Abstract
The incidence of heterotopic gastric mucosa located in the submucosa in resected stomach specimens has been reported to be 3.0 to 20.1%. Heterotopic gastric mucosa is thought to be a benign disease, which rarely becomes malignant. Heterotopic gastric mucosa exists in the gastric submucosa, and gastric cancer rarely occurs in heterotopic gastric mucosa. Since tumors are located in the normal submucosa, they appear as submucosal tumors during endoscopy, and are diagnosed through endoscopic biopsies with some difficulty. For such reasons, heterotopic gastric mucosa is mistaken as gastric submucosal tumor. Recently, two cases of early gastric cancer arising from heterotopic gastric mucosa in the gastric submucosa were treated. Both cases were diagnosed as submucosal tumors based on upper gastrointestinal endoscopy, endoscopic ultrasound, and computed tomography findings, and in both cases, laparoscopic wedge resections were performed, the surgical findings of which also suggested submucosal tumors. However, pathologic assessment of the surgical specimens led to the diagnosis of well-differentiated intramucosal adenocarcinoma arising from heterotopic gastric mucosa in the gastric submucosa.
The recent advancement of endoscopic diagnosis and increase of mass screening test in Korea results in the increase of the incidence of early gastric cancer and submucosal tumor. Gastric cancer and submucosal tumor have different origins. The gastric adenocarcinoma originates from the gastric epithelium, but submucosal tumor does not originate from gastric epithelium. So, their features are different, and the gastric cancer resembling submucosal tumor is very rare. Heterotopic gastric mucosa in the gastric submucosa has been reported of an incidence ranging 3.0 to 20.1% and were considered benign and rarely transformed malignant [1,2]. The gastric cancer arising from heterotopic gastric mucosa in the gastric submucosa is extremely rare, and its feature is similar to submucosal tumor [3,4]. We present two cases of early gastric cancer arising from heterotopic gastric mucosa in the gastric submucosa mimicking submucosal tumor.
A 45-year-old male requested transfer for evaluation of a gastric submucosal tumor found on upper gastrointestinal endoscopy performed during a regular health evaluation. Several months prior to the evaluation, no particular findings existed except for epigastralgia. The medical history, family history, and physical examination showed no particular findings. Upper gastrointestinal endoscopy and endoscopic ultrasound (EUS) showed a 15.8 × 7.8 mm submucosal tumor on the high body of the stomach (Fig. 1A, B). An endoscopic biopsy was performed, and the pathologic diagnosis was chronic gastritis accompanying infection with Helicobacter pylori. According to the abdominal computed tomography (CT), a 17 mm tumor was located in the fundus of the stomach (Fig. 1C). After 6 months, an EUS was performed and the tumor had grown to 18.8 mm in size. The EUS findings suggested that it had malignant potential, such as a lymphoma, so the decision was made to perform a laparoscopic gastric wedge resection for diagnosis and treatment (Fig. 2). At the time of hospitalization, the blood chemistry tests, including tumor markers, showed no abnormal findings. In May 2008, a laparoscopic gastric wedge resection was performed, and at the time of surgery a 2 cm submucosal tumor was found in the fundus of the stomach. A frozen biopsy was not performed because the gross appearance of the tumor appeared benign. No post-operative events occurred. The results of the post-operative pathologic findings were an early gastric cancer (0.5 × 0.5 × 0.4 cm well-differentiated adenocarcinoma) arising from heterotopic gastric mucosa in the gastric submucosa without lymphatic invasion, vessel invasion, or perineural invasion, and in the resection margin no infiltration of tumor cells was found (Fig. 3). We did not perform further treatment because we could not detect metastatic lymphadenopathy on CT and operative findings, and the pathologic finding was the same as the indication of endoscopic mucosal resection (EMR) that was suggested by Tsujitani et al [5]. Currently, the patient is on regular follow-up.
A 50-year-old male requested transfer for further evaluation after detection of a submucosal tumor on upper gastrointestinal endoscopy performed during a regular health evaluation. Except for upper stomach brash symptoms several months ago, the medical history, family history, and physical examination showed no remarkable findings. On upper gastrointestinal endoscopic findings, a submucosal tumor, 20 mm in size and covered with hyperemic mucosa on the greater curvature of the gastric antrum, was found and a biopsy was performed (Fig. 4A). The biopsy results indicated chronic gastritis accompanying an infection with H. pylori. An abdominal CT identified a 20 mm mass on the gastric antrum (Fig. 4B). The endoscopic appearance and the findings on abdominal CT were highly suggestive of a gastrointestinal stromal tumor. We recommended a laparoscopic excision according to the indication of surgical excision of submucosal tumor that suggested by Otani et al [6]. Blood chemistry tests at admission, including tumor markers, showed no abnormal findings. In February 2009, a laparoscopic gastric wedge resection was performed. At the time of surgery, a 2 cm mass was detected on the greater curvature of the gastric antrum; upon visual inspection, the mass was shown to be a gastrointestinal stromal tumor, so we did not perform a frozen biopsy. No post-operative events occurred. The pathologic evaluation revealed a intramucosal adenocarcinoma that was well-differentiated originating from a 1.5 × 1.5 × 1 cm heterotopic gastric mucosa in the gastric submucosa, no tumor infiltration was found at the resection margin, and there was no detected lymphatic, vessel, and perineural invasion (Fig. 5). Because we did not detect metastatic lymphadenopathy on CT and operative findings, and the pathologic finding was the same as the indication of EMR, no further treatment was performed. Presently, the patient is on regular follow-up.
