Abstract
Purpose
Laparoscopic appendectomy has been recognized to have many advantages such as greater cosmetic results, less postoperative pain and shorter hospital stays. On the other hand, the cost of laparoscopic procedures is still more expensive than that of open procedures in Korea. The aim of this study is to compare clinical outcomes and hospital costs between open appendectomy and laparoscopic appendectomy.
Methods
Between January 1, 2010 and December 31, 2010, 471 patients were diagnosed with acute appendicitis. Of these, 418 patients met the inclusion criteria and were divided into two groups of open appendectomy (OA) group and laparoscopic appendectomy (LA) group. We analyzed the clinical data and hospital costs.
Results
The mean operation time for laparoscopic appendectomy (72.17 minutes) was significantly longer than that of open appendectomy (46.26 minutes) (P = 0.0004). The mean amounts of intravenous analgesics for OA group (2.00 times) was greater than that of LA group (1.86 times) (P < 0.0001). The complication rate was similar between the two groups (OA, 6.99% vs. LA, 10.87%; P = 0.3662). The mean length of postoperative hospital stay was shorter in LA group (OA, 4.55 days vs. LA, 3.60 days; P = 0.0002). The mean total cost covered by the National Health Insurance was more expensive in LA group (OA, 1,259,842 won [Korean monetary unit] vs. LA, 1,664,367 won; P = 0.0057).
Conclusion
Clinical outcomes of laparoscopic appendectomy were superior to that of open appendectomy even though the cost of laparoscopic appendectomy was more expensive than that of open appendectomy. Whenever surgeons manage a patient with appendicitis, laparoscopic appendectomy should be considered as the procedure of choice.
Acute appendicitis is the most common intra-abdominal condition requiring emergency surgery [1]. Open appendectomy was the principal procedure in treating a patient with appendicitis until the emergence of laparoscopic devices. Mostly, open appendectomy was performed successfully through a relatively small skin incision, patients had less pain and returned to work earlier as compared to other surgical procedures.
Since Semm [2] described the first laparoscopic appendectomy in 1983, laparoscopic surgical procedures have been popular in almost all surgical fields. Moreover, recently, single-port laparoscopic appendectomy was introduced and has become popular at some hospitals [3,4].
Laparoscopic appendectomy has been recognized to have many advantages such as greater cosmetic results, less postoperative pain and shorter hospital stays [5-10]. On the other hand, the cost of laparoscopic procedures is still more expensive than that of open procedure in Korea.
The aim of this study is to compare the clinical outcomes and the hospital costs between open appendectomy and laparoscopic appendectomy.
The present study was designed as a retrospective, observational study in a single institute. Between January 1, 2010 and December 31, 2010, 471 patients were diagnosed with acute appendicitis. We excluded cases that underwent extended procedures like ileocecectomy or combined other surgical procedure like cholecystectomy and oophorectomy. Also, pregnant women and patients with severe medical disease requiring intensive care or expensive medical procedures were excluded. Patients who underwent surgical procedure by residents were also excluded. Eight surgeons performed surgical procedures for all cases during the last year. In our hospital, the operative procedure was chosen by patients who received enough informed consent about the procedure. 418 patients met the inclusion criteria and we analyzed the clinical data and hospital costs. The patients were divided into two groups of open appendectomy (OA) group and laparoscopic appendectomy (LA) group. The collected clinical data included demographic data, diagnostic tool, preoperative diagnosis, initial body temperature, initial laboratory finding, operation time, time to soft diet, postoperative hospital stay, amount of analgesics, pathologic result and complication. Hospital costs consisted of the total amount of health benefit and charge for non-covered items, for example, uncovered bed charge or non-covered materials. We analyzed data on cost separately; total hospital cost, total covered cost by National Health Insurance (NHI) and copayment by a patient.
Data were analyzed using the statistical software SAS ver. 4.2 (SAS Inc., Cary, NC, USA). Data are expressed as numbers (%) and mean (standard deviation). The results were analyzed using the chi-square analysis or Fisher's exact test for discrete data and student t-test for continuous numeric data. Statistical significance was accepted at the P < 0.05 level.
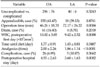
Table 1 shows the demographic data and preoperative clinical feature between OA group and LA group. 372 patients underwent open appendectomy and 46 patients underwent laparoscopic appendectomy. Patients' body mass index, initial body temperature and initial white blood cell (WBC) count did not show difference between the two groups. But, female predominance was observed in LA group (P = 0.0027), and slightly younger age of patients was revealed in the group (P = 0.0185).
