Abstract
Solid pseudopapillary tumor of the pancreas is a rare tumor that affects young females with low malignant potential and good prognosis with more than 90% survival at 5 years. Metastasis is very rare. We report the case of a 74-year-old female who had pancreatic solid-pseudopapillary tumor and synchronous hepatic metastasis.
Solid pseudopapillary tumor (SPT) of the pancreas has been variously designated as solid and cystic tumors, solid and papillary epithelial neoplasms, papillary cystic neoplasms, papillary cystic tumors, and Frantz's tumors. The World Health Organization renamed this tumor as SPT in the International Histological Classification of Tumors [1]. SPT represents a rare tumor that occurs most frequently in young women (90%). Although SPT is considered an indolent lesion with a low malignant potential and a favorable prognosis after surgical resection, some cases of locally infiltrating and metastatic varieties, or recurrences after surgery, have been reported. We report a rare case of SPT in the pancreas with hepatic metastasis.
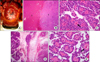
A 74-year-old woman was admitted to the hospital for fever and general weakness. On the computed tomography scan, there was large abscess cavity showing partially septated cystic lesion with peripheral inflammatory hyperemia in the right hepatic lobe. Incidentally, a lobulated, 5 × 3.2 cm, heterogeneous pancreatic mass containing several intratumoral calcification and cystic change on the tail of the pancreas and a 6-cm, well-defined mass with heterogeneous contrast enhancement in the left lobe of the liver were detected (Fig. 1). Two months after conservative treatment for hepatic abscess, the abscess was completely resolved. However, the mass in the left lobe of the liver remained unchanged and then ultrasound-guided liver biopsy was performed. The tumor consisted of papillary neoplasm showing monomorphic polyhedral cells with hyalinized fibrovascular stalks, which was best classified as metastatic SPT of the pancreas. Immunohistochemistry was positive for vimentin, antitrypsin, and neuron specific enolase. On the presumption of an SPT of the pancreas with hepatic metastasis, the patient underwent radical antegrade modular pancreatosplenectomy with hepatic resection. On operation field, there were no seeding nodules or other metastatic lesions in the abdominal cavity. Encapsulated masses, 6 × 5 cm and 5 × 4.5 cm in size, were found in the segment of the left liver and in the tail of the pancreas, respectively. All surgical margins were clear. Microscopically, the growth pattern of the pancreas tumor was heterogeneous, with a combination of solid and pseudocystic structures in varying proportions. The tumor was composed of monomorphic polyhedral cells with hyalinized fibrovascular cores, thereby leading to the characteristic pseudopapillary appearance (Fig. 2). Mitotic activity was low. However, perineural invasion and infiltration into the peripancreatic fat tissue could be seen. Twenty-five lymph nodes examined were free of tumor. Less than 5% of tumor cells were positive for Ki-67. The Microscopic findings of the hepatic tumor were similar to the findings of the pancreatic tumor. A final diagnosis of SPT of the pancreas with metastasis to the liver was made. Currently the patient is alive without recurrent disease (10 months after operation).
SPT is a rare neoplasm of the pancreas accounting for only 1 to 2% of all exocrine pancreatic tumors [2]. Although SPT occurs in young females and is generally considered to be low malignant potential, local recurrence or distant metastases can be found in a significant number of patients [3]. Mao et al. [2] reviewed the reported 292 patients with SPT, 14.7% (43 of 292) were evaluated as malignant due to metastasis (22 of hepatic, lymph node metastasis or peritoneal dissemination) or invasion into adjacent organs. The prognosis for SPTs is excellent after curative resection (more than 90% survival at 5 years). Metastasis develops in less than 15% of cases and among them hepatic metastasis is most common. Curative resection for hepatic metastasis is possible if involvement is limited. Martin et al. [4] suggested that complete resection was associated with long-term survival even in the presence of metastatic disease. In case report series, even patients with local recurrence as well as liver and peritoneal metastasis have experienced long-term survival [4-8]. There were some features predicting metastasis. One study suggested that patient age tended to be older and the tumor size tended to be larger in metastasizing SPT than in non-metastasizing SPT. Invasion of blood vessels, perineural clefts and adjacent organs, a high degree of cellular pleomorphism and an elevated mitotic rate are considered to associated with metastasis [9]. Nishihara et al. [10] compared the histological features of metastasizing SPT and non-metastasizing SPT and reported that venous invasion, nuclear grade, and prominent necrobiotic nests are useful as histologic indicators for the malignant potential of SPT. The present patient was very old age and had an incidental detection of the disease. Microscopic findings showed focally-infiltrative and perineural invasion, while without lymph node metastasis and less than 5% of Ki-67 positivity. Preoperative information from liver biopsy was important in making the surgical strategy.
