Abstract
Lumbar hernia is a rare surgical entity without a standard method of repair. With advancements in laparoscopic techniques, successful lumbar herniorrhaphy can be achieved by the creation of a completely extraperitoneal working space and secure fixation of a wide posterior mesh. We present a total extraperitoneal laparoendoscopic repair of lumbar hernia, which allowed for minimal invasiveness while providing excellent anatomical identification, easy mobilization of contents and wide secure mesh fixation. A total extraperitoneal method of lumbar hernia repair by laparoscopic approach is feasible and may be an ideal option.
Lumbar hernia in the flank is an uncommon type of ventral hernia. Anatomically, lumbar hernia involves both the intraperitoneal and retroperitoneal areas bounded superiorly by the 12th rib and inferiorly by the iliac crest. Its unique anatomical nature has made the diagnosis and proper repair of lumbar hernias a challenge. Since P. Barbette first suggested the existence of this entity in 1672, its management has been controversial. With more accurate body imaging techniques such as computed tomography (CT) scan and magnetic resonance imaging and improvements in laparoendoscopic techniques of hernia repairs with mesh there has been a lot of achievement in understanding and surgical treatment of lumbar hernia.
This report is the first laparoscopic totally extraperitoneal (TEP) approach to lumbar hernia in Korea.
A 76 year old woman with a history of left flank bulge for 6 months presented with left-sided back pain in the same area for two months. She had no previous surgery or trauma in that area. On physical examination she had a 6 × 5 cm reducible bulge at the posterolateral part of left flank below the 12th rib. A CT scan showed herniation of retroperitoneal fat and descending colon through the fascial defect at the left superior lumbar triangle (Fig. 1). We planned the laparoscopic TEP approach for herniorrhaphy of this superior lumbar hernia, Grynfeltt hernia.
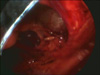
Under the general anesthesia the patient was placed in a full right lateral decubitus position with a lumbar roll in place. A 2 cm transverse incision was made over the hernia defect of the already reduced hernia which was below the 12th rib along the mid axillary line. The retroperitoneal fat was detached first with blunt dissection by an index finger and then with smooth instrument to create space in the retroperitoneal cavity. An 11 mm trocar was inserted and the space was expanded by a balloon dissector (Tyco Healthcare, Norwalk, CT, USA). Under the direct visualization with a 30° 10 mm scope, three 5 mm trocars were inserted anteriorly along the anterior axillary line approximately 5 cm apart (Fig. 2). Then, the 11 mm trocar was removed and the wound was plugged with gauze to maintain the pneumoretroperitoneum. With 30° 5 mm scope in the central port the retroperitoneal fat and structures were detached from the hernia defect and surrounding muscular-bony structures using 2 working ports above and below the central port (Fig. 3). A 15 × 15 cm octagonal polypropylene mesh (Fig. 4) was inserted through the reinserted 11 mm trocar previously used for space making and placed on the lumbar wall to cover at least 4 cm margin around the hernia defect. The mesh was then fixed with transfascial sutures of polypropylene at the center and the margins of each quadrant. To secure the mesh in place we used Tacker (Tyco Healthcare). The mesh was not fixed to the iliac crest or the 12th rib. Postoperative pain was controlled with injections of analgesic (non-steroidal anti-inflammatory drugs) until the postoperative second day. There was no seroma or other wound complication. She was discharged on the 5th day after the operation (Fig. 5). There was no evidence of recurrence on follow up at 11 months.
Lumbar hernia has infrequently been reported with only about 300 cases in the English literature, 62 cases in Japanese journals and 11 cases in Korean journals [1-3]. They are classified as either congenital or acquired. Acquired forms are further grouped as primary or sencondary types. The secondary lumbar hernias are attributed to previous surgery, trauma or infection. Primary or spontaneous lumbar hernias are usually in two anatomical locations: in the inferior (Petit triangle) or in the superior (Grynfeltt or Grynfeltt-Lesshaft triangle). Inferior triangle is smaller and bordered by the iliac crest at the base, the external oblique muscle laterally and the latissimus dorsi medially. Superior triangle is larger and more common location for a lumbar hernia and its borders are defined superiorly by the 12th rib, medially by erector spinae, laterally by the internal oblique muscle. Predisposing factors for primary acquired lumbar hernia are age, obesity, intense slimming, strenuous physical activity, and situations related to increased intra-abdominal pressure. The most common clinical sign is a bulge that increases with coughing or strenuous activity which tends to disappear when placed in the lateral decubitus position. In about 9% of cases the patients present with incarceration. Although the history, symptoms and physical signs suggest a lumbar hernia, an abdominal CT scan is essential for diagnosis. CT scan is used to confirm the physical examination, evaluate abdominal wall muscles, identify the hernia contents, and assess the anatomical relation of lumbar area [4].
