Abstract
Purpose
Conventional laparoscopic appendectomy is performed using three ports, and single-port appendectomy is an attractive alternative in order to improve cosmesis. The aim of this study was to compare pain after transumbilical single-port laparoscopic appendectomy (SA) with pain after conventional three-port laparoscopic appendectomy (TA).
Methods
From April to September 2011, 50 consecutive patients underwent laparoscopic appendectomy for simple appendicitis without gangrene or perforation. Patients who had undergone appendectomy with a drainage procedure were excluded. The type of surgery was chosen based on patient preference after written informed consent was obtained. The primary endpoint was postoperative pain evaluated by the visual analogue scale score and postoperative analgesic use. Operative time, recovery of bowel function, and length of hospital stay were secondary outcome measures.
Results
SA using a SILS port (Covidien) was performed in 17 patients. The other 33 patients underwent TA. Pain scores in the 24 hours after surgery were higher in patients who underwent SA (P = 0.009). The change in postoperative pain score over time was significantly different between the two groups (P = 0.021). SA patients received more total doses of analgesics (nonsteroidal anti-inflammatory drugs) in the 24 hours following surgery, but the difference was not statistically significant. The median operative time was longer for SA (P < 0.001).
Laparoscopic appendectomy is now considered the gold standard for appendectomy, even in complicated appendicitis [1]. The reported advantages of laparoscopic appendectomy compared with open appendectomy are less postoperative pain, less wound infection, and better cosmetic results [2,3]. Multiple case series and comparative analyses have recently described single-port or single-incision surgery for the treatment of acute appendicitis [4-12]. The great majority of these studies have demonstrated technical feasibility and good cosmetic results. However, to date there are no reported advantages of these procedures over conventional laparoscopic appendectomy except for cosmetic results. Disadvantages of single-port or single-incision appendectomy seem to include more postoperative pain due to longer operative time and a larger fascial incision compared to conventional laparoscopic appendectomy. However, only a few studies have assessed pain after single-port or single-incision appendectomy indirectly based on analgesic dose [8,10,13,14] or directly based on visual analogue scale (VAS) pain scores [10,14]. Therefore, we conducted a prospective observational study comparing pain after transumbilical single-port laparoscopic appendectomy (SA) and conventional three-port laparoscopic appendectomy (TA) for simple appendicitis.
From April to September 2011, 50 consecutive patients underwent laparoscopic appendectomy for simple appendicitis without gangrene or perforation performed by one surgeon at our hospital. Patients who had undergone appendectomy with a drainage procedure were excluded. The type of surgery was chosen based on patient preference after written informed consent was obtained. SA was performed using a SILS port (Covidien, Norwalk, CT, USA) in 17 patients. The other 33 patients underwent TA.
The patient was placed in a supine position with the surgeon and assistant on the patient's left and right, respectively. A 20 mm longitudinal incision was made through the umbilicus and the fascia and peritoneum were opened under direct vision; therefore the natural umbilical defect was used to access the intraperitoneal cavity. The SILS port was then inserted into the incision. Three 5 mm cannulas were inserted into the SILS port at different heights to reduced clashes between the cannulas, and insufflation of carbon dioxide gas through a three-way catheter was performed to achieve pneumoperitoneum (Fig. 1).
The operation was performed with the surgeon and assistant (scopist) positioned on the left side of the patient. The patient was placed in the Trendelenburg position with the left side down. A rigid 0°5 mm laparoscope and 5 mm laparoscopic instruments were inserted through the cannulas. Appendectomy was performed in a similar manner with TA, but it was difficult to adhere to the traditional laparoscopic principles of triangulation due to instrument clashes (Fig. 1). The mesoappendix was first divided using ultrasonic shears (Harmonic Scalpel, Ethicon Endo-Surgery Inc., Cincinnati, OH, USA), and then the base of the appendix was ligated using a round loop (Laploop, Sejong Medical Co., Paju, Korea) and resected. After changing one of the 5 mm cannulas to a 5 to 12 mm cannula, the resected appendix was removed through the 5 to 12 mm cannula with the aid of a bag (Lapbag; Sejong Medical Co.). The umbilical fascia was closed with 2-0 Vicryl sutures, and the subcutaneous layer was sutured with 4-0 Vicryl to the alignment of the skin edges without skin suture.
