Abstract
Purpose
Although several reports have been published regarding the coexistence of hyperparathyroidism and papillary thyroid carcinomas, concurrence of parathyroid adenoma and papillary thyroid carcinoma is extremely rare. The aim of this study was to describe experiences with concurrent parathyroid adenoma and papillary thyroid carcinoma.
Methods
Seven patients with concurrent parathyroid adenoma and papillary thyroid carcinoma were identified between January 2006 and December 2007, and their medical records were reviewed retrospectively.
Results
Of the seven patients identified, three were male and four were female; their mean age was 53.6 years. None of the patients presented with symptomatic hyperparathyroidism preoperatively. On laboratory findings, four patients had mild to moderate hypercalcemia, but serum parathyroid hormone concentrations were high in all patients. Preoperative imaging showed suspicious features of diseased parathyroid glands in four patients; two upon ultrasonography and computed tomography together and two upon ultrasonography only. The coexistence of parathyroid adenoma did not affect the extent of thyroid surgery. Laboratory values after surgery returned to within normal ranges in all patients.
Primary hyperparathyroidism is present in up to 0.1% of the general population, and it is clinically recognized in patients presenting with hypercalcemia or as a part of multiple endocrine neoplasia (MEN) types I and IIa [1]. Although there have been sporadic reports of the coexistence of hyperparathyroidism and non-medullary thyroid carcinoma [2], concurrence of parathyroid adenoma and papillary thyroid carcinoma is extremely rare. In most reports discussing the coexistence of these two diseases, primary hyperparathyroidism was diagnosed before the identification of the thyroid carcinoma which was usually diagnosed in a pathology specimens [3,4]. Since the coexistence of both disease processes can complicate patient management via untreated hypercalcemia, unrecognized thyroid cancer, and the necessity of re-operative neck surgery, patients should be screened for both disease entities carefully.
The aim of this study was to describe our experiences with concurrent parathyroid adenoma and papillary thyroid carcinoma in a same patient.
Of the 3,137 patients who underwent thyroid cancer surgery at the Thyroid Cancer Center, Department of Surgery, Yonsei University College of Medicine between January 2006 and December 2007, seven patients (0.2%) who had concurrent parathyroid adenoma and papillary thyroid carcinoma. Information regarding patient demographics, biochemical concentrations, tumor pathologic findings, extent of surgery, and postoperative complications was extracted from the medical records and reviewed retrospectively. Written informed consents of each patient were obtained from the each patient for publication of this article.
The clinicopathologic characteristics of the patients are listed in Table 1. Of the seven patients, 3 (42.9%) were male and 4 (57.1%) were female. The mean age of the patients was 53.6 years (range, 27 to 73 years). None of patients had a history of head and neck irradiation or prior neck surgery. One patient had a history of hyperthyroidism, and two patients had histories of hypertension treated with anti-hypertensive agents.
All patients presented with thyroid nodules detected by medical check-ups and none of the seven patients were initially seen for symptomatic hypercalcemia. On preoperative laboratory findings, four patients had mild to moderate hypercalcemia, while the others had normal serum calcium concentrations. The mean serum calcium concentration was 11.4 mg/dL (range, 9.6 to 15.0 mg/dL). All seven patients had normal serum phosphorus concentrations with a mean concentration of 3.2 mg/dL (range, 2.5 to 4.5 mg/dL). Intact parathyroid hormone (iPTH) concentrations were high in all patients, with a mean concentration of 100.90 pg/mL (range, 57.44 to 159.51 pg/mL).
Laboratory values after surgery were within normal ranges in all patients: 9.0 mg/dL (range, 8.5 to 10.1 mg/dL) for calcium concentrations: 3.5 mg/dL (range, 2.3 to 4.5 mg/dL) for phosphorus concentrations; and 9.34 pg/mL (range, 1.48 to 28.49 pg/mL) for iPTH concentration (Fig. 1).
During the preoperative evaluations for thyroid disease, neck ultrasonography and computed tomography scans were performed on all patients. Four patients were suspected to have diseased parathyroid glands; two were detected by ultrasonography and computed tomography and two by ultrasonography only.
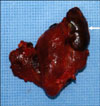
A total thyroidectomy was performed in six patients with thyroid carcinomas and a less-than-total thyroidectomy was performed in one patient (Fig. 2). Central node dissection was performed in all patients, and lateral neck dissection was not performed in any of patients. The coexistence of parathyroid adenoma did not affect the extent of thyroid surgery.
The mean size of the thyroid carcinoma was 1.01 cm (range, 0.2 to 2.7 cm), and four cases showed metastatic lymph nodes in the central compartment.
In regard to complications, postoperative transient hypocalcemia occurred in three patients, and the symptoms were relieved within three months. Except for the development of seroma in one patient, no other complications occurred.
Since synchronous thyroid and parathyroid disease was first described in 1947 [5], the incidence of thyroid disease in patients undergoing parathyroidectomy has been reported to be from 2.5 to 17.6%. Conversely, the frequency of primary hyperparathyroidism in patients with thyroid disease has been reported to range from 0.3 to 8.7% [2].