Heterotopic gastric mucosa in the gastric submucosa is reported to occur in 3.0 to 20.1% of resected stomach specimens [2,4,7]. Although the etiology of this disease is unknown, mucosal infoldings bulging in the submucosal tissue have been demonstrated, probably as a result of inflammation or ulceration [2,7]. In addition, the histologic characteristics of heterotopic gastric mucosa with cystic expansion are very similar to gastritis cystic polyposa, but gastritis cystric polyposa is known to occur at anastromotic sites after gastrectomy [8]. Heterotopic gastric mucosa is thought to occur due to infiltration of mucosa through muscularis mucosa cracks or defects by repeated erosion [2]. While heterotopic gastric mucosa occurs due to movement of gastric mucosa to the submucosa through the muscularis mucosa of weak resistance, the muscularis mucosa of heterotopic gastric mucosa is connected with normally located muscularis mucosa, and such a characteristic suggests that it is a true mucosal diverticuli [4]. Although it has not clearly been determined if heterotopic gastric mucosa is due to congenital or acquired causes, heterotopic gastric mucosa is found in 20.1% of gastric specimens from adults, but not in gastric specimens from children, thus it is thought to occur by acquired causes [4,9]. Because heterotopic gastric mucosa is found primarily among adults in their 60s and is not found in autopsies of people <20 years of age, it is presumed to be due to repetitive inflammation [8]. Indeed, both of our cases were accompanied by chronic gastritis associated with H. pylori infections.
Gastric cancers occurring in such heterotopic gastric mucosa are very rare [3,10] and the association with carcinogenesis is controversial. Rubio and Mandai [4] argued that heterotopic gastric mucosa is related to carcinogenesis. Heterotopic gastric mucosa was found in 34 gastric resection samples, and among them, 3 cases were gastric cancer and 1 case was a stomach ulcer. The authors maintained that such findings are associated with the development of gastric cancer. However, other authors contend that heterotopic gastric mucosa is not associated with the development of cancer. Among 1,500 cases of gastric specimens, heterotopic gastric mucosa was found in 160 cases, and among heterotopic gastric mucosae, 15% were associated with stomach ulcers, 9.9% were associated with gastric cancer, 4% were associated with duodenal ulcers, and 11% were associated with chronic gastritis. With such findings, it was maintained that heterotopic gastric mucosa is not associated with gastric cancer [2]. In other studies, heterotopic gastric mucosa resulted in no development of cancer; however, 11.7% of early gastric cancer with a single lesion were accompanied by heterotopic gastric mucosa, which was found in 28.6% of multicentric lesion gastric cancers. Multicentric lesions are frequently accompanied by heterotopic gastric mucosa, and causes include repetitive erosions. The generated heterotopic gastric mucosa grows in the submucosa. Since surface mucosa is more often exposed to inflammation and erosion, surface mucosa are vulnerable to repetitive erosion and regeneration, and that is presumed to be the cause of aberrations in the gastric mucosa and the development of gastric cancer at the surface mucosa. Such findings suggest that heterotopic gastric mucosa is a paracancerous lesion rather than a precancerous lesion [7]. In the cases presented herein, among the 11,100 patients who underwent gastrectomy for gastric cancer at Samsung Medical Center between November 1994 and March 2009, only 2 cases (0.02% of all cases) were diagnosed as gastric cancer of heterotopic gastric mucosa, and it is estimated that heterotopic gastric mucosa does not lead to a high risk of gastric cancer development.
Gastric cancer that originates from heterotopic gastric mucosa is difficult to diagnose, and on endoscopic findings, takes the form of submucosal tumors. In the case of gastric cancer arising from heterotopic gastric mucosa, cancer exists at the submucosa, and cancer components are not exposed on the surface, so biopsy-based diagnoses of gastric cancer are difficult, and based on upper gastrointestinal barium studies and upper gastrointestinal endoscopy, gastric cancer takes the form of submucosal tumors [10]. Since the findings on upper gastrointestinal endoscopy, barium studies, or CT take the form of a submucosal tumor, it was diagnosed as a submucosal tumor before surgery, and thus laparoscopic gastric wedge resection was performed. After surgery, the pathologic evaluation led to a diagnosis of gastric cancer in our cases.
Heterotopic gastric mucosa is considered to be a benign disease, and cancer rarely occurs within it. Since heterotopic gastric mucosa takes the form of submucosal tumors, it is very hard to diagnose. When submucosal tumors are found, the possibility of being gastric adenocarcinoma arising from heterotopic gastric mucosa is very low, but should still be considered.
Figures and Tables
Fig. 1
(A) The endoscopic study revealed a 1.5 cm ovoid, elevated lesion with a central hyperemic depression on the anterior side of the high body. It was covered with normal-appearing mucosa, except for the central portion. (B) The endoscopic ultrasonographic study revealed a submucosal tumor that was 15.8 × 7.8 mm in size as a heterogenous hyperechoic lesion. (C) Abdominal computed tomography finding showed a 1.7 cm submucosal tumor in the gastric fundus.

