Abstract
Neurofibromatosis type 1 (NF-1) is a genetically inherited disorder that may cause skin abnormalities and tumors that form on nerve tissues. These tumors can be small or large and can occur anywhere in the body, including the brain, spinal cord, or other peripheral nerves. Retroperitoneal lymphangiomas are very rare benign malformations of the lymphatic system. About 95% lymphangiomas occur in the skin and the subcutaneous tissues of the head, neck and axillary region and the remaining 5% appear in other parts of the body such as lungs, pleura, pericardium, liver, gallbladder, kidney, and the mesentery. Herein, we report the case of a giant retroperitoneal lymphangioma in a patient with NF-1 with a review of the literature.
Neurofibromatosis type 1 (NF-1) is a genetically inherited disorder that may cause skin abnormalities and tumors that form on nerve tissues. These tumors can be small or large and can occur anywhere in the body, including the brain, spinal cord, or other peripheral nerves.
Retroperitoneal lymphangiomas are very rare, benign malformations of the lymphatic system [1]. About 95% of lymphangiomas occur in the skin and the subcutaneous tissues of the head, neck and axillary region and the remaining 5% appear in other parts of the body such as lungs, pleura, pericardium, liver, gallbladder, kidney, and the mesentery [2].
Herein, we report the case of a giant retroperitoneal lymphangioma in a patient with NF-1 with a review of the literature.
A 59-year-old woman presented with a large, slow-growing mobile mass along with abdominal distension. She was diagnosed as NF-1 and hypertension five years ago.
Physical examination revealed freckling in the axilla and soft, palpable, fluid-filled mass in the abdomen. There were multiple café-au-lait patches and multiple cutaneous neurofibromas on the upper extremities and trunk. Laboratory studies had no specific findings except for microscopic hematuria.
Abdominal computed tomography (CT) revealed a 12.4 × 9 cm sized, well-circumscribed, low-attenuated, large cystic mass lesion compressing the adjacent organs without regional lymphadenopathy (Fig. 1). Positron emission tomography CT revealed a hypometabolic multiple cystic mass in the retroperitoneal space, periheaptic space and left lower extremity. No abnormalities were revealed in laboratory data including tumor markers such as carcinoembryonic antigen and carbohydrate antigen 19-9 .
We suspected a benign giant retroperitoneal cyst and planned a percutaneous drainage because of its proximity to major blood vessels and other organs. The drainage color of lymphorrhea was reddish and not chylous.
The cytologic analysis revealed mostly red blood cells with a few lymphocytes and macrophages. The adenosine deaminase level was 12 and acid-fast bacteria stain findings were negative. The fresh blood-like drainage without clot formation was continued thereafter.
After two days, the patient complained of palpitation and dizziness. The level of Hb dropped to 9 mg/dL and hypotension was checked. On balance, a laparotomy was performed. A giant retroperitoneal cystic tumor attached to the head of the pancreas and extending to the right kidney was identified. Retroperitoneal resection of the cystic mass was conducted successfully. Regarded as doubtful bleeding, left renal cystectomy was added concurrently.
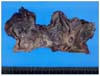
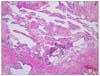
On gross examination, the retroperitoneal mass revealed a well-defined grayish-tan multilocular cystic mass. On cut section, there was a large central cystic space, measuring 6.0 cm in maximum diameter and the inner surface was trabeculated (Fig. 2). The histology showed anastomosing blood vessels and proliferation of mature fat tissue, and smooth muscle with focal bony ossification, displaying a benign vascular tumor (Fig. 3). The central cystic lesion was lined by attenuated endothelial cells and the periphery showed many dilated and anastomosing lymphatic spaces that were lined by endothelial cells. In the surrounding stroma, there was mild patchy aggregation of lymphocytes. In immunohistochemical staining, the lining endothelium was stained with CD34, factor VIII related-antigen and α-smooth muscle actin, except human melanoma black 45 and cytokeratin. The retroperitoneal cystic mass was finally diagnosed as a lymphangioma. The patient was discharged 10 days after operation without complication.
NF-1 is an autosomal dominant genetic disorder that causes tumors to grow on the covering of nerves anywhere in the body at any time [3]. The disorder affects 1 in 3,000 males and females of all races and ethnic groups [4]. NF-1 may affect the gastrointestinal tract in up to 25% of patients.
The incidence of retroperitoneal lymphangioma is very low [1]. Much less so, no report is available on lymphangioma in a neurofibromatosis patient. Clinical presentation varies from asymptomatic masses to abdominal pain. Symptoms are usually related to tumor size and location. If the mass grows large enough to compress adjacent structures and vessels, it can cause significant symptoms and morbidities.
