Abstract
Hemorrhage in the gallbladder (GB) is usually associated with cholecystitis, GB neoplasm, trauma, hemobilia, and cystic artery aneurysm. Our patient had not experienced any previous abdominal trauma, and GB hemorrhage was unlikely to result from cholecystitis or bleeding diathesis. A 55-year-old male was admitted because of right upper quadrant pain. Both prothrombin time and partial thromboplastin time were normal. Abdominal computed tomography, endoscopic ultrasound and magnetic resonance cholangiopancreatography were performed. Image studies revealed GB wall thickening and an intraluminal mass. Laparoscopic cholecystectomy was performed. Upon opening the GB postoperatively, a large amount of fresh blood and old blood clot was noted. The incidence of GB hematoma is very rare. GB hematoma should always be considered in the differential diagnosis of GB tumor. In such a situation, surgical intervention is needed for further patient evaluation and management. We present a rare case of intramural GB hematoma, of which we were unable to make a definitive diagnosis preoperatively.
Intramural gallbladder hematoma is one of the rare causes of abdominal pain and commonly occurs in patients with trauma, hemobilia, gallbladder neoplasm, or bleeding diathesis including renal impairment, hepatic cirrhosis, and anticoagulant therapy [1]. The clinical characteristics vary from findings indicating cholecystitis such as right upper quadrant (RUQ) pain, fever, and leukocytosis to symptoms indicating gastrointestinal bleeding like hemobilia, melena, and hematemesis [2,3]. While abdominal ultrasonography is a major imaging method to diagnose gallbladder diseases, it is difficult to distinguish hyperechogenic, immovable mass on the ultrasonography from diseases like gallbladder neoplasm, tumefactive biliary sludge, and gangrenous cholecystitis [4]. We present one case of intramural gallbladder hematoma of which we were unable to make a definitive diagnosis until after cholecystectomy in a patient who had not experienced any previous abdominal trauma and had no history of bleeding disorders.
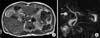
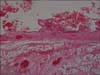
A 55-year-old man visited us with a major complaint of RUQ pain. The pain was sudden in onset, dull in character, and did not radiate to the back. It was not aggravated by food intake or related to movement. On admission, the physical examination exhibited RUQ tenderness and a positive Murphy's sign. Laboratory examinations revealed that white blood cell, hemoglobin, hematocrit, and platelet counts were 9,450/mm3, 16.4 gm/dL, 46.5%, and 289,000/mm3, respectively, which were all within the normal limits. The international normalized ratios including prothrombin time and activated partial thromboplastin time were all normal. Serum amylase and lipase were 47 U/L and 22 U/L, respectively, which were all within the normal limits. Aspartate aminotransferase/alanine aminotransferase was 171/57 U/L and total bilirubin 1.6 mg/dL, which showed slight increase. However, alkaline phosphatase was 48 U/L, which was within the normal limits. As chronic cholecystitis was suspected, abdominal computed tomography (CT) was performed. On the abdominal CT, thickening of the gallbladder wall and high-density intramural gallbladder mass without contrast enhancement were suspected (Fig. 1). Therefore, endoscopic ultrasound (EUS) and magnetic resonance cholangiopancreatography (MRCP) were conducted. The EUS revealed mild diffuse thickening of the gallbladder wall and mass in the gallbladder lumen with the hypoechogenic boundary surrounded by a single layer of membrane along with messy hyperechoic signals (Fig. 2). The MRCP showed mild non-specific diffuse biliary dilatation but did not find anything to suspect biliary obstruction. As with the previous tests, the MRCP showed diffuse thickening of the gallbladder wall and a filling defect inside the gallbladder (Fig. 3). The patient complained of mild but persistent RUQ pain, and a possibility of gallbladder tumor could not be ruled out considering the findings of several imagining studies. Therefore, laparoscopic cholecystectomy was performed. The gallbladder was somewhat distended. There was neither adhesion to the liver nor distinct inflammatory change. Bloody fluid was not seen in the peritoneal cavity. Upon opening the gallbladder postoperatively, a large amount of fresh blood and old blood clot was noted. Macroscopically, the gallbladder mucosa was covered with hematoma. After removal of hematoma, some mucosal congestion was observed (Fig. 4). Under optical microscope, diffuse hemorrhage and infiltration of non-specific chronic inflammatory cells were observed from the mucosa to serosa (Fig. 5). The patient was discharged without any specific complications on the third day after surgery.