Fig. 2
(A) Follow-up endoscopic findings 6 months later revealed a submucosal tumor that was slightly increased in size. (B) Endoscopic ultrasonographic finding showed slightly increased size (about 18.8 mm).

Fig. 3
(A) Low power view shows a 0.5 × 0.5 × 0.4 cm well-differentiated intramucosaladenocarcinoma arising from the heterotopic gastric mucosa in the gastric submucosa (H&E, ×40). (B) High power view shows a well-differentiated intramucosaladenocarioma (white arrow, H&E, ×400)
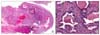
Fig. 4
(A) The endoscopic finding shows the submucosal tumor with normal mucosa on the greater curvature side of the proximal antrum, about 2 cm in size. A round, elevated lesion with normal covering mucosa, hard consistency, and central hyperemia was noted. (B) Abdominal computed tomography finding shows a 2 cm mass in the anterior wall of the gastric antrum.
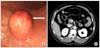
Fig. 5
(A) Low power view shows a 1.5 × 1.5 × 1 cm well-differentiated adenocarcinoma that did not invade the muscularis mucosa arising from the heterotopic gastric mucosa in the gastric submucosa (H&E, ×40). (B) High power view shows a well-differentiated adenocarcinoma (white arrow, H&E, ×400). (C) High power view shows heterotopic gastric mucosa in the gastric submucosa (black arrow, H&E, ×400).

References
1. Matsumoto K, Shida S, Murakami T, Sugiyama Y, Yamagata N, Tsuchida H, et al. Multiple submucosal cysts of the stomach associated with IIc + III type early gastric cancer: report of a case. Gan No Rinsho. 1987. 33:848–853.
2. Yamagiwa H, Matsuzaki O, Ishihara A, Yoshimura H. Heterotopic gastric glands in the submucosa of the stomach. Acta Pathol Jpn. 1979. 29:347–350.
3. Kosugi S, Kanda T, Hatakeyama K. Adenocarcinoma arising from heterotopic gastric mucosa in the stomach. J Gastroenterol Hepatol. 2006. 21:483–484.
4. Rubio CA, Mandai K. Gastric adenocarcinomas in displaced mucosal glands. Anticancer Res. 1999. 19(3B):2381–2385.
5. Tsujitani S, Oka S, Saito H, Kondo A, Ikeguchi M, Maeta M, et al. Less invasive surgery for early gastric cancer based on the low probability of lymph node metastasis. Surgery. 1999. 125:148–154.
6. Otani Y, Ohgami M, Igarashi N, Kimata M, Kubota T, Kumai K, et al. Laparoscopic wedge resection of gastric submucosal tumors. Surg Laparosc Endosc Percutan Tech. 2000. 10:19–23.
7. Iwanaga T, Koyama H, Takahashi Y, Taniguchi H, Wada A. Diffuse submucosal cysts and carcinoma of the stomach. Cancer. 1975. 36:606–614.
8. Littler ER, Gleibermann E. Gastritis cystica polyposa. (Gastric mucosal prolapse at gastroenterostomy site, with cystic and infiltrative epithelial hyperplasia). Cancer. 1972. 29:205–209.
9. Rubio CA. Intramucosal gastric cysts simulating submucosal cysts. Pathol Res Pract. 1989. 184:418–421.
10. Tomonori A, Toshihiro S, Akimichi I, Sei K, Takeshi H, Hitoshi N, et al. Gastric cancer arising from ectopic gastric mucosa glands, report of a case. Stomach Intestine. 2003. 38:1551–1556.




 Citation
Citation Print
Print


 XML Download
XML Download