Abstract
Purpose
We investigated the incidence and risk factors of hypothyroidism after thyroid lobectomy, and evaluated the possibility to predict hypothyroidism preoperatively with serologic markers, such as thyrotropin (TSH), thyroglobulin (TG), anti-thyroglobulin (ATA), and anti-microsomal antibody (AMA).
Methods
We enrolled 123 consecutive patients who underwent thyroid lobectomy due to benign conditions between May 2004 and April 2008. Only preoperative euthyroid patients were included. Patients were divided into two groups by postoperative thyroid function outcomes, into hypothyroid (n = 97) and euthyroid groups (n = 26), and analyzed specially for the preoperative levels of TSH, TG, ATA, and AMA.
Results
Twenty-six (21.1%) patients developed hypothyroidism following thyroid lobectomy within 35.7 months of follow-up. The proportion of post-lobectomy hypothyroidism was high in patients with high-normal preoperative TSH level, and the cut-off value was 2.0 mIU/L, with 67% sensitivity and 75% specificity. The quantitative titer of preoperative TG, ATA, and AMA was not significant, but the outcome of categorical analysis of two or more positivities on these three markers was significantly higher in hypothyroid patients than in euthyroid patients (28.6% vs. 3.9%, P = 0.024). The combined positivity of preoperative TSH and two or more positivities of TG, ATA, and AMA possess 100% positive predictive value and 81% negative predictive value.
With reported rates between 6.5 and 45% in the literature [1-4], hypothyroidism following lobectomy or hemi-thyroidectomy (if additional isthmectomy was performed) remains an inevitable sequelae. In the past, it was common practice to prescribe suppressive dosage of levothyroxine after thyroid lobectomy. However, its effect on preventing the formation of nodules in the remaining thyroid and its adverse effects, such as atrial fibrillation and bone calcium loss, remain unclear and render clinicians reluctant to encourage patients to take daily thyroid replacement.
Many studies have attempted to identify the risk factors for post-lobectomy hypothyroidism, and to reduce postoperative thyroid hormone replacement. Many risk factors have been suggested, including age [5], high serum thyrotropin (TSH) levels [4-6], lower free T4 levels [7], and the presence of thyroid antibodies [4] preoperatively. In contrast, we can see the results of thyroiditis [2,4], residual thyroid volume [8], thyroiditis [4], multinodular goiter [6], and small thyroid remnant after thyroid lobectomy after surgery [2,6]. There exist only one report on a preoperative predictive study of hypothyroidism. Tomoda et al. [5] suggested a predictive scoring system based on preoperative TSH levels and age. No other study predicted post lobectomy hypothyroidism preoperatively.
Thyroiditis is the end result of inflammatory process by thyroid antigens and its antibodies [9], and subclinical thyroiditis is predictable through anti-thyroglobulin (ATA) and anti-microsomal antibody (AMA) preoperatively [10]. The objectives of this study were to determine the incidence, risk factors, and ability to predict hypothyroidism preoperatively by using TSH, thyroglobulin (TG), ATA, and AMA.
This was a retrospective study that included consecutive patients who underwent thyroid lobectomy due to benign conditions between May 2004 and April 2008. Clinical and pathologic data were available in 123 patients, but 26 patients did not have serologic data, particularly TG, ATA and AMA.
Surgical procedure was performed by two experienced surgeons (Jegal YJ and Yoon JH) at our institution, with classic low cervical incision, minimal invasive lobectomy, and via the endoscopic approach. Hemi-thyroidectomy usually involves lobectomy and isthmectomy at the same time, but it remains difficult to define isthmectomy precisely. Thus, hemi-thyroidectomy was defined if the thyroid beyond the centerline of trachea was resected and confirmed by follow-up ultrasonography.
Only preoperative euthyroid patients were included (normal range, 0.5 to 6.0 mIU/L) in this study, and patients with TSH levels greater than 6.0 mIU/L were diagnosed with hypothyroidism. All patients with preoperative hypothyroidism, radiation history, thyroid surgery, premedication to control thyroid function with levothyroxine or anti-thyroid drugs were excluded. Patients psychologically dependent on levothyroxine with TSH levels <6.0 mIU/L were excluded. Patients who received less than 6 months of follow-up or those who did not undergo preoperative TG, ATA, and AMA evaluation were also excluded. If patients did not return for follow-up one year after the last follow-up, summons was obtained by telephone and included in this study.
Patients were followed up at 3 to 6 months intervals during the first two postoperative years, and annually thereafter. At each visit, we took careful history of hypothyroidism symptoms and checked serum thyroid hormone levels. Neck ultrasonography was performed for suspected recurrence of benign or malignant nodular lesions. No patient required completion thyroidectomy of the contralateral lobe during the follow-up period. Most patients who developed postoperative hypothyroidism were commenced with levothyroxine, but some were delayed a few months later.