The frequency of coexistence of primary hyperparathyroidism and thyroid carcinoma is not well-known; only two studies have been conducted and have reported frequencies of 3.7% and 8.0% [3,4]. In the present study, primary hyperparathyroidism was diagnosed prior to the thyroid carcinomas, and the thyroid carcinomas were diagnosed from pathology specimens [3,4].
In the present series, primary hyperparathyroidism was 0.2% of the patients with thyroid carcinoma. As different from the previous studies, the thyroid carcinoma was diagnosed prior to the diagnosis of primary hyperparathyroidism, and primary hyperparathyroidism was postoperatively diagnosed in the pathology specimens. To our knowledge, there is only one similar case report [6].
The pathogenesis of primary hyperparathyroidism and thyroid carcinoma coexistence has not been established. The oncogenic effect of hypercalcemia on the thyroid gland has been assumed [7], and low-dose radiation therapy for the head and neck, especially in childhood and adolescence, is known to induce thyroid and parathyroid tumors [8,9]. In the present series, however, none of the patients showed severe hypercalcemia, and only four patients had mild to moderate clinically diagnosed hypercalcemia. Thus, the oncogenic effect of hypercalcemia was not applicable in the present series. No patients had a history of prior neck irradiation.
The occasional coexistence of papillary thyroid carcinoma and primary hyperparathyroidism may result in a discrepancy between the clinical impression and the fine needle aspiration (FNA) cytology diagnosis, leading to the possibility of a false-positive FNA cytology diagnosis [10]. The final diagnosis of concurrent parathyroid adenoma and thyroid carcinoma can be established on postoperative histopathologic examinations [11]. In the present series, four patients were suspicious for coexisting parathyroid disease, and the confirmations of these concurrences were made using the final histopathologic results. Coexistence of parathyroid disease had no influence on the surgical extent of thyroid cancer, and thyroid surgeries in our series were performed based on the international guidelines in our series [12]. Additional resections for the diseased parathyroid glands were performed.
In conclusion, although concurrent parathyroid adenoma and thyroid carcinoma is rare, they can and do coexist. Preoperative biochemical studies, including serum calcium and iPTH concentrations, may be helpful to evaluate for occult primary hyperparathyroidism, and appropriate treatment for the parathyroid pathology including surgical resection should be performed for the prevention of the adverse disease resulted from the untreated parathyroid disease post-thyroidectomy period. Furthermore, when a patient with thyroid cancer is diagnosed, a routine checkup for serum calcium is mandated after the removal of concomitant parathyroid lesion and iPTH is considered as useful method to confirm and screen the hypercalcemia.
Figures and Tables
References
1. Silverberg SJ, Bilezikian JP. Asymptomatic primary hyperparathyroidism: a medical perspective. Surg Clin North Am. 2004. 84:787–801.
2. Morita SY, Somervell H, Umbricht CB, Dackiw AP, Zeiger MA. Evaluation for concomitant thyroid nodules and primary hyperparathyroidism in patients undergoing parathyroidectomy or thyroidectomy. Surgery. 2008. 144:862–866.
3. Krause U, Olbricht T, Metz K, Rudy T, Benker G. Coincidence of non-medullary thyroid cancer and hyperparathyroidism. Chirurg. 1991. 62:536–539.
4. Calcaterra TC, Paglia D. The coexistence of parathyroid adenoma and thyroid carcinoma. Laryngoscope. 1979. 89(7 Pt 1):1166–1169.
5. Kissin M, Bakst H. Co-existing myxedema and hyperparathyroidism; case report. J Clin Endocrinol Metab. 1947. 7:152–158.
6. Sakata S, Fuwa Y, Komaki T, Tarao M, Takuno H, Miura K. A case of papillary carcinoma of the thyroid associated with parathyroid adenoma without hyperparathyroidism. Intern Med. 1992. 31:459–462.
7. Ho KJ. Papillary parathyroid adenoma. A rare occurrence and its importance in differentiation from papillary carcinoma of the thyroid. Arch Pathol Lab Med. 1996. 120:883–884.
8. Stephen AE, Chen KT, Milas M, Siperstein AE. The coming of age of radiation-induced hyperparathyroidism: evolving patterns of thyroid and parathyroid disease after head and neck irradiation. Surgery. 2004. 136:1143–1153.
9. De Jong SA, Demeter JG, Jarosz H, Lawrence AM, Paloyan E. Thyroid carcinoma and hyperparathyroidism after radiation therapy for adolescent acne vulgaris. Surgery. 1991. 110:691–695.
10. Beecham JE. Coexistent disease as a complicating factor in the fine needle aspiration diagnosis of papillary carcinoma of the thyroid. Acta Cytol. 1986. 30:435–438.
11. Friedman M, Shimaoka K, Lopez CA, Shedd DP. Parathyroid adenoma diagnosed as papillary carcinoma of thyroid on needle aspiration smears. Acta Cytol. 1983. 27:337–340.
12. Cooper DS, Doherty GM, Haugen BR, Kloos RT, Lee SL, Mandel SJ, et al. Management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid. 2006. 16:109–142.




 ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download