Abstract
A 33-year-old woman was admitted to our hospital with a slow-growing mass in the left side of her neck. The mass was found to be a huge (73 × 56 × 54 mm) carotid body paraganglioma. Another 21 mm-size tumor was incidentally detected at the right carotid bifurcation. She had hoarseness and Horner's syndrome of her left side. Both tumors were surgically removed. There were no cerebrovascular complications but some neurologic complications occurred when the left tumor was removed.
Carotid body paraganglioma is a tumor arising from paraganglionic tissue at the bifurcation of the common carotid artery. The treatment of choice is surgical resection. In 1953, Linder [1] classified the tumors of the carotid body and about 20 years later (1971), Shamblin et al. [2] repeated the same classification based on the size and involvement of the carotid artery. Group 1 or 2 tumors are usually not problematic to surgical resection. However, surgery is very challenging for group 3 tumors that have an intimate adherent relationship to the entire circumference of the carotid bifurcation. We report a case of bilateral carotid body paragangliomas that were Shamblin group 3 and 1, respectively.
A 33-year-old woman was referred to the department of vascular surgery for left side neck swelling. She was manifesting a non-tender, slightly movable, approximately 6 cm-sized, soft mass in the left side of her neck. The mass was discovered 15 years ago and grew slowly. She wanted to evaluate the mass because her voice had changed a year prior and the mass became a cosmetic problem. She was a non-smoker and had never been in high-altitude areas. There was no family history with similar symptoms. Blood pressure, pulse rate, body temperature and respiration rate were within the normal range. Her voice had changed over the last year and had become aggravated. On laryngoscopy, movement of the left vocal cord was slightly limited. Her left pupil was slightly more contracted than the right pupil. Other neurologic examinations were unremarkable. Her arterial blood gas analysis, serum electrolytes and other laboratory test were unremarkable at admission.
On imaging evaluation, the computed tomogram (CT) scan showed a well enhanced, lobular contoured mass located at the left carotid bifurcation and also revealed a similar tumor at the right carotid bifurcation (Fig. 1). Magnetic resonance imaging revealed an enhanced mass with maximal diameter of 7.3 cm (7.3 × 5.6 × 5.4 cm) encircling the ipsilateral common carotid artery (CCA), internal carotid artery (ICA) and external carotid artery (ECA) (Fig. 2). The left side tumor was diagnosed as carotid body paraganglioma of Shamblin group 3 and the right side tumor was group 1. Horner's syndrome of the left side due to tumor encasement of the left vagus nerve was also suspected. Digital subtraction angiography showed hypervascular lesions at both carotid bifurcations with multiple feeders from CCA, ICA and ECA. The selective embolization for the left side tumor was impossible because we failed to select the feeder arteries (Fig. 2).
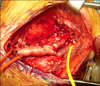
The left-side tumor was removed and involved ECA segment, vagus nerve segment, and sympathetic nerve segment were also resected simultaneously. The hypoglossal nerve could not be identified during surgery. The tumor was attached tightly at carotid bifurcation, so some part of ICA wall was removed with tumor and ICA was reconstructed by remnant ECA segment patch (Figs. 3, 4). Transient shunt was not used during the ICA reconstruction. Swallowing difficulty developed with left-side tongue atrophy and Horner's syndrome was aggravated after the surgery. On laryngoscopic examination, left-side vocal cord paralysis was aggravated. There was no evidence of brain infarction after the surgery. Four months after the surgery, she could swallow without aspiration by specific movement on swallowing and the difference in pupil size decreased.
Carotid body paraganglioma (CBP) is rare and usually benign. However, complete surgical resection is recommended because of the unpredictable malignancy potentials. Early excision is also mandatory because resection can be technically difficult or may result in neurovascular complications, especially for large size and Shamblin group 3 tumors [3]. In our case, with the left-side tumor, which was Shamblin group 3, swallowing difficulty persisted after surgery while the right-side tumor (group 1) was removed without any complication.
