 gene in two families with neurofibromatosis 1 accompanied by pheochromocytoma. Endocrinol Metab. 2011. 26:177–184.
16. Jeong CY, Hong SC, Lee YJ, Jung EJ, Choi SK, Joo YT, et al. Multiple duodeno-jejunal GIST associated with pheochromocytoma in patients with von Recklinghausen disease. J Korean Surg Soc. 2005. 69:74–78.
17. Kim KJ, Choi SR, Sohn SH, Lee S, Hong KB, Keum DJ, et al. A case of colon cancer in a patient with neurofibromatosis type I. Korean J Gastroenterol. 2002. 40:402–405.
18. Lee MH, Yang JH, Han SD, Kim HR, Jung YK, Kim SM, et al. Apical lung cancer associated with neurofibromatosis type 1. J Korean Neurol Assoc. 2004. 22:562–563.
19. Kim SH, Son WJ, Sin DJ, Chang MC. Bilateral metachronous breast cancer in neurofibromatosis type 1. J Korean Surg Soc. 2009. 76:388–391.
20. Im DH, Whang HC, Oh JS, Kim HJ, Lee HM, An JK, et al. A case of early gastric adenocarcinoma and intraabdominal schwannoma in a patient with neurofibromatosis type I. Korean J Gastrointest Endosc. 2007. 34:83–87.




 ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download