Abstract
Purpose
To describe the clinical characteristics and outcomes after inguinal hernia repair in overweight and obese patients.
Methods
We retrospectively reviewed the medical records of 636 adult patients who underwent mesh plug inguinal hernia repair performed by one surgeon from November 2001 to January 2009.The clinical characteristics and surgical outcomes of the patients were analyzed. According to the body mass index, patients higher than 23 were defined as overweight and obese patient group (O group) and patients between 18.5 and 23 were defined as normal weight patient group (N group). Seventeen underweight patients were excluded in this study.
Results
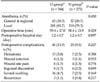
Of 619 cases, the number for O group was 344 (55.6%) and for N group was 275 (44.4%). The mean age was significantly higher in N group (62.2 ± 12.6 vs. 64.4 ± 14.8, P = 0.048). Underlying diseases were present in 226 (65.7%) of the O group and 191 (69.5%) of the N group (P = 0.322). Anesthesia method, operative time and postoperative hospital stay had no significant difference between the two groups. Postoperative complications developed in 41 (11.9%) of the O group and in 28 (10.2%) of the N group, respectively, and no major complications developed in either group.
Conclusion
Adult inguinal hernias developed at a relatively younger age in overweight and obese patients than in normal weight patients. There were no specific differences in other clinical characteristics and outcomes between the two groups. Therefore inguinal hernia repair in overweight and obese patients is a safe procedure as in normal weight patients.
The cumulative incidence of inguinal hernia is 13.9% in the male and 2.1% in the female [1]. Inguinal hernia repair is one of most commonly performed surgeries in the world, and approximately 100,000 cases have been performed annually in England, and approximately 750,000 cases in the USA [2]. Obesity increases the development of underlying diseases such as coronary artery diseases and hypertension, hence, it has been considered to be a risk factor of poor outcomes after surgery [3]. Nonetheless, it is controversial. Reid et al. [4] reported that the incidence of complications in overweight and obese patients was not different from normal weight patients. Studies concerning the effect of obesity on the outcomes after inguinal hernia repair have been reported rarely. The aim of this study is to describe the clinical characteristics and outcomes after inguinal hernia repair in overweight and obese patients by comparing with those of normal weight patients.
We retrospectively reviewed the medical records of 636 patients who were older than 20 years and underwent mesh plug inguinal hernia repair performed by one surgeon at our hospital from November 2001 to January 2009 and the clinical characteristics and surgical outcomes of patients were analyzed. Based on the Asia-Pacific obesity classification, patients were classified as underweight (body mass index [BMI] < 18.5), normal (18.5 ≤ BMI < 23), overweight (23 ≤ BMI < 25), obese (BMI ≥ 25), and severely obese (BMI ≥ 30) by BMI.
According to the BMI, patients higher than 23 were defined as the overweight and obese patient group (O group), patients between 18.5 and 23 were defined as the normal weight patient group (N group). Seventeen underweight patients were excluded in this study.
Statistical analysis was performed with SPSS ver. 12.0 (SPSS Inc., Chicago, IL, USA). Chi square test and Student's t-test were performed, and P < 0.05 was considered to be statistically significant.
Of 619 cases, overweight were 168 (27.1%), obese were 176 (28.4%), total of overweight and obese patient group (O group) was 344 (55.6%) and the N group was 275 (44.4%).
The mean age was 62.2 ± 12.6 years in the O group and 64.4 ± 14.8 years in the N group, significantly higher in the N group (P = 0.048). The rate of patients aged 65 or more was 47.1% in the O group, 60.0% in the N group, significantly higher in the N group (P = 0.001).
The rate of the male in the O group was 94.2% and that of the N group was 91.6%. In regard to BMI, the O group was 25.4 ± 1.9, the highest case was 33.9 and the N group was 21.2 ± 1.1. On the other hand, in patients less than 65 years, BMI was 24.0 ± 2.7 and in patients aged 65 years or more, it was 23.2 ± 2.6 and it was significantly lower in elderly patients (P < 0.001).
Concerning the location of hernia, in the O group, the right side was 191 (55.5%), the left side was 142 (41.3%) and bilateral was 11 (3.2%), and in the N group, the right side was 140 (50.9%), the left side was 118 (42.9%), and bilateral was 17 (6.2%) (P = 0.156). The type of hernia in the order was indirect, direct, femoral and pantaloon type in both groups.
