Abstract
Purpose
ABO incompatible (ABOi) kidney transplantation (KT) has been increasing to compensate for the shortage of organ donors. However, detailed comparative analyses of ABOi KT with ABO compatible (ABOc) KT are still rare.
Methods
This retrospective study compared 12 consecutive ABOi KTs to 50 ABOc KTs that employed the same maintenance immunosuppressive agents during the same period. Comparisons of patient survival, graft survival, graft function, and complications were made until post-transplant day 90.
Results
Baseline characteristics of the two groups were similar except for the positivity of panel reactive antibody (12% in the ABOc group vs. 42% in the ABOi group; P = 0.029). There were no significant differences in patient survival, graft survival, post-operative renal function, incidence of acute rejection, infections, or medical and surgical complications. However, bleeding complications were more common in the ABOi group (25%) than versus the ABOc group (6%) (P = 0.08). The preoperative and total hospital stay of the ABOi patients was significantly longer than the ABOc patients (P = 0.001).
The ideal treatment for end-stage renal disease (ESRD) is kidney transplantation (KT). However, the considerable shortage of donor organs and the increasing number of patients with ESRD on KT waiting lists often have resulted in unacceptably long waiting times for an appropriate organ allograft. Despite only a slight increase in the number of KTs performed in Korea in the past decade, the number of ESRD patients requiring renal replacement therapy has markedly increased from 23,900 in 1998 to 56,396 in 2009. At the end of 2008, there were more than 7,000 patients awaiting KT and the median wait time was 1,660 days [1,2].
The increasing demand for KT requires an expanded pool of potential kidney donors. One option is anti-blood group-incompatible (ABOi) living donors. ABO incompatibility had, until recently, been regarded as an absolute contraindication to living donor transplantation because of the high risk of hyperacute rejection [3]. Alexandre et al. [4,5] reported the first planned successful ABOi KT using plasmapheresis (PP) and splenectomy, although the overall short- and long-term rates of graft survival were poor. However, in the modern era of immunosuppression, the use of the protocol that includes PP plus rituximab has led to encouraging results [6-8]. Recently, ABOi KT was also started in Korea; the data is scanty [9].
To be generally used in a donor organ program, ABOi KT must not have a negative impact on graft survival, patient survival, graft function, and complications compared with ABOc KT. However, a little comparative data is available. To address this important shortfall, the present study compared 12 consecutive ABOi KTs to 50 ABOc KTs that employed the same maintenance immunosuppressive agents during the same period. Comparisons of patient survival, graft survival, graft function, and complications were made until post-transplant 90th day.
This comparative retrospective and cross-sectional study was approved by the Seoul St. Mary's Hospital Institutional Review Board.
From May 2009 to March 2010, 12 patients were prepared for ABOi living donor KTs and none were excluded due to magnitude of their ABO antibody (Ab) titer. As a control group, 50 ABOc living donor KTs performed during the same period were selected on the basis of the initial maintenance immunosuppressive therapy (tacrolimus, mycophenolate mofetil, and corticosteroids; see below). Another 10 ABOc living donor KTs that were done during the same period had been maintained on other immunosuppressive agents, and so were excluded.
All kidney recipients of both ABOc and ABOi grafts received basiliximab (20 mg on days 0 and 4; Simulect, Novatis Pharmaceuticals Co., Basel, Switzerland) as antibody induction. Maintenance immunosuppression consisted of tacrolimus (Tacrobell, Chong Kun Dang Pharmaceuticals Co., Seoul, Korea; Prograf, Astellas Pharma Inc., Toyama, Japan), corticosteroid, and either mycophenolate mofetil (Cellcept, Hoffmann-La Roche Inc., Nutley, NJ, USA) or mycophenolate sodium (Myfortic, Novatis Pharmaceuticals Co.).
