Abstract
Endovascular aneurysm repair (EVAR) for the treatment of abdominal aortic aneurysm (AAA) is a widely used method, and its decreased invasiveness compared to traditional surgical repair has brought about reduced rates of morbidity and mortality. Several vascular complications related to the procedure have been reported, but non-vascular complications have rarely occurred. We report herein the case of a 78-year-old man who underwent EVAR for AAA and presented with active duodenal ulcer bleeding and acute acalculous cholecystitis as complications after the procedure. We must consider that a wide spectrum of complications may occur following EVAR, and therefore it is important to evaluate the risks of complication and to take the necessary measures to minimize them.
The treatment of abdominal aortic aneurysm (AAA) has shifted from the traditional open graft replacement to the less invasive endovascular approach. Currently endovascular aneurysm repair (EVAR) is being widely used, and complications of this procedure have been reported [1,2], including endoleaks, stent migration, stent occlusion or breaks, and graft infection [3]. Other complications such as ischemic colitis, aortoenteric fistulas [4] and spinal cord ischemia [5] have also been reported, but most of these complications are vascular complications related to either technical problems or vascular compromise. We report herein a case of non-vascular complications after EVAR in the immediate post-procedural period.
A 78 year-old male patient undergoing endoscopic mucosal resection of colon polyps had been incidentally diagnosed of a 4 cm-sized infrarenal AAA, 1.5 to 2 cm distal from the left renal artery, with extension to the right common iliac artery (CIA), 3.8 cm in maximal diameter on computed tomography (CT) scan. However the patient was asymptomatic and therefore the aneurysm was observed. The patient had a past medical history of hypertension (diagnosed 2 years ago) and gout (diagnosed 5 years ago), and both on medications. Two years later, the patient was diagnosed of prostate cancer and underwent robot-assisted laparoscopic prostatectomy. During the work-up for the operation, the aneurysm was detected on CT scan but the AAA size was unchanged (4 cm) and the patient remained asymptomatic. Postoperatively, the patient suffered from deep vein thrombosis (DVT) needing the insertion of an inferior vena cava filter and anticoagulation.
During the next 8 months, the maximum diameter of the aorta grew to 4.2 cm and that of the right CIA to 4.3 cm, with the aneurysm extending also to the proximal left common iliac artery (Fig. 1). Because of the large sized, rapid growth of right common iliac artery aneurysm, we decided to perform an EVAR procedure. It was planned and performed in two stages. The first stage was the embolization of the right internal iliac artery using a 16 mm vascular plug and the second stage was an EVAR procedure under general anesthesia using a bifurcated modular aortic stent graft (Zenith®, Cook Inc, Bloomington, Indiana, USA). During EVAR, intravenous 5,000 unit heparin injection was done for preventing graft thrombosis. Intraopertive minimal transfusion with red blood cell 1 pint was done, and hemoglobin was slightly dropped from 11.6 g/dL to 10.8 g/dL without definite change of vital sign after EVAR. The overall procedure was done without any other major complications and both lower extremity pulses were good immediately after the procedure.
Follow-up CT angiography performed on the second day after procedure revealed a type II endoleak with otherwise intact lower limb blood flow (Fig. 2). Also from day 2 after the procedure the patient had a fever of spiking pattern with peak temperatures of up to 39.6℃ and a leukocytosis of 19,000/mm3. At that time, systolic blood pressure was 105 mmHg with a hemoglobin level of 10.4 g/dL. On day 4 the patient presented with sudden onset of hypotension (systolic BP <80 mmHg), tachycardia (>120/min), anemia (Hb 5.9 g/dL), oliguria and melena as well as continued spiking fever, leukocytosis, elevated C-reactive protein and hyperbilirubinemia (total bilirubin 1.5 mg/dL). CT scan revealed active bleeding from the second portion of duodenum and the wall thickening of gallbladder with pericholecystic abscess and inflammation (Fig. 3), indicating the presence of acute acalculous cholecystitis. Esophagogastroduodenoscopy revealed a huge exposed vessel with bleeding at the duodenal bulb, probably due to duodenal ulcer bleeding and hemoclipping was performed. However the patient's anemia and melena did not improve and angiography revealed active bleeding at the duodenal branch of the anterior pancreaticoduodenal arcade, which was embolized using a mixture of glue/lipiodol and gelfoam (Fig. 4A, B). Furthermore a percutaneous drain was inserted in the gallbladder in order to decompress the inflamed gallbladder, and nature of drain revealed out an infected bile. A delayed laparoscopic cholecystectomy was performed one month after the EVAR. The patient was discharged on day 35 and is currently being followed-up in an outpatient basis with resumption of his normal activities. The most current follow-up CT angiogram shows decreased but still existent type II endoleak, but without any other complications (Fig. 5).
This case shows various complications of a patient who underwent EVAR for AAA. Many complications after EVAR have been reported, including endoleaks, stent migration and stent rupture [3], aortoduodenal fistula [4] and spinal cord ischemia [5]. However, these complications are mainly vascular complications. Review of the literature has shown that non-vascular complications following EVAR are very rare. The only non-vascular complication reported up to date is the report of a case of acute pancreatitis as a complication of EVAR [6].
This case describes ulcer bleeding and acute cholecystitis as complications of EVAR. The patient had spiking fevers and leukocytosis starting from day 2 after the procedure. At the time, the differential diagnosis was either post-implantation syndrome or lung atelectasis. Retrospectively reviewing the case, these differential diagnoses could have had some influence in the patient's fever, but there is a high probability that the cause of the spiking fever was due to acute cholecystitis. We suggest that cholecystitis may have occurred due to the stressful condition after the procedure. There have been several reports of stress-induced acute acalculous cholecystitis, especially postoperatively [7,8]. Furthermore, the fact that the patient had undergone EVAR under general anesthesia and that there was no evidence of cholecystitis or calculus before the procedure favor the causal relationship between the procedure and the acute acalculous cholecystitis.
The patient presented with melena and other signs of bleeding (hypotension, tachycardia and anemia) from day 4 after the procedure. Workup showed active bleeding from a duodenal ulcer, which was controlled both endoscopically and angiographically. It is probable that the bleeding may have occurred from an indolent, preexisting duodenal ulcer, although there is no esophagogastroduodenoscopy to confirm this theory. Such bleeding may have occurred due to the fact that the patient had been on warfarin for more than 8 months for a previous DVT and had switched to low molecular weight heparin for 4 to 5 days before and after the procedure. This increased bleeding tendency, and the stressful condition after the procedure may have accounted for the ulcer bleeding, which was controlled successfully.
From this case, we need to emphasize the importance of recognizing the underlying medical and medication histories of patients undergoing a stressful condition such as surgery or other invasive procedures, and to take the necessary precautions for the possibly related events that may occur. Vascular patients, in particular, may have several comorbid conditions, such as cardiovascular or cerebrovascular diseases, and may be on several medications, including antiplatelet agents or anticoagulants. These conditions may increase the risk of bleeding, as well as the incidence of myocardial infarction or cerebrovascular accidents after general anesthesia, and therefore it is important to evaluate the risks of complication and to take the necessary measures to minimize them. The importance of a detailed history and a thorough physical examination needs no further debate, and emphasis on this aspect is needed in patients with vascular diseases.
Figures and Tables
Fig. 1
Maximum intensity projection image shows infrarenal aortic aneurysm involving bilateral common iliac artery and proximal portion of right external iliac artery.