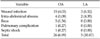
All patients with suspicious appendicitis underwent radiologic evaluation, either computed tomography or ultrasonography, and preoperative diagnosis was made (Table 2). Comparison of the ratio of complicated appendicitis, accompanied by appendicolith and time to soft diet did not show any difference (Table 3). The operation time for laparoscopic appendectomy was significantly longer than that of open appendectomy (P = 0.0004). The ratio of accompanying external drainage procedure of OA group (16.4%) was slightly higher than that of LA group (8.7%), but there was no statistical difference. The WBC count at first postoperative day of LA group was lower than that of OA group (P = 0.0008). The amounts of intravenous analgesics of OA group was more than that of LA group (P < 0.0001). The complication rate observed in LA group (10.87%) was slightly higher than that in OA group (6.99%), but there was no statistical difference. The length of postoperative hospital stay was shorter in LA group (P = 0.0002).
Surgical wound infection was the most common complication in both groups (Table 4). Umbilical port site insertion was the most commonly infected site in LA group. Intra-abdominal abscess occurred in 6 cases in both groups (Table 5).
Analysis of hospital costs presented interesting but confusing results (Table 6). The total hospital cost and copayment by a patient of the LA group were more expensive than those of the OA group, but there were no statistical difference. The total cost covered by NHI was more expensive in LA group, and significant difference was shown (P = 0.0057).
In 1886, acute appendicitis was revealed to be the first causative of right lower quadrant pain by Fitz, and surgical treatments at the time of diagnosis became the common treatment mode [11].
Laparoscopic appendectomy has many advantages such as cosmetic effect, less pain and shorter hospital stay [5-10], but the debate over OA versus LA remains contentious, with more than 100 articles written on the topic [12].
Radiologic evaluation could help surgeons to confirm the diagnosis and to recognize the location of appendix, and/or other intra-abdominal conditions requiring other procedures. If the radiologic finding is vague, we recommended operation considering clinical features like fever, leukocytosis, and typical migration pain from epigastrium to right lower quadrant after a short-term observational period.
Eight surgeons were involved in our series; two surgeons did not perform laparoscopic appendectomy. There was no conversion case from laparoscopic appendectomy to open appendectomy.
The number of patients who underwent laparoscopic appendectomy was much smaller than that of patients who underwent open appendectomy. This result might be due to the fact that the patients tended to have incomplete information and distorted knowledge about the advantages and disadvantages of the laparoscopic procedure from unauthorized resources. Secondly, surgeons preferred open procedure to laparoscopic procedure when the appendicitis seemed to have severe inflammation or seemed to be perforated.
The present study revealed that the LA group was younger and had female predominance. We thought this result was mainly due to the cosmetic advantage.
The operation time of LA group was longer than that of OA group and it was similar with the meta-analysis [13,14]. Because all six surgeons had experience of over 30 cases by laparoscopic procedure each, we believe that the longer operation time of laparoscopic appendectomy was not associated with technical inexperience.
In the view of clinical outcomes, laparoscopic appendectomy was safe and technically feasible and it shortened hospital stay. Therefore, the result of the procedure was superior to that of open appendectomy.
The present study revealed the same results on the length of hospital stay and amount of analgesics. But, compared with OA group, the complication rate in LA group was slightly higher even though there was no significant difference. We assumed that the result of complication rates was associated with the relatively small sample size in LA group. Among these complications, intra-abdominal abscess was the most serious complication because it sometimes required either intervention or re-laparotomy. In our series, 6 cases developed intra-abdominal abscess. They were successfully treated by non-operative methods, using antibiotics or percutaneous drainage. This is a similar result to the literature reported by Ingraham et al. [15].
During short-term follow up, we did not observe either post-operative paralytic ileus or intestinal obstruction in LA group, whereas 5 cases of intestinal obstruction occurred in OA group. The reason for lower post-operative ileus occurrence in LA group was thought to be due to laparoscopic procedure reducing interference to the microenvironment and injury to the intestinal serous membrane, then lightened the adherence between the intestines [13]. But, in the literature, there was no statistically significant difference of small bowel obstruction between the two groups [14]. A long observational period is required to assess intestinal obstruction between the two groups.
Between OA and LA, in the literature, there was no significant difference in cost, or, hospital costs were incomparable [13,14]. Comparing costs with other countries between the two groups is difficult because of the difference in health care systems and health insurance. The present study revealed that LA was more expensive than OA in the total cost covered by NHI. But, no significant difference was found for copayment by a patient. The reason for this misconception is that the patient only pays 20 percent of the insurance fee in Korea. When the procedure was chosen, the difference of cost must be considered by surgeon and patient. If the patient is not covered by NHI, we would recommend open appendectomy.