In the ABOc group, tacrolimus and corticosteroid was started on pretransplant day 2. A trough level of tacrolimus was maintained at 8 to 12 ng/mL in the first month and 6 to 8 ng/mL thereafter. Methylprednisolone was administered at a dose of 125 mg/day, 250 mg/day, 500 mg/day, 240 mg/day, and 180 mg/day on pretransplant day 2, 1, operation day, posttransplant day 1 and 2, respectively. Prednisolone (30 mg/day) was prescribed beginning at posttransplant day 3 and was rapidly tapered to a dose of 10 mg/day by 1 month post-transplantation. Mycophenolate mofetil (1,500 mg/day twice daily or 1,000 mg/day twice daily if body weight <50 kg) or mycophenolate sodium (1,080 mg/day twice daily or 720 mg/day twice daily if body weight <50 kg) was begun on operation day. The recipients receiving ABOc allograft with positive complement dependent cytotoxicity test were additionally prepared with single dose of rituximab (375 mg/m2; Roche Pharma AG, Renach, Switzerland) and plasma exchange (PE) followed by 100 mg/kg of intravenous immunoglobulin (IVIG) 7 days before planned operation.
In the ABOi group, a single dose of rituximab (100 to 375 mg/m2) was administered 1 month before the anticipated transplantation. On seven days before the scheduled operation, a triple oral immunosuppression regimen consisting of tacrolimus, mycophenolate mofetil or mycophenolate sodium, and prednisolone (20 mg/day) were started. The target trough level of tacrolimus and the dosage of mycophenolate mofetil or mycophenolate sodium were same as used for the ABOc recipients. Twenty milligrams of prednisolone was changed to methylprednisolone on preoperative day 2. The dosage of methylprednisolone was 125 mg/day, 250 mg/day, 1,000 mg/day, 500 mg/day, 240 mg/day, and 180 mg/day on day preoperative day 2, 1, operation day, postoperative day 1, 2, and 3, respectively. Prednisolone (30 mg/day) was prescribed beginning on postoperative day 4 and was rapidly tapered to a dose of 10 mg/day by 1 month post-transplantation.
All ABOi recipients received cytomegalovirus (CMV) prophylaxis (valganciclovir) for 3 months post-operatively, regardless of CMV serostatus. All ABOc and ABOi recipients received Pneumocystis jiroveci prophylaxis (trimethoprim, 80 mg/day; sulfamethoxazole, 400 mg/day) for 6 months and fungal prophylaxis (fluconazole, 100 mg/day) for 1 month.
All patients receiving ABOi KT were treated before transplantation with an every other day PE (one plasma volume exchanged with 5% albumin) followed by 100 mg/kg of IVIG. The final preoperative PE and all post-operative PEs were performed with donor blood type fresh frozen plasma. The number of pre-transplant PEs was determined by the baseline of ABO Ab titer [6]. The acceptant criterion of anti-blood type Ab titer was ≤1:32 at the time of transplantation. Postoperative PE was performed only if there was a rise in ABO Ab with concomitant impairment of the graft function except for the first case. ABO Ab titers were determined using an established tube test [10].
To compare the baseline characteristics of two groups, the following data were collected: donor and recipient age at KT; previous history of KT; gender; cause of ESRD; type and duration of renal replacement therapy; pre-operative comorbidity (e.g., diabetes mellitus, hypertension); previous blood transfusion, pregnancy, or erythropoietin treatment; number of human leukocyte antigen (HLA) mismatches; presence of panel reactive antibody (PRA) and donor-specific HLA antibody; serologic status of CMV and Epstein-Barr virus; nephron mass; and total ischemic time. To evaluate and compare the outcome; data on patient and graft survival; incidence of biopsy proven acute rejection, renal function, infections, medical, and surgical complications; duration of hospital stay; and re-admission episodes were collected until post-transplant 90th day.
Graft function was assessed by recording serum creatinine (SCr), estimated glomerular filtration rate (eGFR) using the modification of diet in renal disease (MDRD) formula, urine protein-to-creatinine ratio (UPCR) on post-transplantation day 7, 30, 60, and 90. Recipients who experienced allograft loss were excluded from the analysis after the point of graft loss.
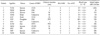
Donor and recipient baseline characteristics were similar in both groups, except for sensitization (PRA ≥ 20% in 41.7% of ABOi recipients and 12% of ABOc recipients) and cold ischemic time (56.3 ± 13 minutes in ABOi recipients vs. 47.1 ± 9.7 minutes in ABOc recipients; P = 0.008, respectively) (Table 1).