Early detection of the small tumor is very difficult because of poor clinical symptoms during its small size phase. Neurovascular symptoms and signs, such as hoarseness, vocal cord paralysis, otalgia, dysphasia, Horner's syndrome, pulsation, a thrill or a bruit, cerebral ischemia, or carotid sinus syndrome are present in large tumor or Shamblin group 3. In this case, the left side tumor had neurologic symptoms, hoarseness and Horner's syndrome but the right side tumor was detected incidentally.
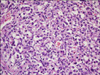
The histological appearance of a CBP is not reliable to differentiate for malignancy and the majority of authors agree that the only proof of malignancy is the presence of metastasis [3]. Needle biopsy to confirm diagnosis should be avoided because of high vascularity of the lesion. CT scan with contrast and magnetic resonance image are useful modalities to identify CBP [4]. Angiography with selective embolization can be used for diagnosis when the diagnosis is unclear [5]. We tried selective embolization before surgery in order to reduce the size of tumor and bleeding complications but there are multiple arteries in tumor vascularization and many anastomoses between external and internal carotid arteries and tumor, thus we forfeited the pre-operative embolization. In huge CBPs, such as our case, superselective embolization is very difficult, thus the incidence of stroke is increased [6].
In surgical techniques, there are two areas needing special attention in dissection; one is the carotid bifurcation and the other is the superior pole of the tumor. Removal of CBPs is most difficult in the posterior face of the carotid bifurcation where the glomus artery originates. Among the post-operative complications, vascular insufficiency in the brain is the most serious complication so maintenance of cerebral blood flow is the most important thing during surgery and vascular reconstruction must be considered preoperatively. In our case, the left-side tumor was resected with part of posterior wall of carotid bifurcation and external carotid artery. The continuity from the common carotid artery to internal carotid artery was reconstructed by patch from a part of the external carotid artery. We prepared the transient shunt to maintain the cerebral blood flow but we did not have to use the shunt. There was no evidence of vascular insufficiency after surgery. Another difficult area is the superior pole of the tumors. In our left-side tumor, control of internal carotid artery was difficult and the tumor had involved the vagus nerve and the cervical sympathetic trunk. We couldn't identify the hypoglossal nerve in the left side. After the left side surgery, the patient suffered from swallowing difficulty, aggravated Horner's syndrome and hoarseness. A recent study reported that the crainocaudal technique in removing CBP made favorable results [7]. We applied this technique in our case but unfortunately could not prevent the neurologic complications. However, the right side tumor was removed completely without any complication.
In conclusion, despite the development of surgical and endovascular treatment, huge carotid body paraganglioma can make pre- and post-operative sequalae. Carotid body paraganglioma should be removed immediately upon detection. Because even if the tumor is not pathologically malignant, it will continue to grow and can cause various complications and the tumor will become too difficult for a surgeon to remove without complications.
Figures and Tables
Fig. 2
Magnetic resonance image. The left side mass surrounds the common, internal and externalcartoid arteries
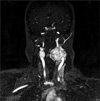
Fig. 3
Pre-operative finding of left side tumor. A huge hypervascular tumor surrounds the left common, internal and external carotid arteries.

References
1. Linder F. Tumoren der Karotisdrüse. Langenbecks Arch Chir Suppl Kongressbd. 1953. 276:156–162.
2. Shamblin WR, ReMine WH, Sheps SG, Harrison EG Jr. Carotid body tumor (chemodectoma). Clinicopathologic analysis of ninety cases. Am J Surg. 1971. 122:732–739.
3. Dimakakos PB, Kotsis TE. Carotid body paraganglioma: review and surgical management. Eur J Plast Surg. 2001. 24:58–65.
4. Carroll W, Stenson K, Stringer S. Malignant carotid body tumor. Head Neck. 2004. 26:301–306.
5. van den Berg R. Imaging and management of head and neck paragangliomas. Eur Radiol. 2005. 15:1310–1318.
6. Persky MS, Setton A, Niimi Y, Hartman J, Frank D, Berenstein A. Combined endovascular and surgical treatment of head and neck paragangliomas: a team approach. Head Neck. 2002. 24:423–431.
7. van der Bogt KE, Vrancken Peeters MP, van Baalen JM, Hamming JF. Resection of carotid body tumors: results of an evolving surgical technique. Ann Surg. 2008. 247:877–884.




 ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download