Using a modified Hasson technique to access the peritoneum, a 5 to 12 mm blunt laparoscopic port was inserted into the supraumbilical position including the center of the umbilicus. Two additional 5 mm laparoscopic ports were inserted into the suprapubic and left iliac fossa positions under laparoscopic direct vision. Appendectomy was performed using common laparoscopic instruments including a Harmonic Scalpel, Laploop, and Lapbag. The umbilical wound was closed in the same manner as described in the previous section.
Patients received a 1.0 g (adult) or 20 mg/kg (child) dose of cefotetan before the operation. Intravenous antibiotics were continued during the hospital stay. All patients were allowed a clear fluid diet after subjective full recovery from general anesthesia, and diet was advanced as tolerated. Postoperative pain was measured using the VAS every three hours except during sleep and whenever patients complained of pain. VAS was graded from 0 to 10. All VAS scoring was performed by the attending nurse who was unaware of the ongoing study.
Relaxation therapy was administered first for pain management, and then nonsteroidal anti-inflammatory drugs (NSAIDs) were injected intramuscularly as needed for pain that had not improved. Opioids or oral analgesics were not used. Patients were eligible for discharge when they tolerated a regular diet. However, analgesic dose and time of discharge were largely decided by the patient.
This was a prospective observational study, and the study protocol was approved by the local ethics committee at our institute. The primary endpoint was postoperative pain evaluated by VAS score and postoperative analgesic use. Collected data included patient demographics, clinicopathologic characteristics, and perioperative outcomes including operative time, recovery of bowel function, length of hospital stay, total dose of analgesics, and VAS pain score.
Results are expressed as median values with the interquartile range or mean values ± standard deviations. Continuous variables were compared using Student's t-test, the Mann-Whitney U-test or repeated measures analysis of variance. Discrete variables were analyzed with the χ2 test or Fisher's exact test. Statistical analysis was performed using SPSS ver. 19.0 (IBM, New York, NY, USA). A probability of 0.05 or less was considered statistically significant.
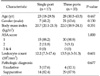
There was no difference in age, gender distribution, body mass index (BMI), American Society of Anesthesiologists score, preoperative leukocyte count, or pathologic results between patients who underwent SA and those who underwent TA (Table 1).
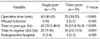
Perioperative outcomes are listed in Table 2. There was no case in which an additional port outside the umbilicus (SILS port) was inserted during SA. The median operative time was longer with SA (P < 0.001). There were no intraoperative complications, although two wound infections (omphalitis) developed in patients who underwent TA. Time to pass gas was achieved earlier in the TA group (P < 0.001), but there were no differences in time to regular diet and length of postoperative hospital stay.
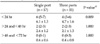
Median and mean postoperative pain scores are listed in Table 3. When a discrepancy in pain scores presented within the same period, the highest scores were analyzed. Pain score in the 24 hours after surgery was higher in patients who underwent SA (P = 0.009; corrected by Bonferroni's method). However, there were no differences for 24 to 48 hours and 48 to 72 hours after surgery (Fig. 2). The change in postoperative pain score over time was significantly different between the two groups (P = 0.021 by repeated measures analysis of variance) (Fig. 3). Patients in the SA group tended to receive more total doses of analgesics (NSAIDs) in the 24 hours after surgery, but the different was not statistically significant (Table 4). No patients needed opioids or oral analgesics.
Laparoscopic surgeons have made great efforts to improve perioperative outcomes in patients undergoing appendectomy. The establishment of three ports via the umbilicus, the suprapubic region and the left iliac fossa is currently considered the best approach to achieve proper triangulation [15]. The use of two trocars has been investigated retrospectively, but no significant advantage was found [16]. At present, there is no evidence that a single-port technique is an adequate alternative to standard laparoscopic appendectomy. A recent prospective randomized trial of single-incision versus standard three-port laparoscopic appendectomy was performed and found that operative time, doses of narcotics, surgical difficulty and hospital charges were greater with the single-site approach [13]. Several other minimally invasive single-port or single-incision techniques have been introduced for the treatment of acute appendicitis [4-13,17]. However, the majority of these studies have demonstrated only safety, feasibility or ambiguous cosmetic outcomes, without definitive advantages over conventional laparoscopic appendectomy.