Results are summarized in Tables 2, 3. Twelve adult ABOi patients (mean age, 45.6 ± 9.7 years; range, 28 to 61 years; seven males and five females) were successfully transplanted at our institution since May 2009. There were B incompatibility in eight cases and A incompatibility in four cases. Elevated pre-treatment ABO Ab titers ranged from 32 times to more than 1,024 times. Median higher ABO Ab titer were 256 (32 to 1,024), 8 (4 to 64), 8 (0 to 16), 4 (2 to 64), 8 (2 to 64), and 8 (2 to 128) on pre-treatment day 0, 7, 30, 60, and 90, respectively. When compared with the pre-treatment level, the reduction of Ab titer was observed at all time points except patient number 6. The mean number of pre-operative PEs needed to achieve a target ABO Ab titer of 1:32 was 7.2 ± 2.3 (3 to 12) and the mean number of post-operative PE in four patients was 2.8 ± 1.3 (1 to 44).
Overall patient survival was 100% in both groups for 90 days post-operatively. Graft survival was 98% in the ABOc group and 92% in the ABOi group on post-transplant 90th day. In the ABOc group, one graft loss and one delayed graft function occurred. The graft loss was due to an acute cellular rejection on post-operative day 21 and the failed graft was removed. One graft was removed in the ABOi group on post-operative day 22 because of uncontrolled bleeding from biopsy site (Table 4). The graft was removed. SCr, eGFR by MDRD, and UPCR obtained on postoperative day 7, 30, 60, and 90 revealed no significant difference between the two groups. The ABOi patients displayed slightly better (but statistically insignificant) renal allograft functions on those days (Table 4).
All rejections were confirmed upon biopsy. The incidence of acute rejection was 16% and 25% in the ABOc and ABOi group, respectively (P = 0.515). In the ABOc group, seven patients experienced eight episodes of acute rejection, one acute antibody mediated rejection (AAMR) and seven acute cellular rejection. In the ABOi group, three suffered acute rejection, one AAMR and two acute cellular rejections (Table 4).
All infectious, medical, and surgical complications are listed in Table 5. No difference was apparent between the two groups.
There were no serious and lethal infectious complications. No significant differences were evident in the incidence of viral, bacterial, and fungal infection between the two groups (P = 0.691, 0.185, and 1.000, respectively). CMV infection occurred in 11 patients (22%) of the ABOc group and in three patients (25%) of the ABOi group. Two other patients (4%) in the ABOc group experienced CMV disease in a renal allograft (n = 1) and the duodenum (n = 1). All cases of CMV infection and disease were successfully treated by ganciclovir treatment. Seven patients had positive polyoma BK virus replication in the blood but none developed polyoma virus associated nephropathy. Nine cases of bacterial infection developed only in the ABOc group; seven cases were urinary tract infections that responded well to antibiotic treatment.
Overall, there was a trend toward increased medical complications in the ABOi group compared to the ABOc group (50% vs. 22%, respectively; P = 0.051). Leukopenia and post-transplant diabetes mellitus developed more frequently in the ABOi group compared with the ABOc group (leucopenia: 16.7% vs. 2%, respectively; P = 0.093) (diabetes: 30% vs. 14.6%, respectively; P = 0.406). The overall incidence of surgical complications was similar between the two groups (P = 0.686). Major bleeding complications requiring operation or transfusion with more than two units of packed red cells were more frequent in the ABOi group (25%) than in the ABOc group (18%), but this difference was not statistically significant (P = 0.08). Three cases of deep vein thrombosis occurred in the ABOc group.
The goal of ABOi KT is to increase the number of KTs and to avoid or shorten the time on dialysis. For ABOi donors to become widely used in KT, the allograft function and potential risks must be equal to those after ABOc KT. Yet, comparative data is lacking. Presently, ABOi KT recipients (n = 12) were compared for 3 months after KT with 50 ABOc KT patients whose regimen had included the same basic immunosuppression. This short-term study demonstrated that the outcomes of ABOi KT using PE plus rituximab is equivalent to that from an ABOc KT in terms of patient survival, graft survival, graft function, post-operative complications, and total hospital stay.