The preoperative and postoperative follow-up profiles of all patients were analyzed. 1) Preoperative assessment included patient demographics, laboratory and hormonal assays including preoperative TSH, TG, ATA, and AMA. 2) Surgical factors included approach, laterality of thyroid lobectomy and the extent of isthmus ablation. 3) Postoperative assessment included pathology, portion and size of benign tumors and the presence of thyroiditis. Histologic thyroiditis was graded on a scale of 0 to 4 according to Williams and Doniach [11], and scoring was performed by pathologists who were blind to the laboratory data and operative findings.
Patients were divided into two groups: hypothyroid (n = 97) and euthyroid (n = 26) state after thyroid lobectomy for benign conditions. The parameters discussed above were compared. We used the t-test to compare continuous variables between each group and the chi-square test for categorical variables. Binary logistic regression test was used for multivariate analysis of statistically significant variables from the univariate analysis. We consider statistical significance when the P-value was less than 0.05 (P < 0.05). Results were analyzed by using PASW ver. 18.0 (SPSS Inc., Chicago, IL, USA).
Of the 123 patients, 26 (21.1%) developed hypothyroidism following thyroid lobectomy and 97 remained euthyroid. The mean length of follow-up was 35.7 months (range, 6 to 80 months). Age, sex, follow-up period and operation type were not significant factors for post-lobectomy hypothyroidism development. A total of 108 patients underwent classic open surgery through low cervical incision, 21 patients underwent minimal incision with less than 3.0 cm in length and 21 via the endoscopic approach. The operation approach (P = 0.206), laterality (P = 0.238) and isthmus ablation (P = 0.237) were not significant factors. The pathologic characteristics of the resected thyroid tissue did not show significant difference in pathology, portion, tumor size, and the presence of histologic thyroiditis (P = 0.635).
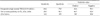
Only postoperative TSH was significantly different (P < 0.001) in the euthyroid group (median TSH, 2.5 mIU/L; range, 0.5 to 6.0 mIU/L) compared with the hypothyroid group (median TSH, 9.5 mIU/L; range, 6.1 to 29 mIU/L) (Table 1).
We assumed high normal preoperative TSH levels and subclinical thyroiditis to be factors for post-lobectomy hypothyroidism, as is in other studies [2,4]. The proportion of post-lobectomy hypothyroidism was higher normal side (TSH 2.0 to 5.9 mIU/mL) distributed and statistically significant (P < 0.001) in preoperative TSH levels. The cut-off value of preoperative TSH was 2.0 mIU/L, and the area under curve was 0.841, 95% confidence interval (CI): (0.76 to 0.92) (Table 2). As thyroid lobectomy reduces functioning thyroid tissue, patients whose thyroid glands were at the limit of their capacity preoperatively, as indicated by elevated TSH, are likely to deteriorate. Therefore, a "normal" preoperative TSH encompasses a wide range of thyroid status [4].
Thyroiditis is the end result of an inflammatory process caused by thyroid antigens and its antibodies [9] and subclinical thyroiditis is predictable through ATA and AMA [10]. Although the presence of histologic thyroiditis in the resected specimens was not significant in post-lobectomy hypothyroidism patients (P = 0.063), we reviewed preoperative TG, ATA, and AMA in all patients. Their quantitative titers were not significant, and positivity was defined as follows: TG > 60 ng/mL, ATA > 120 IU/mL, and AMA above 35 U/mL. Categorical analysis of two or more positivity of these three markers - serologic thyroiditis - was significantly higher in hypothyroid than euthyroid patients (28.6% vs. 3.9%, P = 0.024) (Table 2).
The relationship between post-lobectomy hypothyroidism and several clinicopathologic factors among the 123 patients were analyzed through multivariate analysis. The incidence of post-lobectomy hypothyroidism is significantly higher in those with higher preoperative TSH between 2.0 and 5.9 mIU/L (P = 0.008, odds ratio [OR] = 4.749) and patients with two or more positivity on preoperative TG, ATA, and AMA (P = 0.006, OR = 9.492) (Table 3). These were independent predictive factors of hypothyroidism after thyroid lobectomy. In addition, the combined positivity of preoperative TSH between 2.0 and 5.9 mIU/L and two or more positivity of TG, ATA, and AMA exhibited 100% positive predictive value and 80.8% negative predictive value (Table 4). It should be emphasized that these factors can be clearly identified preoperatively.