The combined use of ultrasonography, CT and magnetic resonance imaging is very helpful. But, clinical symptoms and radiologic tools may have limitations in accurate diagnosis [5].
Lymphangiomas are classified as simple, cavernous, or cystic types based on their histological findings [6,7]. The simple type is usually situated superficially in the skin and is composed of small thin-walled lymphatic vessels. The cavernous type is composed of dilated lymphatic vessels and lymphoid stroma, and has a connection with spaces of various normal adjacent lymphatics. The cystic type consists of lymphatic spaces.
The differential diagnosis of retroperitoneal lymphangiomas must include other fluid-filled lesions such as pseudocysts, dermoid cysts, lymphoceles or neoplasms like mesotheliomas, pancreatic tumours, lipomas, teratomas, leiomyosarcomas, neurofibromas or liposarcomas. In addition, lymphangioma should be differentiated from hemagioma in case secondary hemorrhage is present.
Beyond all things, it is important to distinguish intra-abdominal lymphangioma from cystic forms of malignancy.
Lymphangioma is characterized by stromal aggregates of lymphocytes, an endothelial lining that usually stains positively with factor VIII-related antigen or CD31, and that is often surrounded by a layer of smooth muscle tissue [8]. In this case report, the appearance of retroperitoneal lymphangioma at the abdominal CT scanning and distinctive pathologic findings are illustrated.
Some authors recommended conservative management in asymptomatic patients, based on a 10% spontaneous regression rate [8].
Although lymphangioma is a benign neoplasm, a larger or symptomatic lymphangioma is treated with resection to prevent recurrence, infection, torsion, rupture and enlargement. Surgery is often required for symptom control or diagnosis.
The definitive treatment of lymphangioma is complete surgical excision. Retroperitoneal cysts are technically more difficult to excise completely because of their proximity to major blood vessels and other organs. Retroperitoneal cysts are often incompletely excised and require multiple operations. For the most part, it should be noted that the 10% postoperative recurrence rate is due to incomplete resection as evinced by positive microscopic resection margins [9].
Aspiration and injection of sclerosing agents such as alcohol and polidocanol into lymphangioma may be recommended in nonsurgical candidates for emergency decompression [10].
In this case, a 12 cm-sized giant retroperitoneal lymphangioma and left renal cyst were surgically removed without any complication. Our case may be the first reported case of lymphangioma in a patient of NF-1.
From this case and literature, we can conclude that an accurate preoperative diagnosis of retroperitoneal lymphangioma in a patient with NF-1 is highly exceptional. Mass resection should be performed whenever possible. To prevent recurrence, complete excision of the retroperitoneal cystic lymphangioma is mandatory.
Figures and Tables
References
1. Kurtz RJ, Heimann TM, Holt J, Beck AR. Mesenteric and retroperitoneal cysts. Ann Surg. 1986. 203:109–112.
2. Takiff H, Calabria R, Yin L, Stabile BE. Mesenteric cysts and intra-abdominal cystic lymphangiomas. Arch Surg. 1985. 120:1266–1269.
3. Torpy JM, Burke AE, Glass RM. JAMA patient page. Neurofibromatosis. JAMA. 2009. 302:2170.
4. Lu-Emerson C, Plotkin SR. The neurofibromatoses. Part 1: NF1. Rev Neurol Dis. 2009. 6:E47–E53.
5. Yang DM, Jung DH, Kim H, Kang JH, Kim SH, Kim JH, et al. Retroperitoneal cystic masses: CT, clinical, and pathologic findings and literature review. Radiographics. 2004. 24:1353–1365.
6. Rieker RJ, Quentmeier A, Weiss C, Kretzschmar U, Amann K, Mechtersheimer G, et al. Cystic lymphangioma of the small-bowel mesentery: case report and a review of the literature. Pathol Oncol Res. 2000. 6:146–148.
7. Allen JG, Riall TS, Cameron JL, Askin FB, Hruban RH, Campbell KA. Abdominal lymphangiomas in adults. J Gastrointest Surg. 2006. 10:746–751.
8. Ordóñez NG. Value of immunohistochemistry in distinguishing peritoneal mesothelioma from serous carcinoma of the ovary and peritoneum: a review and update. Adv Anat Pathol. 2006. 13:16–25.
9. Méndez-Gallart R, Solar-Boga A, Gómez-Tellado M, Somoza-Argibay I. Giant mesenteric cystic lymphangioma in an infant presenting with acute bowel obstruction. Can J Surg. 2009. 52:E42–E43.
10. Jain R, Bandhu S, Sawhney S, Mittal R. Sonographically guided percutaneous sclerosis using 1% polidocanol in the treatment of vascular malformations. J Clin Ultrasound. 2002. 30:416–423.




 Citation
Citation Print
Print



 XML Download
XML Download