The mean symptomatic period of the O group was 2.8 ± 7.6 years and the N group was 2.3 ± 7.1 years respectively (P = 0.451).
Examining the distribution of patients according to their age group, in both the O group and the N group, patients were prevalent in the order of the 60s, 70s, and 50s. And the rate of the O group patients was in the order of the 50s (63.1%), 60s (60.1%) and 40s (58.3%).
Underlying diseases were present in 226 (65.7%) of the O group and 191 (69.5%) of the N group respectively (P = 0.322).
Concerning anesthesia methods, in the O group, general or spinal anesthesia were performed in 63 (18.3%) and local anesthesia was performed in 281 (81.7%). And in the N group, general or spinal anesthesia were performed in 57 (20.7%) and local anesthesia was performed in 218 (79.3%) respectively (P = 0.450).
The operative time of the O group was 59.4 ± 17.0 minutes and the N group was 58.4 ± 15.9 minutes (P = 0.429), and the postoperative hospital stay of the O group was 1.2 ± 0.7 days and the N group was 1.2 ± 0.7 days respectively (P = 0.897).
Postoperative complications were developed in 41 (11.9%) of the O group, hematoma 13 (3.8%), wound infection 4 (1.2%), wound site pain 6 (1.7%), inguinal discomfort 6 (1.7%), scrotal swelling 16 (4.7%) and recurrence 1 (0.3%), and in 28 (10.2%) of the N group, hematoma 7 (2.5%), wound infection 3 patients (1.1%), wound site pain 4 (1.5%), inguinal discomfort 6 (2.2%), scrotal swelling 7 (2.5%) and recurrence 3 (1.1%) (P = 0.495). Mean follow up period was 61.0 ± 22.6 months. No major complications were developed in both groups.
Of the O group, if we definite severe obese (BMI ≥ 30) by BMI as the severely group (S group) and compare with the N group, total of patient was 286. The S group was 11 (3.8%) and the N group was 275 (96.2%).
In regard to BMI, the S group was 31.7 ± 1.1, the highest case was 33.9 and the N group was 21.2 ± 1.1.
Underlying diseases were present in 7 (63.6%) of the S group and 191 (69.5%) of the N group respectively (P = 0.742).
The operative time of the S group was 66.5 ± 21.1 minutes and the N group was 58.4 ± 15.9 minutes (P = 0.103), and the postoperative hospital stay of the S group was 1.4 ± 0.5 days and the N group was 1.2 ± 0.7 days respectively (P = 0.554).
Postoperative complications were developed in 4 (36.4%) of the S group, wound infection 1 (9.1%), inguinal discomfort 1 (9.1%), scrotal swelling 16 (4.7%) and no recurrence and in 28 (10.2%) of the N group (P = 0.017).
In adults, inguinal hernia developed commonly in old and thin males [5,6]. In addition, it has been reported to occur readily in cases with hiatal hernia, varix, prostate hyperplasia, hemorrhoids, etc. [1,6]. Besides, in adult males, many risk factors inducing inguinal hernia have been reported. In cases with the family history of inguinal hernia, the probability of developing inguinal hernia is approximately 8 times higher. And repeated lifting heavy materials for a long period or activities requiring a big force suddenly, chronic cough, chronic obstructive pulmonary disease, education levels, drinking, monthly net income, etc. have been reported to be risk factors [7-10]. On the other hand, in adult females, risk factors are family history, constipation, old age, living in a rural area, tall, chronic cough, umbilical hernia, etc. [1,11].
Theoretically, obesity has been considered to increase the incidence of inguinal hernia by increasing abdominal pressure [5]. However, the risk of developing inguinal hernia was shown to be rather decreased in overweight and obese patients in most reports [1,5,6], Rosemar et al. [5] have reported that in 47 to 55 years adult male inguinal hernia patients, with the increase of 1 unit (3 to 4 kg) BMI, the risk level is decreased by 4%, and in comparison with normal weight patients, in obese patients, the risk rate of developing inguinal hernia is decreased to 43%. In addition, in adult females, obesity has been reported to be a defense factor of inguinal hernia [11].