The literature has shown that laparoscopic appendectomy is a safe and clinically beneficial operating procedure even in patients with peritonitis, perforation, and abscess [7]. We could not compare the clinical outcomes and hospital cost between uncomplicated appendicitis and complicated appendicitis due to the small sample size of patients with complicated appendicitis in LA group. We felt it was a limitation in our series but an inevitable selection to compare the clinical outcomes and hospital cost simultaneously.
The clinical outcomes of laparoscopic appendectomy were superior to that of open appendectomy even though the cost of laparoscopic appendectomy was higher than that of open appendectomy. Whenever a surgeon manages a patient with appendicitis, laparoscopic appendectomy should be considered as procedure of choice.
Figures and Tables
References
1. Park JH, Hyun KH, Park CH, Choi SY, Choi WH, Kim DJ, et al. Laparoscopic vs transumbilical single-port laparoscopic appendectomy: results of prospective randomized trial. J Korean Surg Soc. 2010. 78:213–218.
2. Semm K. Endoscopic appendectomy. Endoscopy. 1983. 15:59–64.
3. Kim HJ, Lee JI, Lee SC, Kim SH, Lee IK, Lee YS, et al. Single-port laparoscopic appendectomy. J Korean Surg Soc. 2010. 78:338–342.
4. Hong YH, Sohn TJ, Oh SJ, Chang YS, Kang JH, Kim DH, et al. Comparison of single port and conventional laparoscopic surgery in acute appendicitis. J Korean Soc Endosc Laparosc Surg. 2010. 13:102–106.
5. Park JY, Choe YM, Yun MY, Choi SK, Hur YS, Lee KY, et al. Laparoscopic versus open appendectomy for perforated appendicitis in children. J Korean Surg Soc. 2008. 75:116–119.
6. Park JM, Kim J, Kim CY, Choi DJ, Kim SH, Kim CS, et al. Laparoscopic appendectomy: a safe procedure that can be performed by surgical residents. J Korean Surg Soc. 2008. 75:315–322.
7. Jun YW, Jung H, Kim SJ, Jun KH, Chin HM, Park WB. Comparison of clinical outcomes between laparoscopic and open appendectomy: a retrospective analysis of 2,745 patients. J Korean Surg Soc. 2009. 77:320–325.
8. Seo K, Choi Y, Choi J, Yoon K. Laparoscopic appendectomy is feasible for inexperienced surgeons in the early days of individual laparoscopic training courses. J Korean Surg Soc. 2009. 76:23–27.
9. Park SS, Kim HS, Ryu BY, Kim HK, Lee JH, Lee JW, et al. Laparoscopic versus open appendectomy for complicated appendicitis. J Korean Soc Endosc Laparosc Surg. 2010. 13:69–73.
10. Yang YJ, Kim ID, Kim KH, Park JS, Suh BS, Kim SW, et al. Comparsion of laparoscopic appendectomy vs open appendectomy in non-complicated appendicitis and complicated appendicitis. J Korean Soc Endosc Laparosc Surg. 2010. 13:74–79.
11. John MA, Kimberly SK. Townsend CM, Beauchamp RD, Evers BM, Mattox KL, editors. The appendix. Textbook of surgery: the biological basis of modern surgical practice. 2008. 18th ed. Philadelphia: W.B. Saunders;917–973.
12. Clarke T, Katkhouda N, Mason RJ, Cheng BC, Olasky J, Sohn HJ, et al. Laparoscopic versus open appendectomy for the obese patient: a subset analysis from a prospective, randomized, double-blind study. Surg Endosc. 2011. 25:1276–1280.
13. Wei B, Qi CL, Chen TF, Zheng ZH, Huang JL, Hu BG, et al. Laparoscopic versus open appendectomy for acute appendicitis: a metaanalysis. Surg Endosc. 2011. 25:1199–1208.
14. Liu Z, Zhang P, Ma Y, Chen H, Zhou Y, Zhang M, et al. Laparoscopy or not: a meta-analysis of the surgical effects of laparoscopic versus open appendicectomy. Surg Laparosc Endosc Percutan Tech. 2010. 20:362–370.
15. Ingraham AM, Cohen ME, Bilimoria KY, Pritts TA, Ko CY, Esposito TJ. Comparison of outcomes after laparoscopic versus open appendectomy for acute appendicitis at 222 ACS NSQIP hospitals. Surgery. 2010. 148:625–635.




 ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download