In the past, we recommended routine TSH monitoring at 3, 6, and one year after surgery, then once or twice a year thereafter. Most new onset hypothyroidism is observed in routine screening at 3, 6 months and 1 year after surgery, and 72% of patients were diagnosed by one year and 96% by two years. However, 29% of patients (10% at 3 months, 5% at 9 months, and 14% at 18 months) experienced overt clinical hypothyroidism, and all these patients had high normal TSH and two or more positivity on TG, ATA, and AMA (Fig. 1).
Many studies have attempted to evaluate the incidence and risk factors for hypothyroidism following thyroid lobectomy and hemi-thyroidectomy. Many studies have reported an incidence between 10.9 and 36.3% [1-4,12-15]. Various risk factors, such as age, high TSH levels, lower free T4 levels, presence of thyroid antibodies, and histologic thyroiditis have been reported. If pre-surgical predictive factors can be identified, patients' thyroid status will be optimally managed after surgery. However, there exists only one report on a preoperative predictive study. Tomoda et al. [5] suggested a predictive scoring system by using preoperative TSH levels and age. Other studies did not predicted hypothyroidism after thyroid lobectomy before surgery.
A prevalence of 21.1% of post-lobectomy hypothyroidism is comparable to that of previous studies [4,5,8], and high normal preoperative TSH levels between 2.0 and 5.9 mIU/L and two or more positivity on TG, ATA and AMA clearly increased the risk of hypothyroidism after thyroid lobectomy. Many studies reported that hypothyroid patients after lobectomy have higher preoperative TSH when compared with euthyroid patients [6,12]. A preoperative TSH levels were lower side distribution in euthyroid group, and evenly and slightly higher side distributed in hypothyroid group. The cut-off value was 2.0 mIU/L, with 66.6% sensitivity and 75.0% specificity, with area under curve was 0.841, 95% CI: 0.758 to 0.923 for the prediction of post-lobectomy hypothyroidism (Table 2).
In contrast to previous studies, age, sex, isthmusectomy, laterality of lobectomy and histologic thyroiditis were not significant factors for post-lobectomy hypothyroidism. In histologic thyroiditis, circulating auto-antibodies were initially thought to be the cause of the inflammatory process, but thyroiditis do not necessarily correlate with the level of circulating antibodies [9]. It appears as an end result of serologic thyroiditis - increased inflammatory process by circulating antibodies - and predictable by TG, ATA, and AMA [10]. It was significant at 67% sensitivity and 83% specificity to predict post-lobectomy hypothyroidism through TG, ATA, and AMA in our study. In contrast to histologic thyroiditis [2,4,15], we are able to obtain the results of serologic thyroiditis before surgery.
The mean age of the postoperative hypothyroid group was 40.1 years, compared with 40.2 years of the postoperative euthyroid group. Although hypothyroidism is more prevalent among elderly patients [16], our study did not find old age to be a risk factor for the development of hypothyroidism.
In benign thyroid conditions surgeons try to leave as much remnant thyroid tissues as possible, including the isthmus [17]. More thyroid tissue is ablated and harvested in endoscopic thyroid lobectomy. For comport handling of endoscopic procedure, isthmus usually transected beyond the centerline of trachea, and grasped and tracted with endoscopic forceps. All of isthmusectomy of hypothyroid group was endoscopic approach. Endoscopic thyroid lobectomy was slightly more common in hypothyroid (23.8% vs. 10.5%) patients albeit without significance (P = 0.203). Likewise for isthmusectomy (P = 0.191).
We recommended patients to evaluate their thyroid function at 3, 6 months, and 1 year after surgery, then once or twice a year thereafter for low risk patients. Additional thyroid function monitoring at 2 and 9 months was optional for high-risk patients. All patients were educated with symptoms of hypothyroidism, and most patients endured hypothyroidism with TSH higher than 10 IU/mL without experiencing serious symptoms. However, 29% of patients experienced overt clinical hypothyroidism. As such, we recently added TSH at 1, 9, and 18 months of follow-up as routine monitoring for high risk patients, such as preoperative TSH between 2.0 and 5.9 mIU/L, and two or more positivity of TG, ATA, and AMA.
This study is limited by its retrospective nature and asymptomatic subclinical hypothyroid patients - normal T3 and free T4 levels but 6 mIU/L or higher TSH levels - was defined as hypothyroid and required thyroid replacement therapy. To support this, there was significant rise in postoperative TSH that peaked at 1 to 2 months. TSH levels in patients not treated with levothyroxine was the lowest at 3 months and increased subsequently [5]. Also, some patients with asymptomatic subclinical hypothyroidism were delayed for thyroid replacement. Tracking thyroid function tests were performed after 1 month but all experienced clinical hypothyroidism.