On the other hand, diabetes or hypertension is not associated with inguinal hernia [5], and in adult females, smoking, multiparity, appendectomy and other abdominal surgeries are not associated with the development of inguinal hernia [11].
In adult inguinal hernia patients, the ratio of overweight and obese patients varies slightly depending on reports. In a study conducted on 125 patients older than 19 years reported by Reid et al. [4], the median value of BMI was 27 (19 to 38), 28% of cases were normal weight, and 72% of cases were overweight or obese patients. In our study, the mean value of BMI was 23.6 (18.5 to 33.9), 44.4% cases were normal weight, 27.1% cases were overweight, and 28.4% were obese patients, and the sum of overweight patients and obese patients was 55.6%.
In regard to the mean age of patients, in overweight and obese patients, it was 62.2 ± 12.6 years, and significantly lower than 64.4 ± 14.8 years of normal weight patients (P = 0.048). It is because as aging, generally, patient's weight decrease, and thus the BMI of patients younger than 65 years was 24.0 ± 2.7, that of patients aged 65 years or older was 23.2 ± 2.6, and it was significantly lower in elderly patients (P < 0.001). Underlying diseases were 65.7% in the O group and 69.5% in the N group respectively, and it had no statistically significant difference (P = 0.343).
Because of several advantages of inguinal hernia repair performed under local anesthesia, the satisfaction of patients have been obtained, nonetheless, in overweight and obese patients, attentions should be paid on the maximal safety dose of local anesthetic agents. Reid et al. [4] used average 62 mL of local anesthetic agent (mixture of lignocaine, bupibacaine, adrenaline and saline) in overweight and obese patients, and 58 mL in normal weight patients, and special complications caused by local anesthetic agents were not developed. In their study, the rate of one day surgery in overweight and obese patients was 84%, in normal weight patients was 91%. In our hospital, principle is to discharge on 1st postoperative day after inguinal hernia repair, and the rate of patients discharged on the 1st postoperative day was 85.2% in overweight and obese patients, 81.8% in normal weight patients, and there was no significant difference.
In a study performed on 125 patients older than 19 years reported by Reid et al. [4], concerning complications, in normal weight patients, hematoma was 2 (6%) and wound infection was 1 (3%), and in overweight and obese patients, hematoma was 1 (1%) and wound infection was 2 (2%), and no significant difference between the two groups was seen. Therefore, they reported that overweight and obese patients underwent inguinal hernia repair using local anesthesia well, and it was a safe procedure. In our study, in almost all patients except patients with the fear of local anesthesia, hernia repair was performed under local anesthesia in 79.3% of normal weight patients and 81.7% of overweight and obese patients.
Lindström et al. [12] have reported that among patients underwent inguinal hernia repair, in cases with high BMI, the risk of the development of complications was increased, and the higher was BMI, the longer was the average postoperative hospital stay. In our study, the incidence of complications in overweight and obese patients was 11.9%, normal weight patients was 10.2%, and a significant difference was not shown, and the mean postoperative hospital stay was 1.3 ± 0.9 days in overweight and obese patients and 1.5 ± 3.9 days in normal weight patients, respectively, and a difference was not shown. It has been shown that obesity is an independent risk factor of wound infection, and deep vein thrombosis or pulmonary embolism is developed more frequently in obese patients in comparison with normal patients [3]. In abdominal wall surgery, infection of prosthetic material is rare, nonetheless, it is a very important complication developed in 1.3%, and obesity has been reported to be included in a risk factor of the infection of mesh [13]. In addition, in inguinal hernia repair without using a mesh, obesity is associated with wound infection [14]. In a study conducted on patients underwent surgery in the department of general surgery, urology, vascular surgery, chest surgery and gynecology reported by Choban et al. [15], BMI was normal in 63%, obese in 21%, and morbid obese in 16%. In each group, opportunistic infection developed in 0.05%, 2.8%, and 4.0%, respectively, and there was significant difference, and thus they reported that obesity is to be a risk factor of opportunistic infection in patients undergoing surgery. In our study, wound infection developed 4 patients (1.2%) in overweight and obese patients, and 3 patients (1.1%) in normal weight patients, and there was no significant difference.
