Abstract
Purpose
Whereas the Kasai portoenterostomy (KPE) is an accepted first line of surgery for bile drainage in infants with biliary atresia, its long-term effectiveness is not clear because its etiology and pathogenesis remains unknown. This study was aimed to investigate the late complications occurring in long-term survivors and the current status of living patients who survived over 10 years after KPE.
Methods
A retrospective analysis of the medical records of 32 patients who underwent KPE from 1990 to 2000 was done. We analyzed 10-year survival rates with the Kaplan-Meier method and the current status of the long-term survivors.
Results
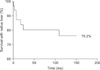
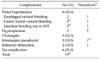
The overall 10-year survival rate by Kaplan-Meier method after KPE was 76.2%. Eight (25%) patients had died, including 4 who were transplanted. Nineteen (59.4%) patients survived over 10 years. Among them, 6 (31.6%) patients had portal hypertension, and 5 (26.3%) had episodes of cholangitis. Two had intrahepatic cyst and 2 had intestinal obstruction. Six (31.6%) patients have been well without any complications.
Conclusion
The long-term survival rate of biliary atresia is slightly improving. However, two thirds of patients suffer from various complications. One-third of survivors go on without any complication. As biliary atresia is known as a progressive inflammatory disease, careful life-long follow- up is needed in long-term survivals after KPE.
Since the success of Kasai portoenterostomies (KPE) in patients with biliary atresia, operative results have improved remarkably, and long-term survivals following the procedure have gradually increased. Despite evidence of a restoration in bile flow, however, liver cirrhosis and portal hypertension have remained as significant life threatening problems throughout patients' life times [1,2]. Herein, we analyzed long-term survival rates and current status of the living patients who underwent KPE over 10 years prior.
We analyzed medical records of the 32 patients with KPE performed for biliary atresia at our institution between 1990 and 2000, retrospectively. Telephone interviews were made when the authors needed further information lacking in the medical records. We analyzed 10-year survival rate by Kaplan-Meier method. Numbers of the death, causes, and the current status of survivals over 10 years were also evaluated. Transplanted cases were considered as death in our study.
During the period from 1990 to 2000, 32 infants with biliary atresia underwent KPE at our institution. Kaplan-Meier analysis showed the 10-year overall survival rate after KPE was 76.2% (Fig. 1). Of the 32 patients, 4 died due to hepatic failure, unknown origin of sepsis and unknown cause, 4 were transplanted, and 6 were lost during follow- up with a median (not average) follow-up period of 38.1 months (range, 2.7 to 88.1 months). Of 6 patients lost to follow up, 1 had severe hepatic dysfunction while 2 had almost normal liver status at the last follow-up check. Two patients suffered from cholangitis, and 1 had hypersplenism. Nineteen (59.4%) patients, including one case of transplant at the age of 17, survived over 10 years.
Among 19 patients who survived over 10 years after KPE, 6 (31.6%) patients suffered from portal hypertension; 2 with hypersplenism, and 4 with variceal bleeding. The 2 patients with hypersplenism were managed by partial splenic artery embolization (PSE). Among the 4 patients with variceal bleeding, 2 had esophageal variceal bleeding and were treated with endoscopic ligation of varices, 1 had gastric fundal variceal bleeding that was controlled by-balloon-occluded retrograde transvenous obliteration (BRTO), and 1 had intestinal bleeding due to arteriovenous malformation at jejunal branch from superior mesenteric artery and was controlled via embolization. There were 5 (26.3%) patients who suffered from cholangitis. Among those 5 patients, only 1 patient had a single episode and the remaining 4 patients had recurrent events of cholangitis. There were 2 patients with intrahepatic cyst. One was detected at 4 years after KPE, and maintained the same size with normal bilirubin level in 9 years of follow- up. The other patient had intrahepatic cystojejunostomy performed after failure of percutaneous transhepatic cholangio-drainage. Two patients had intestinal obstruction. Adhesive bandlysis was performed by laparotomy in one case and the other was managed conservatively.
Six (31.6%) patients have been well without any complications. The mean level of total bilirubin was 0.6 ± 0.3 mg/dL (range, 0.4 to 1.2 mg/dL) and no one had a history of admission or other illness except one who showed mild esophageal varix on esophagography without any event of bleeding or hypersplenism (Two patients had both cholangitis and variceal bleeding).