As the number of ports is reduced to one, the length of the single fascial incision tends to be longer. The length of the fascial incision is closely associated with postoperative wound pain. The single umbilical incisions reported in other studies typically reached lengths of 15 to 20 mm [4,6-8,10,12,13]. However, there are only a few studies that have assessed pain after single-port or single-incision appendectomy. One prospective study found more total doses of analgesia were given to single-site patients during their hospital stay, but not during convalescence [13]. Another prospective study reported that VAS pain score during the first 24 postoperative hours was significantly higher in patients who underwent SA [14], whereas two retrospective studies did not find differences in postoperative pain between SA and TA [8,10]. The present prospective study focused on postoperative pain and showed that pain score in the 24 hours after surgery was higher in patients who underwent SA, and that the change in postoperative pain score over time was significantly different between the two groups. These discrepancies in findings among studies may be due to different surgical techniques, operative time, and study design. In this study, the longitudinal fascial incision made through the umbilicus to insert the SILS port had a length of 20 mm. In surgical techniques using a 15 mm single umbilical incision, there was no difference in terms of VAS pain score and postoperative analgesic requirements [8,10]. However, these two studies were retrospective, and the primary outcome assessed was not postoperative pain [8,10].
Our other concern was operative time. Our study found SA to have an approximately 15 minutes longer operative time, which was statistically significant. Longer operative time may translate to more stretching of the single umbilical wound, and subsequently more postoperative pain. A limitation of this investigation is that it was not a randomized double blind study. However, the postoperative pain assessment was somewhat blinded as all scoring was performed by the attending nurse who was unaware of the ongoing study.
The only advantage of SA over TA may be improved cosmetic results, although no studies have objectively evaluated the cosmetic results of SA (Fig. 4). To emphasize the cosmetic advantages of SA, an objective assessment of cosmesis should be performed comparing SA with TA in the future. However, although cosmetic results may be better in SA, cosmesis may not outweigh other perioperative disadvantages. The time to pass gas was longer in the SA group in this study, and postoperative pain may be associated with delayed passage of gas.
Surgeons should make an effort to reduce postoperative pain in SA patients, especially in the 24 hours after the SA. In this study, patients who underwent SA tended to receive more total doses of analgesics (NSAIDs) in the 24 hours after operation, but there was no statistical difference between groups due to the small sample size and the relatively small number of analgesic doses administered in both groups. The mean number of analgesic doses administered in the 24 hours after SA was 1.2 in this study. The postoperative dose of analgesics was somewhat small in part due to a superstition in Korea in which surgical patients believe that postoperative analgesics impede wound healing. In another study, the mean number of analgesic doses during a mean of 22.7 hours in the hospital after SA was 9.6 [13].
Various modalities besides pharmacologic agents for postoperative pain control have been developed. Among them, local anesthetic infiltration and transversus abdominis plane (TAP) blocks to control postoperative port-site pain have yielded variable analgesic effects [18-20]. Further trials focused on the effects of local anesthetic infiltration or TAP blocks after SA are planned at our hospital.
In conclusion, laparoscopic surgeons should be concerned about longer operation times and higher immediate postoperative pain scores in patients who undergo SA.
Figures and Tables
Fig. 1
Transumbilical single-port laparoscopic appendectomy (SA). (A) Preoperative view. (B) A longitudinal umbilical incision about 20 mm in length. (C) The SILS port was inserted into the umbilical incision. (D) External view during SA. (E) The mesoappendix was first divided using ultrasonic shears. (F) The base of the appendix was ligated using a round loop. (G, H) The resected appendix was removed with the aid of a bag.

Fig. 2
Postoperative pain score on the visual analogue scale according to the number of ports as a function of time after laparoscopic appendectomy. a)Pain in the 24 hours after surgery was higher in patients who underwent transumbilical single-port laparoscopic appendectomy (P = 0.009; corrected by Bonferroni's method).

Fig. 3
The change in the visual analogue scale pain score as a function of postoperative time was significantly different between the two groups (P = 0.021 by repeated measures analysis of variance).
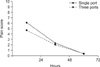
Fig. 4
Example of cosmetic results in this study. (A) At the time of closure. (B) Seven days postoperatively.

References
1. Tiwari MM, Reynoso JF, Tsang AW, Oleynikov D. Comparison of outcomes of laparoscopic and open appendectomy in management of uncomplicated and complicated appendicitis. Ann Surg. 2011. 254:927–932.
2. Wei HB, Huang JL, Zheng ZH, Wei B, Zheng F, Qiu WS, et al. Laparoscopic versus open appendectomy: a prospective randomized comparison. Surg Endosc. 2010. 24:266–269.