Intramural gallbladder hematoma is a very rare disease and its causes are various. Since Sandblom [5] reported 9 patients with cholemia who showed post-traumatic acute abdominal pain and shock in 1948, intramural gallbladder hematoma has been reported in a number of clinical situations.
Intramural gallbladder hematoma commonly occurs after trauma including percutaneous liver biopsy [6]. It is also associated with gallbladder neoplasm, aneurysm rupture, hemophilia, bleeding diathesis including renal impairment and hepatic cirrhosis, and anticoagulant therapy. Hemorrhage accompanied with cholecystitis has rarely been reported [6]. As for symptoms, clinical characteristics indicating acute cholecystitis such as RUQ pain, fever, and leukocytosis are commonly observed, and gastrointestinal bleeding like hemobilia, melena, and hematemesis rarely happen. Intramural gallbladder hematoma caused by hemorrhage can rarely induce obstruction of common bile duct, leading to cholangitis. Therefore, intramural gallbladder hematoma can be hard to diagnose by symptoms alone. Scrupulous examinations should be conducted including ultrasonography, abdominal CT, and - if gastrointestinal bleeding is suspected - endoscopy. Despite several concomitant imaging studies, it can be difficult to diagnose gallbladder hematoma, which occurs without initiating factors including clear trauma and coagulopathy, because it looks similar to gallbladder tumor, tumefactive biliary sludge, etc.
Ultrasonography is an important method in diagnosing gallbladder diseases. On the ultrasonography, gallbladder hematoma shows fluidity changes caused by changes in posture along with hyperechogenic mass in the gallbladder. The diseases that can be identified by ultrasonography, which reveals intramural gallbladder mass, include gallbladder cancer, tumefactive biliary sludge, and gangrenous cholecystitis. Early findings of gallbladder tumors on ultrasonography are local gallbladder wall thickening, irregular-bordered polyp-shaped lesion, loss of normal gentle contour of the gallbladder, etc. In the case of tumefactive biliary sludge, diffuse rough shadow in the gallbladder is observed along with thickening gallbladder wall, but acoustic shadow is not. Therefore, they must be distinguished from intra-gallbladder hematoma [7].
In this case report, the patient visited us for RUQ pain and there were no findings to suspect cholecystitis except for high-density shadow in the gallbladder on the abdominal CT. The subsequent EUS revealed immovable polypoidmass in the gallbladder lumen with clear boundary as well as diffuse thickening of the gallbladder wall. These findings allowed us to strongly suspect gallbladder tumor in a situation when obvious evidence could not be found to predict occurrence of intramural gallbladder hematoma. The MRCP showed mild non-specific diffuse biliary dilatation, thickening of the gallbladder wall, and filling defect in the gallbladder. These findings were also similar to those indicative of gallbladder tumor.
Treatment of intramural gallbladder hematoma can be managed by conservative therapy or surgical intervention depending on its cause. For gallbladder hematoma caused by trauma or bleeding diathesis, substantial improvement can be expected mainly through conservative therapy and follow up as long as the patient's vital signs are stable, the clinical course is good or there are no findings such as persistent bleeding. However, if gangrenous cholecystitis is accompanying, emergency cholecystectomy should be performed because complications including perforation may occur [8]. If gallbladder tumor is suspected as with this case report, surgical treatment is required. As mentioned above, intramural gallbladder hematoma is a very rare disease and most cases can not be definitely diagnosed although findings of imaging studies are different from those indicative of gallbladder tumor. Therefore, the possibility of gallbladder tumor should be taken into consideration when a diagnosis is made. It is very difficult to diagnose intramural gallbladder hematoma before surgery. It is almost impossible to diagnose, especially when the patient does not have trauma or hemophilia or is not onanticoagulant therapy [9,10].