Unfortunately, in up to one-third of cases, kidney donation is refused due to blood group incompatibility. The use of living donor KT would boost the available transplants by 10 to 20% [6,11,12]. The number of living donor KTs at our hospital has increased by 12% (from 60 to 72) since the start of the ABOi KT program in May 2009. ABOi KT performed in a donor exchange program will likely increase the number of living donor KTs.
Before this goal can be achieved, protocols to overcome the ABOi barrier will be necessary for successful ABOi KT. As an initial approach, PE with splenectomy was used, but more widespread implementation was frustrated by the high rates of infection and rejection [5,13]. However, in the modern era of immunosuppression, protocols using PP plus rituximab have led to encouraging results [6-8].
In this study, patient and graft survival of the ABOi group for 3 months after KT was good and did not differ from that of the ABOc group. Even patients with very high initial ABO Ab titers (patients 1 and 9, ≥1,024) were successfully transplanted for 90 days. Therefore, consistent with previous studies, a high initial ABO Ab titer should not be an exclusion criterion for ABOi KT [14,15]. The target ABO Ab titers in our institution is ≤1:16 at the time of transplantation until patient 8, after which the inclusion criteria for ABOi KT was expanded to those with titers of 1:32. The target ABO Ab titers at which a KT can safely be performed are different between each center, due to differences in titration methods, type of PP, and dosage and timing of rituximab use. Some centers aim at a titer level ≤4, while others target a titer level of ≤32 [8,15-17]. Due to use of different detection method, it is difficult to compare the published data on the outcome of ABOi KT. Exact measurement of ABO Ab titers is critical for successful ABOi KT [18]. However, no standard method for quantitative determination has yet been established. In most institutions performing ABOi KT, the tube test is used to determine the ABO Ab titers. However, significant inter-institutional variability in the measurement of ABO Ab can occur [15]. When different techniques were compared, only flow cytometry yielded a very consistent outcome in repeated measurements, indicating its adoption as an international standard to determine ABOi [19-21].
It is well-known that the risk for AAMR after an ABOi KT is highest in the first 2 weeks after the operation, and can correlate with the post-operative ABO Ab titer [22,23]. A very high incidence of graft loss occurs in patients who experienced AMR during this critical period [24]. This has prompted many centers to employ a protocol with routine fixed scheduled post-operative PP during the first 2 weeks after transplantation [25,26]. Although a routine postoperative PP is effective to prevent acute cellular rejection, it can increase cost, prolong hospitalization, and increase the risk of PP-related complications. Recently, many centers have adopted a policy where post-operative PP is done only if there is an increase in the anti-blood type Ab titer to a certain level [15,27] or a rise in ABO Ab titer with concomitant impairment of graft functions [7,8]. We also performed selective postoperative PP if there was a rise in anti-blood type Ab titer with concomitant impairment of renal functions, except for the first case. Elimination of routine postoperative PE did not result in an increased incidence of AAMR in our series. Postoperative PP was performed on only three (27%) of the 11 ABOi recipients. Among them, only one case of AAMR was confirmed, and was successfully treated with four sessions of PE and steroid pulse therapy.
Table 5 shows the type and incidence of complications after living donor KT. Between the two groups, there were no statistical differences in overall complications. Since Tydén et al. [25] reported on ABOi KT without splenectomy using rituximab in 2003, most transplant centers have adopted rituximab instead of splenectomy as a B-cell ablation therapy in ABOi KT. Increased risk of infectious complications have been reported after the use of rituximab for other indications [28,29], but have not been well-studied in solid organ transplantation. One of our major concerns was that the routine administration of rituximab would lead to an increased rate of infectious complications. But, we did not experience an increased risk of infectious complications after ABOi KT, despite rituximab induction. The incidence of CMV infection was the same as the ABOc group (25% vs. 22%, respectively), and CMV disease did not occur in the ABOi group. The incidence of CMV infection was relatively lower than another report [30]. We administered valganciclovir prophylactically in the ABOi group and this is likely the reason why there was a relatively lower incidence and severity of CMV infection compared with other studies and the ABOc group. The rates of positive BKV replication in the blood that did not develop to overt BKV nephropathy were also the same in both groups. Although statistically insignificant, bleeding complications occurred more frequently in the ABOi group, whereas deep vein thrombosis developed only in the ABOc group. These two findings suggest that the ABOi group has an upward tendency to defect on coagulation. A possible explanation for the coagulopathy in our series is the method of PP. Theoretically, PE removes much more coagulation factors than double filtration PP or immunoadsorption [22]. Medical complications tended to occur more often in the ABOi group compared to the ABOc group (50% vs. 22%, respectively; P = 0.051). More post-transplant diabetes mellitus and leukopenia developed in the ABOi group. The higher applied dose of corticosteroid, longer pre-operative use of oral immunosuppressives, and rituximab may have played a role. As expected, pre-operative hospital stay was significantly longer in ABOi recipients, primarily because of the pre-operative PE (P = 0.003). However, post-operative hospitalization was nearly same between the two groups.