There are many options in management of a lumbar hernia including no repair, suture closure, muscle closure of diverse techniques, and various repair with prostheses. Repairing the hernias is often difficult. The reasons for no standard treatment and difficulty in repair include difficulty in defining edges of the fascial defect, no adequate fascia and inherent weakness of the surrounding tissue, the bony boundaries, and the lack of collective experience of any one surgeon or group of surgeons to improve the operative technique [5].
Several surgeons have adapted the technique of laparoscopic ventral herniorrhaphy to lumbar hernia repair. In 1996, Burick and Parascandola [6] reported the first laparoscopic repair for a traumatic superior lumbar hernia. They explored the abdomen transperitoneally and repaired the lumbar defect with polypropylene mesh by a technique similar to that of transabdominal preperitoneal inguinal herniorrhaphy. In 1997, Heniford et al. [7] reported laparoscopic transperitoneal repair using a 4 cm overlapping polytetrafluoroethylene mesh secured with transabdominal polypropylene sutures. In 1999 Woodward et al. [8] operated on a patient of recurrent lumbar hernia having a history of previous open mesh repair by the first laparoscopic retroperitoneal (extraperitoneal) approach. With extraperitoneal approach, Habib [9] in 2000 repaired a primary Grynfeltt hernia, and in 2001 Meinke [10] did a large inferior lumbar hernia by transfascial suture and Tacker fixation of 4 cm overlapping polypropylene mesh. A flank incision permits easy dissection of extraperitoneal plane. With the aid of ballooning we can get generous operating space large enough to complete a repair with a large mesh which is secured to the abdominal wall with a transfascial suture and Tacker reinforcements. Although there are favorable reports of extraperitoneal mesh repair using Prolene Hernia System (Ethicon Inc., Somerville, NJ, USA) via the anterior approach in Japan and Korea [2,3] the laparoscopic extraperitoneal approach could be an ideal option for lumbar hernia repair.
Laparoscopic approaches for lumbar hernia using TEP technique of inguinal herniorrhaphy and laparoscopic ventral herniorrhaphy had been reported with promising results. Our experience of the laparoendoscopic TEP lumbar hernia repair further supports the advantages of excellent operative visualization as well as minimal invasiveness.
Figures and Tables
References
1. Moreno-Egea A, Baena EG, Calle MC, Martínez JA, Albasini JL. Controversies in the current management of lumbar hernias. Arch Surg. 2007. 142:82–88.
2. Kurumiya Y, Kameoka N, Ogawa A, Hibino M, Chigira H. A case of superior lumbar hernia- with review of 62 cases of lumbar hernia in Japan. Geka (Japanese). 2005. 67:1761–1765.
3. Chung M. Post-traumatic lumbar hernia repaired with PHS (Prolene Hernia System). J Korean Surg Soc. 2009. 77:221–224.
4. Salameh JR. Primary and unusual abdominal wall hernias. Surg Clin North Am. 2008. 88:45–60. viii
5. Yavuz N, Ersoy YE, Demirkesen O, Tortum OB, Erguney S. Laparoscopic incisional lumbar hernia repair. Hernia. 2009. 13:281–286.
6. Burick AJ, Parascandola SA. Laparoscopic repair of a traumatic lumbar hernia: a case report. J Laparoendosc Surg. 1996. 6:259–262.
7. Heniford BT, Iannitti DA, Gagner M. Laparoscopic inferior and superior lumbar hernia repair. Arch Surg. 1997. 132:1141–1144.
8. Woodward AM, Flint LM, Ferrara JJ. Laparoscopic retroperitoneal repair of recurrent postoperative lumbar hernia. J Laparoendosc Adv Surg Tech A. 1999. 9:181–186.
9. Habib E. Retroperitoneoscopic tension-free repair of lumbar hernia. Hernia. 2003. 7:150–152.
10. Meinke AK. Totally extraperitoneal laparoendoscopic repair of lumbar hernia. Surg Endosc. 2003. 17:734–737.




 ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download