There were 8 patients who survived over 15 years. One patient was transplanted at the age of 17. Four patients suffered from portal hypertension. Three patients had histories of cholangitis. Three patients attended college and have lived without any problem. Their liver profiles were within the normal range (Table 2).
Although there has been an increase in the number of long-term survivors of biliary atresia, the disease is still one of the most challenging problems in the field of pediatric surgery because of progressive fibrosis, portal hypertension, and liver cirrhosis [3]. Several investigators have reported that KPE plays a role in gaining time for liver transplantation but is not a curative treatment [3,4]. However, the results of KPE seem to steadily improve, especially in Japanese studies. Altman et al. [5] reported 45% of 5-year survival rates with native liver and 35% for 10-year survival rate in 266 patients in 1997. Davenport et al. [6] showed their experience of 338 infants with biliary atresia, as their current survival rate of 5-years with native liver was 60% and 10-years survival was 41%. In 2003, Nio et al. [7] published 59.7% and 52.8% for 5- and 10-year survival rate, respectively, from the Japanese Biliary Atresia Registry. Furthermore, Shinkai et al. [1] showed improvement of post-KPE survival rate with almost 90% for 5years and nearly 80% for 10 years in patients who were operated on in the 1980s. We also reported increased 5-year survival rate in previous reports [8]. Our results showed 76.2% 10-year survival rates with native liver. As such, these increased post-KPE long-term survival rates suggest that KPE is still considered as first choice of surgery in patients with biliary atresia in the era of liver transplantation.
However, despite initially good surgical outcome of KPE, a few long-term survivals had portal hypertension, esophageal or gastric fundal varices due to hypersplenism, cholangitis, and hepatic failure caused by progressive ongoing cirrhosis and finally were in need of liver transplantation. Portal hypertension is considered the main cause of comorbidity among long-term survivals of biliary atresia. It could be presented as various types of variceal bleeding or hypersplenism. According to two series of long-term follow-up studies in Japan and France, which analyzed native liver after KPE over 20 years, incidence of portal hypertension were 49% and 70%, respectively [1,9]. In our study, one-third of survivals over 10 years had portal hypertensive events, which shows a similar incidence to previous reports [1,9]. Because biliary atresia is not restricted to the extrahepatic bile duct, patients who had KPE successfully performed display abnormalities of the intrahepatic biliary tree, including stenosis, dilatation, and sometimes pseudocyst formation. Intrahepatic change could lead to hepatic cirrhosis and affect portal hypertension [9]. Management of various variceal bleeding has developed according to the site and types of bleeding. In our cases, one esophageal variceal bleeding was controlled with endoscopic band ligation, which is considered as first line of treatment in variceal bleeding with sclerotherapy [9,10]. Another case of gastric fundal variceal bleeding was controlled with BRTO as previously reported [11]. Percutaneous embolization of a branch of jejunal artery was performed in one case of jejuna arteriovenous malformation who had suffered a chronic episode of melena. Another portal hypertensive complication of hypersplenism could be managed with PSE without splenectomy. Nio et al. [12] suggested that PSE should be used rather than splenectomy because it prevents not only the risk of post-splenectomy overwhelming sepsis but also severe intraabdominal adhesion, which could make dissection difficult during liver transplantation. Furthermore, they concluded the long-term efficacy of PSE was 70%. Both patients in our study who suffered hypersplenism were treated successfully with PSE.
With respect to cholangitis, Hadzic et al. [2] reported 41% of patients had cholangitis in 28 long-term survivors over 10 years, and Nio et al. [13] reported 48% in 21 long-term survivors over 20 years. Our series showed 26.3% in 19 survivors over 10 years, all of whom were managed with intravenous antibiotics.
Some authors reported that intrahepatic biliary cyst occurred in 23 to 25% of patients after KPE, and it has been considered that patients with intrahepatic cyst have poor outcomes compared to those who do not [14,15]. In our study, there were 2 patients with intrahepatic cyst. One survived more than 9 years without any procedure or management with constant size. The other case was performed intrahepatic cystojejunostomy as percutaneous transhepatic cholangio-drainage had failed. We have previously reported this case [16], and this patient finally received liver transplantation due to progressive hepatopulmonary syndrome.
