Abstract
Adult-onset type II citrullinemia (CTLN2) is a disorder caused by an inborn error of metabolism affecting the liver. CTLN2 is an autosomal recessive disorder characterized by recurrent encephalopathy with hyperammonemia due to highly elevated plasma levels of citrulline and ammonia, caused by a deficiency of argininosuccinate synthetase in the liver. A small number of patients have undergone liver transplantation with favorable results. In Korea, the limitations of the deceased donor pool have made living donor liver transplantation a common alternative treatment option. We report the case of a patient with type II citrullinemia who was treated successfully with auxiliary partial orthotopic liver transplantation (APOLT) from a living donor. This is the first description of an APOLT for a patient with adult onset type II citrullinemia in Korea.
Urea cycle disorders (UCD) are among the most common inborn errors of metabolism of the liver. Citrullinemia can be classified into three types: neonatal/infantile (types I and III) and the adult form (type II) [1]. More than 20 patients with citrullinemia have undergone liver transplantation, with favorable therapeutic results [2]. However, the number of cases with auxiliary partial orthotopic liver transplantation (APOLT) is limited. APOLT was initially performed in patients with acute liver failure and non-cirrhotic metabolic liver disease to compensate for enzyme deficiencies without complete removal of the native liver and for small-for-size living donor grafts [3-5]. We report a successful APOLT for the treatment of adult onset type II citrullinemia.
Our patient was a 27-year-old man who was diagnosed with adult-onset type II citrullinemia (CTLN2) at age 24. The patient's height was 178 cm with a body weight of 60 kg. The patient had been treated with a low protein diet and oral administration of lactulose. Intermittent lactulose enemas were provided for intermittent alteration of consciousness. Recently, the patient has had more frequent alterations of his mental status with irritability and altered consciousness. Even though oral administration of L-arginine, Kanamycin and intravenous hyperalimentation with branched chain amino acids was started, his plasma levels of ammonia and citrulline were highly elevated, up to 844 µg/dL (normal range, 19 to 87 µg/dL) and 682 µmol/L (normal range, 12 to 55 µmol/L), respectively. Despite the conservative medical treatment including alternative pathway medication, intermittent continuous renal replacement therapy and hemodialysis, his condition failed to improve. Therefore, living donor liver transplantation was planned using a right lobe graft from his 25-year-old sister. However, the estimated volume of the donor's right lobe was 800 mL compared to 180 mL of the left and in addition there was a type III portal vein anomaly. We eventually decided to perform an APOLT using the extended left lobe of the liver from the donor. The patient underwent APOLT in February of 2008. The actual graft volume was 200 g and the graft-to-recipient weight ratio (GRWR) was only 0.33%. The patient's extended left lobe (including caudate lobe) was resected and the extended left lobe graft (including middle and left hepatic vein) was transplanted orthotopically. The left and middle hepatic vein trunk of the extended left lobe graft was anastomosed to the left and middle hepatic vein trunk of the recipient in end-to-end fashion with interposition venoplasty using the recipient's greater saphenous vein as a patch. The left portal vein of the graft was anastomosed to that of the recipient in end-to-end fashion. Considering that the graft was too small, the recipient's right portal vein was narrowed by surgical clipping, instead of total diversion, for prevention of the development of portal venous hypertension. The left hepatic artery of the graft was anastomosed to that of the recipients in end-to-end fashion. Intraoperative Doppler ultrasonography demonstrated that portal and arterial blood flow were well maintained in both the native liver and the graft. Biliary drainage was accomplished by a Roux-en-Y hepaticojejunostomy. On postoperative day 7, abdominal computed tomography demonstrated orthotopically transplanted small left lobe graft with well-enhanced pattern (Fig. 1). The post-operative course was uneventful and the patient was discharged without any problems. The plasma concentrations of ammonia were at the upper limits of normal, so only a low protein diet (50 g/day) was supplied without any specific medication. On post-operative day 33, the patient reported a sudden severe visual disturbance and the plasma levels of ammonia were noted to have increased up to 209 µg/dL. The estimated computed tomography volume of the graft was decreased to 190 mL and a left portal vein stenosis was suspected. Direct portography was performed and a severe left portal vein stenosis was confirmed. Immediate coil embolization of 8th segmental branch of right anterior portal vein and self-expandable stent placement for left portal vein was performed in order to increase the portal flow to the graft (Fig. 2). On post stent insertion day 7, the calculated computed tomography volume of the graft was increased to 250 mL (Fig. 3). The plasma level of ammonia was within normal range. By the thirtieth postoperative month, the patient had no signs of rejection or vascular problems.