In Korea, BMI ≥ 35 patients are very rare and BMI ≥ 40 patients are extremely rare. In this study, there were no BMI ≥ 35 patients. So we compared severely obese patient group and normal weight patient group. In this study, operative time was about 8 minutes longer in severely obese patient group but not statistically significant (P = 0.103). Postoperative complications were developed more in severely obese patient group (36.4%) than normal weight patient group (10.2%) (P = 0.017).
In conclusion, in adult inguinal hernia, it is developed at relatively younger ages in overweight and obese patients in comparison with normal weight patients, and the rate of elderly patients aged 60 or more is 47.1% in overweight and obese patients, and it is less than 60.0% of normal weight patients. In addition, the rate of overweight and obese patients in the 50s and the 60s was more than 60%. In regard to underlying diseases, the ratio of surgery performed under local anesthesia, operation time, the postsurgical hospitalization period, postsurgical complications, etc., a significant difference between the two group was not shown, and thus it is considered that in overweight and obese patients, inguinal hernia repair is a safe procedure, as like in normal weight patients.
Figures and Tables
Table 1
Comparison of demographics between overweight and obese patient group and normal weight patient group

Table 2
Comparison of the age distribution between the overweight and obese inguinal hernia patients and normal weight inguinal hernia patients

ACKNOWLEDGEMENTS
This paper was presented at the 61th annual meeting of the Korean Surgical Society, November 11-13, 2009, COEX, Seoul, Korea.
References
1. Ruhl CE, Everhart JE. Risk factors for inguinal hernia among adults in the US population. Am J Epidemiol. 2007. 165:1154–1161.
2. Kingsnorth A. Treating inguinal hernias. BMJ. 2004. 328:59–60.
3. DeMaria EJ, Carmody BJ. Perioperative management of special populations: obesity. Surg Clin North Am. 2005. 85:1283–1289. xii
4. Reid TD, Sanjay P, Woodward A. Local anesthetic hernia repair in overweight and obese patients. World J Surg. 2009. 33:138–141.
5. Rosemar A, Angerås U, Rosengren A. Body mass index and groin hernia: a 34-year follow-up study in Swedish men. Ann Surg. 2008. 247:1064–1068.
6. Abramson JH, Gofin J, Hopp C, Makler A, Epstein LM. The epidemiology of inguinal hernia. A survey in western Jerusalem. J Epidemiol Community Health. 1978. 32:59–67.
7. Lau H, Fang C, Yuen WK, Patil NG. Risk factors for inguinal hernia in adult males: a case-control study. Surgery. 2007. 141:262–266.
8. Carbonell JF, Sanchez JL, Peris RT, Ivorra JC, Del Baño MJ, Sanchez CS, et al. Risk factors associated with inguinal hernias: a case control study. Eur J Surg. 1993. 159:481–486.
9. Flich J, Alfonso JL, Delgado F, Prado MJ, Cortina P. Inguinal hernia and certain risk factors. Eur J Epidemiol. 1992. 8:277–282.
10. Sanjay P, Woodward A. Single strenuous event: does it predispose to inguinal herniation? Hernia. 2007. 11:493–496.
11. Liem MS, van der Graaf Y, Zwart RC, Geurts I, van Vroonhoven TJ. The Coala Trial Group. Risk factors for inguinal hernia in women: a case-control study. Am J Epidemiol. 1997. 146:721–726.
12. Lindström D, Sadr Azodi O, Bellocco R, Wladis A, Linder S, Adami J. The effect of tobacco consumption and body mass index on complications and hospital stay after inguinal hernia surgery. Hernia. 2007. 11:117–123.
13. Bueno Lledó J, Sosa Quesada Y, Gomez I Gavara I, Vaqué Urbaneja J, Carbonell Tatay F, Bonafé Diana S, et al. Prosthetic infection after hernioplasty. Five years experience. Cir Esp. 2009. 85:158–164.
14. Pessaux P, Lermite E, Blezel E, Msika S, Hay JM, Flamant Y, et al. Predictive risk score for infection after inguinal hernia repair. Am J Surg. 2006. 192:165–171.
15. Choban PS, Heckler R, Burge JC, Flancbaum L. Increased incidence of nosocomial infections in obese surgical patients. Am Surg. 1995. 61:1001–1005.




 ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download