The long-term survival rate after KPE in biliary atresia is slightly improving. However, two thirds of patients who survived over 10 years suffer from various complications including portal hypertension, cholangitis, intrahepatic cyst, and intestinal obstruction in spite of successful KPE. One-third of long-term survivals remain alive without any problem. Careful follow-up is needed because of some manifestations of ongoing liver cirrhosis and thus need planning for liver transplantation.
Figures and Tables
ACKNOWLEDGEMENTS
Presented at the 62nd Annual Congress of The Korean Surgical Society, Seoul, Korea, November 19, 2010.
References
1. Shinkai M, Ohhama Y, Take H, Kitagawa N, Kudo H, Mochizuki K, et al. Long-term outcome of children with biliary atresia who were not transplanted after the Kasai operation: >20-year experience at a children's hospital. J Pediatr Gastroenterol Nutr. 2009. 48:443–450.
2. Hadzić N, Davenport M, Tizzard S, Singer J, Howard ER, Mieli-Vergani G. Long-term survival following Kasai portoenterostomy: is chronic liver disease inevitable? J Pediatr Gastroenterol Nutr. 2003. 37:430–433.
3. Hartley JL, Davenport M, Kelly DA. Biliary atresia. Lancet. 2009. 374:1704–1713.
4. Leonhardt J, Kuebler JF, Leute PJ, Turowski C, Becker T, Pfister ED, et al. Biliary atresia: lessons learned from the voluntary German registry. Eur J Pediatr Surg. 2011. 21:82–87.
5. Altman RP, Lilly JR, Greenfeld J, Weinberg A, van Leeuwen K, Flanigan L. A multivariable risk factor analysis of the portoenterostomy (Kasai) procedure for biliary atresia: twenty-five years of experience from two centers. Ann Surg. 1997. 226:348–353.
6. Davenport M, Kerkar N, Mieli-Vergani G, Mowat AP, Howard ER. Biliary atresia: the King's College Hospital experience (1974-1995). J Pediatr Surg. 1997. 32:479–485.
7. Nio M, Ohi R, Miyano T, Saeki M, Shiraki K, Tanaka K. Five- and 10-year survival rates after surgery for biliary atresia: a report from the Japanese Biliary Atresia Registry. J Pediatr Surg. 2003. 38:997–1000.
8. Hong AR, Jung E, Kang YN, Choi SO, Park WH. Five-year survival and prognostic factors after Kasai portoenterostomy for biliary atresia. J Korean Surg Soc. 2010. 79:405–410.
9. Lykavieris P, Chardot C, Sokhn M, Gauthier F, Valayer J, Bernard O. Outcome in adulthood of biliary atresia: a study of 63 patients who survived for over 20 years with their native liver. Hepatology. 2005. 41:366–371.
10. Miga D, Sokol RJ, Mackenzie T, Narkewicz MR, Smith D, Karrer FM. Survival after first esophageal variceal hemorrhage in patients with biliary atresia. J Pediatr. 2001. 139:291–296.
11. Hwang JB, Jung EY, Park WH, Kim YH, Kim AS. Balloon-occluded retrograde transvenous obliteration treats hepatic dysfunction and gastric varices. J Pediatr Gastroenterol Nutr. 2011. 52:219–221.
12. Nio M, Hayashi Y, Sano N, Ishii T, Sasaki H, Ohi R. Longterm efficacy of partial splenic embolization in children. J Pediatr Surg. 2003. 38:1760–1762.
13. Nio M, Ohi R, Hayashi Y, Endo N, Ibrahim M, Iwami D. Current status of 21 patients who have survived more than 20 years since undergoing surgery for biliary atresia. J Pediatr Surg. 1996. 31:381–384.
14. Shimadera S, Iwai N, Deguchi E, Kimura O, Ono S, Furukawa T, et al. Predicting factors on the occurrence of cystic dilatation of intrahepatic biliary system in biliary atresia. Pediatr Surg Int. 2010. 26:611–614.
15. Takahashi A, Tsuchida Y, Suzuki N, Kuroiwa M, Murai H, Toki F, et al. Intrahepatic biliary cysts in biliary atresia in the era of liver transplantation. J Pediatr Gastroenterol Nutr. 2003. 36:608–612.
16. Park WH, Choi SO. The intrahepatic biliary cyst in biliary atresia after Kasai operation. J Korean Assoc Pediatr Surg. 1999. 5:126–129.




 ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download