Therefore, when gallbladder tumor cannot be definitely distinguished and diagnosed by applicable test methods and it is difficult to predict the clinical course as with this case report, a definite diagnosis should be made by cholecystectomy. In this case, we could not predict gallbladder bleeding because it is very rare in healthy men without any special medical history including hemorrhagic diseases. Under the impression of probable gallbladder tumor, we opened the gallbladder, removed the hematoma, and performed tissue scanning to follow up for mucosa after cholecystectomy. However, macroscopic gallbladder tissues in the pool of blood and hematoma could not be scanned. In conclusion, when hyperechogenic lesion is seen in the gallbladder, gallbladder cancer should be suspected mostly, but hematoma, which can occur without bleeding diathesis or trauma, should be considered in the differential diagnosis, and cholecystectomy should be performed for definite diagnosis.
Figures and Tables
Fig. 2
Endoscopic ultrasonography shows diffuse wall thickening of the gallbladder with a fixed echogenic polypoid mass (arrow) in the gallbladder lumen.
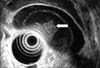
Fig. 3
MRCP shows (A) heterogenous multiple filling defects in gallbladder with diffuse gallbladder wall thickening (arrow) and (B) mild diffuse biliary tree dilatation without demonstrable obstructive lesion.
References
1. Tan SW, Lai SK, Ng KW, Chen P, Chen KH, Jiang CF. Intramural gallbladder hematoma mimicking gallbladder neoplasm in a 33-year-old male. J Chin Med Assoc. 2005. 68:146–149.
2. Lai YC, Tarng DC. Hemorrhagic acalculous cholecystitis: an unusual location of uremic bleeding. J Chin Med Assoc. 2009. 72:484–487.
3. Parekh J, Corvera CU. Hemorrhagic cholecystitis. Arch Surg. 2010. 145:202–204.
4. Gore RM, Yaghmai V, Newmark GM, Berlin JW, Miller FH. Imaging benign and malignant disease of the gallbladder. Radiol Clin North Am. 2002. 40:1307–1323. vi
5. Sandblom P. Hemorrhage into the biliary tract following trauma; traumatic hemobilia. Surgery. 1948. 24:571–586.
6. Kwon TK, Jeon SH, Park HW, Jung WJ, Hwang JY, Park KS, et al. A case of intraluminal gallbladder hematoma after percutaneous liver biopsy. Korean J Hepatol. 2002. 8:486–489.
7. Wibbenmeyer LA, Sharafuddin MJ, Wolverson MK, Heiberg EV, Wade TP, Shields JB. Sonographic diagnosis of unsuspected gallbladder cancer: imaging findings in comparison with benign gallbladder conditions. AJR Am J Roentgenol. 1995. 165:1169–1174.
8. Gremmels JM, Kruskal JB, Parangi S, Kane RA. Hemorrhagic cholecystitis simulating gallbladder carcinoma. J Ultrasound Med. 2004. 23:993–995.
9. Shimura T, Kojima T, Tsutsumi S, Yoshida T, Uchiumi H, Kuwano H. Gallbladder hematoma in a patient with hemophilia B, report of a case. Hepatogastroenterology. 2000. 47:939–941.
10. Cho YU, Kim JY, Choi SK, Hur YS, Lee KY, Kim SJ, et al. A case of hemorrhagic gallbladder paraganglioma causing acute cholecystitis. Yonsei Med J. 2001. 42:352–356.




 ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download