We conclude that the short-term results of the ABOi KT using this regimen are equivalent to that of the ABOc KT in patient survival, graft survival, and graft function, without any serious complications.
Figures and Tables
Table 1
Recipient and donor characteristics and recipient comorbidity

Values are presented as number (%) or mean ± SD (range).
RRT, renal replacement therapy; KT, kidney transplantation; Hx, history; Tx, treatment; HLA, human leukocyte antigen; CDC, complement dependent cytotoxicity assay; FCMX, flow-cytometric cross-match test; PRA, panel reactive antibody; Ab, antibody.
Table 3
Higher anti-A/B antibody titer and antibody removal of ABO-incompatible living donor kidney transplantation

References
1. 2008 Annual Data Report [Internet]. Korean Network for Organ Sharing (KONOS). 2010. cited 2010 Jan 2. Seoul: KONOS;Available from: http://konos.go.kr.
2. Current renal replacement therapy in Korea [Internet]. ESRD Registry Committee, Korean Society of Nephrology. 2009. cited 2010 Jan 2. Seoul: Korean Society of Nephrology;Available from: http://www.ksn.or.kr/journal/2009/index.html.
3. Liefeldt L, Giessing M, Budde K, Neumayer HH. Contraindications to living donor kidney transplantation. Dtsch Med Wochenschr. 2005. 130:2039–2042.
4. Alexandre GP, De Bruyere M, Squifflet JP, Moriau M, Latinne D, Pirson Y. Human ABO-incompatible living donor renal homografts. Neth J Med. 1985. 28:231–234.
5. Alexandre GP, Squifflet JP, De Bruyère M, Latinne D, Reding R, Gianello P, et al. Present experiences in a series of 26 ABO-incompatible living donor renal allografts. Transplant Proc. 1987. 19:4538–4542.
6. Montgomery RA, Locke JE, King KE, Segev DL, Warren DS, Kraus ES, et al. ABO incompatible renal transplantation: a paradigm ready for broad implementation. Transplantation. 2009. 87:1246–1255.
7. Toki D, Ishida H, Horita S, Setoguchi K, Yamaguchi Y, Tanabe K. Impact of low-dose rituximab on splenic B cells in ABO-incompatible renal transplant recipients. Transpl Int. 2009. 22:447–454.
8. Genberg H, Kumlien G, Wennberg L, Berg U, Tydén G. ABO-incompatible kidney transplantation using antigen-specific immunoadsorption and rituximab: a 3-year follow-up. Transplantation. 2008. 85:1745–1754.
9. Kong JM, Lee DR, Jeong JH, Choi JH, Lee JO, Lee WR, et al. ABO blood group incompatible living donor kidney transplantation without splenectomy. J Korean Soc Transplant. 2009. 23:71–76.
10. Brecher ME. Technical Manual. 2002. 14th ed. Bethesda: American Association of Blood Banks.
11. Stegall MD, Dean PG, Gloor JM. ABO-incompatible kidney transplantation. Transplantation. 2004. 78:635–640.
12. Segev DL, Simpkins CE, Warren DS, King KE, Shirey RS, Maley WR, et al. ABO incompatible high-titer renal transplantation without splenectomy or anti-CD20 treatment. Am J Transplant. 2005. 5:2570–2575.
13. Tanabe K, Takahashi K, Sonda K, Tokumoto T, Ishikawa N, Kawai T, et al. Long-term results of ABO-incompatible living kidney transplantation: a single-center experience. Transplantation. 1998. 65:224–228.