In conclusion, patients who undergo thyroid lobectomy should be counseled for thyroid replacement therapy [4,5,8]. This is significantly higher than those who have high normal preoperative TSH levels and who have two or more positivity on TG, ATA, and AMA. And these were independent predictive factors of hypothyroidism after thyroid lobectomy. The combined positivity of them had 100% positive predictive value and 80.8% negative predictive value. We recommend patient to evaluate their thyroid function at 3 and 6 months, and 1 year after surgery for low risk patients. Additional TSH monitoring at 1, 9, and 18 months should be performed for high-risk patients.
Figures and Tables
Fig. 1
Time course of hypothyroidism after thyroid lobectomy. Routine thyroid function test monitoring was performed at 3, 6, 12, 18th month after surgery. About 10%, 5% and 14% of patients experienced overt clinical hypothyroidism at 3, 9 and 18 months respectively.

References
1. Niepomniszcze H, Garcia A, Faure E, Castellanos A, del Carmen Zalazar M, Bur G, et al. Long-term follow-up of contralateral lobe in patients hemithyroidectomized for solitary follicular adenoma. Clin Endocrinol (Oxf). 2001. 55:509–513.
2. Buchanan MA, Lee D. Thyroid auto-antibodies, lymphocytic infiltration and the development of post-operative hypothyroidism following hemithyroidectomy for non-toxic nodular goitre. J R Coll Surg Edinb. 2001. 46:86–90.
3. Seiberling KA, Dutra JC, Bajaramovic S. Hypothyroidism following hemithyroidectomy for benign nontoxic thyroid disease. Ear Nose Throat J. 2007. 86:295–299.
4. Su SY, Grodski S, Serpell JW. Hypothyroidism following hemithyroidectomy: a retrospective review. Ann Surg. 2009. 250:991–994.
5. Tomoda C, Ito Y, Kobayashi K, Miya A, Miyauchi A. Subclinical hypothyroidism following hemithyroidectomy: a simple risk-scoring system using age and preoperative thyrotropin level. ORL J Otorhinolaryngol Relat Spec. 2011. 73:68–71.
6. Miller FR, Paulson D, Prihoda TJ, Otto RA. Risk factors for the development of hypothyroidism after hemithyroidectomy. Arch Otolaryngol Head Neck Surg. 2006. 132:36–38.
7. Stoll SJ, Pitt SC, Liu J, Schaefer S, Sippel RS, Chen H. Thyroid hormone replacement after thyroid lobectomy. Surgery. 2009. 146:554–558.
8. Moon HG, Jung EJ, Park ST, Jung TS, Jeong CY, Ju YT, et al. Thyrotropin level and thyroid volume for prediction of hypothyroidism following hemithyroidectomy in an Asian patient cohort. World J Surg. 2008. 32:2503–2508.
9. De Groot LJ, Hall R, McDermott WV, Davis AM. Hashimoto's thyroiditis. A genetically conditioned disease. N Engl J Med. 1962. 267:267–273.
10. Arai T, Kurashima C, Utsuyama M, Sawabe M, Ito H. Measurement of anti-thyroglobulin and anti-thyroid peroxidase antibodies using highly sensitive radioimmunoassay: an effective method for detecting asymptomatic focal lymphocytic thyroiditis in the elderly. Endocr J. 2000. 47:575–582.
11. Williams ED, Doniach I. The post-mortem incidence of focal thyroiditis. J Pathol Bacteriol. 1962. 83:255–264.
12. McHenry CR, Slusarczyk SJ. Hypothyroidisim following hemithyroidectomy: incidence, risk factors, and management. Surgery. 2000. 128:994–998.
13. Griffiths NJ, Murley RS, Gulin R, Simpson RD, Woods TF, Burnett D. Thyroid function following partial thyroidectomy. Br J Surg. 1974. 61:626–632.
14. De Carlucci D Jr, Tavares MR, Obara MT, Martins LA, Hojaij FC, Cernea CR. Thyroid function after unilateral total lobectomy: risk factors for postoperative hypothyroidism. Arch Otolaryngol Head Neck Surg. 2008. 134:1076–1079.
15. Piper HG, Bugis SP, Wilkins GE, Walker BA, Wiseman S, Baliski CR. Detecting and defining hypothyroidism after hemithyroidectomy. Am J Surg. 2005. 189:587–591.
16. Woeber KA. Subclinical thyroid dysfunction. Arch Intern Med. 1997. 157:1065–1068.
17. Kim HS, Kwon DS, Kim JS, Moon DJ. A clinical analysis of endoscopic thyroid lobectomy and comparison with conventional thyroid lobectomy. J Korean Surg Soc. 2005. 69:450–454.




 ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download