In conclusion, we report a case of pancreatic SPT with synchronous hepatic metastasis, which appeared later in life. Preoperative diagnostic work-up is a cornerstone for surgical approach and complete resection should be considered for this potentially curative disease if operation is possible. The literatures reported up to date, as well as our case, demonstrate an aggressive approach to this rare low-grade malignant tumor can result in long-term survival even in patients with local invasion and distant metastasis.
Figures and Tables
Fig. 1
Computed tomography scan of abdomen. There was large abscess cavity showing partially septated cystic lesion with peripheral inflammatory hyperemia in right hepatic lobe (A). There was a 5 × 6.2 cm, well-defined mass with heterogeneous contrast enhancement in hepatic segment S3 (B) and a lobulated, 5 × 3.2 cm, heterogeneous pancreatic mass containing several intratumoral calcifications (arrow) and cystic change (arrow head) around pancreatic tail (C). The hepatic abscess was completely resolved 2 months after antibiotic treatment for hepatic abscess (D).
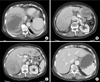
Fig. 2
On operation field, there was hepatic mass in lower portion of left lateral segment of liver (S3) and resection plane was marked on surface of liver (A). Microscopic findings of the left lobe of the liver and the pancreas. Low-power micrograph showing normal liver tissue (L) and tumor tissue (T in B), normal pancreas (P) and tumor tissue (T in D). Monomorphic polyhedral cells with hyalinzed fibrovascular stalks (arrow) were noted in hepatic tumor (C) and pancreatic tumor (E).
References
1. Kloppel G, Solcia E, Longnecker DS, Capella C, Sobin LH. Histological typing of tumours of the exocrine pancreas. 1996. 2nd ed. Berlin: Springer-Verlag.
2. Mao C, Guvendi M, Domenico DR, Kim K, Thomford NR, Howard JM. Papillary cystic and solid tumors of the pancreas: a pancreatic embryonic tumor? Studies of three cases and cumulative review of the world's literature. Surgery. 1995. 118:821–828.
3. Madan AK, Weldon CB, Long WP, Johnson D, Raafat A. Solid and papillary epithelial neoplasm of the pancreas. J Surg Oncol. 2004. 85:193–198.
4. Martin RC, Klimstra DS, Brennan MF, Conlon KC. Solid-pseudopapillary tumor of the pancreas: a surgical enigma? Ann Surg Oncol. 2002. 9:35–40.
5. Horisawa M, Niinomi N, Sato T, Yokoi S, Oda K, Ichikawa M, et al. Frantz's tumor (solid and cystic tumor of the pancreas) with liver metastasis: successful treatment and long-term follow-up. J Pediatr Surg. 1995. 30:724–726.
6. Matsunou H, Konishi F. Papillary-cystic neoplasm of the pancreas. A clinicopathologic study concerning the tumor aging and malignancy of nine cases. Cancer. 1990. 65:283–291.
7. Ogawa T, Isaji S, Okamura K, Noguchi T, Mizumoto R, Ishihara A. A case of radical resection for solid cystic tumor of the pancreas with widespread metastases in the liver and greater omentum. Am J Gastroenterol. 1993. 88:1436–1439.
8. Sclafani LM, Reuter VE, Coit DG, Brennan MF. The malignant nature of papillary and cystic neoplasm of the pancreas. Cancer. 1991. 68:153–158.
9. Klimstra DS, Wenig BM, Heffess CS. Solid-pseudopapillary tumor of the pancreas: a typically cystic carcinoma of low malignant potential. Semin Diagn Pathol. 2000. 17:66–80.
10. Nishihara K, Nagoshi M, Tsuneyoshi M, Yamaguchi K, Hayashi I. Papillary cystic tumors of the pancreas. Assessment of their malignant potential. Cancer. 1993. 71:82–92.




 Citation
Citation Print
Print


 XML Download
XML Download