14. Donauer J, Wilpert J, Geyer M, Schwertfeger E, Kirste G, Drognitz O, et al. ABO-incompatible kidney transplantation using antigen-specific immunoadsorption and rituximab: a single center experience. Xenotransplantation. 2006. 13:108–110.
15. Shimmura H, Tanabe K, Ishida H, Tokumoto T, Ishikawa N, Miyamoto N, et al. Lack of correlation between results of ABO-incompatible living kidney transplantation and anti-ABO blood type antibody titers under our current immunosuppression. Transplantation. 2005. 80:985–988.
16. Tydén G, Donauer J, Wadström J, Kumlien G, Wilpert J, Nilsson T, et al. Implementation of a Protocol for ABO-incompatible kidney transplantation: a three-center experience with 60 consecutive transplantations. Transplantation. 2007. 83:1153–1155.
17. Wilpert J, Fischer KG, Pisarski P, Wiech T, Daskalakis M, Ziegler A, et al. Long-term outcome of ABO-incompatible living donor kidney transplantation based on antigen-specific desensitization. An observational comparative analysis. Nephrol Dial Transplant. 2010. 25:3778–3786.
18. Kobayashi T, Saito K. A series of surveys on assay for anti-A/B antibody by Japanese ABO-incompatible Transplantation Committee. Xenotransplantation. 2006. 13:136–140.
19. Yung GP, Valli PV, Starke A, Mueller RJ, Fehr T, Cesar-Ozpamir M, et al. Flow cytometric measurement of ABO antibodies in ABO-incompatible living donor kidney transplantation. Transplantation. 2007. 84:12 Suppl. S20–S23.
20. Krishnan NS, Fleetwood P, Higgins RM, Hathaway M, Zehnder D, Mitchell D, et al. Application of flow cytometry to monitor antibody levels in ABO incompatible kidney transplantation. Transplantation. 2008. 86:474–477.
21. Valli PV, Puga Yung G, Fehr T, Schulz-Huotari C, Kaup N, Güngör T, et al. Changes of circulating antibody levels induced by ABO antibody adsorption for ABO-incompatible kidney transplantation. Am J Transplant. 2009. 9:1072–1080.
22. Tydén G, Kumlien G, Efvergren M. Present techniques for antibody removal. Transplantation. 2007. 84:12 Suppl. S27–S29.
23. Kumlien G, Ullström L, Losvall A, Persson LG, Tydén G. Clinical experience with a new apheresis filter that specifically depletes ABO blood group antibodies. Transfusion. 2006. 46:1568–1575.
24. Takahashi K. A new concept of accommodation in ABO-incompatible kidney transplantation. Clin Transplant. 2005. 19:Suppl 14. 76–85.
25. Tydén G, Kumlien G, Fehrman I. Successful ABO-incompatible kidney transplantations without splenectomy using antigen-specific immunoadsorption and rituximab. Transplantation. 2003. 76:730–731.
26. Padmanabhan A, Ratner LE, Jhang JS, Duong JK, Markowitz GS, Vasilescu ER, et al. Comparative outcome analysis of ABO-incompatible and positive crossmatch renal transplantation: a single-center experience. Transplantation. 2009. 87:1889–1896.
27. Wilpert J, Geyer M, Pisarski P, Drognitz O, Schulz-Huotari C, Gropp A, et al. On-demand strategy as an alternative to conventionally scheduled post-transplant immunoadsorptions after ABO-incompatible kidney transplantation. Nephrol Dial Transplant. 2007. 22:3048–3051.
28. Kamar N, Milioto O, Puissant-Lubrano B, Esposito L, Pierre MC, Mohamed AO, et al. Incidence and predictive factors for infectious disease after rituximab therapy in kidney-transplant patients. Am J Transplant. 2010. 10:89–98.
29. Grim SA, Pham T, Thielke J, Sankary H, Oberholzer J, Benedetti E, et al. Infectious complications associated with the use of rituximab for ABO-incompatible and positive cross-match renal transplant recipients. Clin Transplant. 2007. 21:628–632.
30. Tanabe K. Japanese experience of ABO-incompatible living kidney transplantation. Transplantation. 2007. 84:12 Suppl. S4–S7.




 ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download