3. Wei B, Qi CL, Chen TF, Zheng ZH, Huang JL, Hu BG, et al. Laparoscopic versus open appendectomy for acute appendicitis: a metaanalysis. Surg Endosc. 2011. 25:1199–1208.
4. Chouillard E, Dache A, Torcivia A, Helmy N, Ruseykin I, Gumbs A. Single-incision laparoscopic appendectomy for acute appendicitis: a preliminary experience. Surg Endosc. 2010. 24:1861–1865.
5. Chow A, Purkayastha S, Nehme J, Darzi LA, Paraskeva P. Single incision laparoscopic surgery for appendicectomy: a retrospective comparative analysis. Surg Endosc. 2010. 24:2567–2574.
6. Hong TH, Kim HL, Lee YS, Kim JJ, Lee KH, You YK, et al. Transumbilical single-port laparoscopic appendectomy (TUSPLA): scarless intracorporeal appendectomy. J Laparoendosc Adv Surg Tech A. 2009. 19:75–78.
7. Kim HJ, Lee JI, Lee YS, Lee IK, Park JH, Lee SK, et al. Single-port transumbilical laparoscopic appendectomy: 43 consecutive cases. Surg Endosc. 2010. 24:2765–2769.
8. Lee J, Baek J, Kim W. Laparoscopic transumbilical single-port appendectomy: initial experience and comparison with three-port appendectomy. Surg Laparosc Endosc Percutan Tech. 2010. 20:100–103.
9. Lee SY, Lee HM, Hsieh CS, Chuang JH. Transumbilical laparoscopic appendectomy for acute appendicitis: a reliable one-port procedure. Surg Endosc. 2011. 25:1115–1120.
10. Lee YS, Kim JH, Moon EJ, Kim JJ, Lee KH, Oh SJ, et al. Comparative study on surgical outcomes and operative costs of transumbilical single-port laparoscopic appendectomy versus conventional laparoscopic appendectomy in adult patients. Surg Laparosc Endosc Percutan Tech. 2009. 19:493–496.
11. Ohno Y, Morimura T, Hayashi S. Transumbilical laparoscopically assisted appendectomy in children: the results of a single-port, single-channel procedure. Surg Endosc. 2012. 26:523–527.
12. Raakow R, Jacob DA. Initial experience in laparoscopic single-port appendectomy: a pilot study. Dig Surg. 2011. 28:74–79.
13. St Peter SD, Adibe OO, Juang D, Sharp SW, Garey CL, Laituri CA, et al. Single incision versus standard 3-port laparoscopic appendectomy: a prospective randomized trial. Ann Surg. 2011. 254:586–590.
14. Park JH, Hyun KH, Park CH, Choi SY, Choi WH, Kim DJ, et al. Laparoscopic vs transumbilical single-port laparoscopic appendectomy; results of prospective randomized trial. J Korean Surg Soc. 2010. 78:213–218.
15. Vettoretto N, Gobbi S, Corradi A, Belli F, Piccolo D, Pernazza G, et al. Consensus conference on laparoscopic appendectomy: development of guidelines. Colorectal Dis. 2011. 13:748–754.
16. Fazili FM, Al-Bouq Y, El-Hassan OM, Gaffar HF. Laparoscope-assisted appendectomy in adults: the two-trocar technique. Ann Saudi Med. 2006. 26:100–104.
17. Stanfill AB, Matilsky DK, Kalvakuri K, Pearl RH, Wallace LJ, Vegunta RK. Transumbilical laparoscopically assisted appendectomy: an alternative minimally invasive technique in pediatric patients. J Laparoendosc Adv Surg Tech A. 2010. 20:873–876.
18. Cervini P, Smith LC, Urbach DR. The effect of intraoperative bupivacaine administration on parenteral narcotic use after laparoscopic appendectomy. Surg Endosc. 2002. 16:1579–1582.
19. Sandeman DJ, Bennett M, Dilley AV, Perczuk A, Lim S, Kelly KJ. Ultrasound-guided transversus abdominis plane blocks for laparoscopic appendicectomy in children: a prospective randomized trial. Br J Anaesth. 2011. 106:882–886.
20. Conaghan P, Maxwell-Armstrong C, Bedforth N, Gornall C, Baxendale B, Hong LL, et al. Efficacy of transversus abdominis plane blocks in laparoscopic colorectal resections. Surg Endosc. 2010. 24:2480–2484.




 ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download