Fig. 2
Follow-up CT angiography at the level of proximal portion of iliac limb shows contrast in the sac consistent with an endoleak.
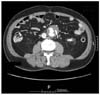
Fig. 3
Computed tomography scan revealed active bleeding from the duodenum second portion and gallbladder wall thickening with pericholecystic abscess and infiltration (arrow).

References
1. Chambers D, Epstein D, Walker S, Fayter D, Paton F, Wright K, et al. Endovascular stents for abdominal aortic aneurysms: a systematic review and economic model. Health Technol Assess. 2009. 13:1–189. 215–318. iii
2. Drury D, Michaels JA, Jones L, Ayiku L. Systematic review of recent evidence for the safety and efficacy of elective endovascular repair in the management of infrarenal abdominal aortic aneurysm. Br J Surg. 2005. 92:937–946.
3. Becquemin JP, Allaire E, Desgranges P, Kobeiter H. Delayed complications following EVAR. Tech Vasc Interv Radiol. 2005. 8:30–40.
4. Ruby BJ, Cogbill TH. Aortoduodenal fistula 5 years after endovascular abdominal aortic aneurysm repair with the Ancure stent graft. J Vasc Surg. 2007. 45:834–836.
5. Berg P, Kaufmann D, van Marrewijk CJ, Buth J. Spinal cord ischaemia after stent-graft treatment for infra-renal abdominal aortic aneurysms: analysis of the Eurostar database. Eur J Vasc Endovasc Surg. 2001. 22:342–347.
6. James AD, Anderson HJ, Edwards R, Sandison AJ. Pancreatitis as a complication of endovascular aneurysm repair. Eur J Vasc Endovasc Surg. 2008. 35:310–311.
7. Fidler F, Prosek V. Acute acalculous cholecystitis as a postoperative complication: the stress gallbladder. Rozhl Chir. 1991. 70:495–497.
8. Schirren J, Dietz W, Rothmund M. Acute acalculous cholecystitis: a stress-induced complication. Chirurg. 1990. 61:382–386.




 Citation
Citation Print
Print




 XML Download
XML Download