APOLT was initially introduced as a temporary or permanent support for patients with fulminant hepatic failure [6]. Currently, the indications for its use have expanded to include metabolic liver disease. APOLT can provide an adequate hepatic mass to correct underlying enzyme deficiencies in adult patients with UCD. This procedure can be carried out to overcome the limitations of graft volume in living donor liver transplantation [7]. In Korea, deceased donor livers are in limited supply. Therefore, living donor liver transplantation is the only treatment option for patients with metabolic liver disease such as UCD. In this case, the graft weight of 200 g and the GRWR of 0.33% are the smallest graft and lowest margin ever reported to meet the minimum requirements for the demands of adequate metabolic function in adults. The post-operative management of this patient is complicated. Because the remaining native liver function, except for the metabolism of ammonia, is normal, the differential diagnosis including portal steal phenomenon and rejection as well as other problems associated with the vascular system is difficult. Thus the plasma ammonia level is a valuable follow up marker and should be closely monitored in such patients. In addition, careful monitoring of the portal flow to the graft is important for the detection of delayed graft dysfunction. Selective portal vein embolization is a useful method for the increase of portal flow to the graft. In conclusion, APOLT can be a life saving procedure and an effective treatment for patients with adult-onset type II citrullinemia, especially when a deceased donor graft is not available or when candidate donors have insufficient graft volume. However, further confirmation is needed with additional patients and long-term follow-up. How much volume of graft can be transplanted successfully is questionable in cases of inborn error of metabolism, such as UCD.
Figures and Tables
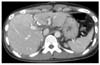
Fig. 1
On postoperative day 7, abdominal computed tomography shows orthotopically transplanted small left lobe graft with well-enhanced pattern.
References
1. Saheki T, Kobayashi K, Inoue I. Hereditary disorders of the urea cycle in man: biochemical and molecular approaches. Rev Physiol Biochem Pharmacol. 1987. 108:21–68.
2. Morioka D, Kasahara M, Takada Y, Shirouzu Y, Taira K, Sakamoto S, et al. Current role of liver transplantation for the treatment of urea cycle disorders: a review of the worldwide English literature and 13 cases at Kyoto University. Liver Transpl. 2005. 11:1332–1342.
3. Bismuth H, Azoulay D, Samuel D, Reynes M, Grimon G, Majno P, et al. Auxiliary partial orthotopic liver transplantation for fulminant hepatitis: the Paul Brousse experience. Ann Surg. 1996. 224:712–724.
4. Inomata Y, Kiuchi T, Kim I, Uemoto S, Egawa H, Asonuma K, et al. Auxiliary partial orthotopic living donor liver transplantation as an aid for small-for-size grafts in larger recipients. Transplantation. 1999. 67:1314–1319.
5. Ikegami T, Nishizaki T, Yanaga K, Kakizoe S, Nomoto K, Ohta R, et al. Living-related auxiliary partial orthotopic liver transplantation for primary sclerosing chonangitis: subsequent removal of the native liver. Hepatogastroenterology. 1999. 46:2951–2954.
6. Gubernatis G, Pichlmayr R, Kemnitz J, Gratz K. Auxiliary partial orthotopic liver transplantation (APOLT) for fulminant hepatic failure: first successful case report. World J Surg. 1991. 15:660–665.
7. Yazaki M, Hashikura Y, Takei Y, Ikegami T, Miyagawa S, Yamamoto K, et al. Feasibility of auxiliary partial orthotopic liver transplantation from living donors for patients with adult-onset type II citrullinemia. Liver Transpl. 2004. 10:550–554.




 Citation
Citation Print
Print




 XML Download
XML Download