Abstract
Purpose
To analyze the outcomes of laparoscopic liver resection compared with open liver resection in patients with hepatocellular carcinoma (HCC).
Methods
Between July 2005 and December 2009, 26 consecutive patients with HCC underwent a pure laparoscopic liver resection, and data from this group (laparoscopic liver resection group, L-group) were compared with a retrospective control group of 29 patients who underwent open liver resection for HCC (open liver resection group, O-group) during the same period. The two groups were matched in terms of demographic data, tumor size, degree of liver cirrhosis, American Society of Anesthesiology score, type of resection, and tumor location.
Results
Median operation time and the amount of intraoperative packed red blood cell transfusion in the L-group were 147.5 minutes and 0.35 units, respectively. The L-group revealed a shorter operation time (147.5 vs. 220.0 minutes, P = 0.031) than the O-group. No difference in perioperative morbidity or mortality rates was observed (3.8, 0 vs. 24.1%, 0%; P = 0.054, non-specific, respectively); the L-group was associated with a shorter hospital stay than the O-group (11.08 vs. 16.07 days, P = 0.034). After a mean follow-up of 23.9 months (range, 0.7 to 59.4 months), the 1-year disease-free survival rate was 84.6% in the L-group and 82.8% in the O-group (P = 0.673).
The indications for laparoscopic liver resection have been widening, even for cancer treatment options [1]. However, laparoscopic liver resection has various efficacy and safety concerns for the procedure, and gas emboli and appropriate bleeding control are technical problems [2]. Second, port-site implantations and tumor cell seeding under a CO2 pneumoperitoneum are of concern to surgeons [2]. However, accumulating data have revealed that these problems have been overcome [3], and laparoscopic liver resection for hepatocellular carcinoma (HCC) seems to offer advantages over conventional open surgery in terms of shortened postoperative recovery [4-9], immunological benefits [10], and smaller volumes of ascites [3,5]. However, most of these studies have reported typically minor hepatic procedures with tumor locations in peripheral liver segments (segments 2 to 6), and few were comparative [3,4,7,11]. Additionally, the oncological results of laparoscopic liver resection for HCC remain a matter of debate.
The aim of this study was to analyze the outcomes of laparoscopic liver resection compared with open liver resection for HCC using a case-matched analysis for tumor size, type of resection (including major hepatectomies), degree of liver cirrhosis, American Society of Anesthesiology (ASA) score, type of resection, and tumor location (including segments 7 and 8).
Between July 2005 and December 2009, 102 patients underwent a liver resection for HCC by a single surgeon, at the Chonnam National University Hwasun Hospital, Korea. Twenty-nine laparoscopic cases were attempted, with three conversions to open hepatectomy (10.3%). The remaining 26 cases were completed laparoscopically. In contrast, 73 patients (71.5%) had an open procedure. Of them, 26 consecutive cases underwent pure laparoscopic liver resection (laparoscopic liver resection group, L-group) and were compared to a retrospective control group of 29 patients who underwent open liver resection for HCC (open liver resection group, O-group) by the same surgeon during the same period. The data of the three cases converted to an open hepatectomy were excluded because of extreme values, to avoid bias. The patients in the two groups were matched for gender, age, body mass index, tumor size, degree of liver cirrhosis, ASA score, type of resection, and tumor location. Three patients underwent conversion to an open approach (10.3%). All procedures were performed according to the same surgical and oncological principles. The patients in the L- and O-groups received similar preoperative assessments and postoperative management.
According to the international consensus meeting on laparoscopic liver surgery [12], the best indication for a laparoscopic liver resection is a patient with solitary lesions and tumors sized 5 cm or smaller and located in peripheral liver segments (segments 2 to 6). Our indications for a laparoscopic procedure were tumors 5 cm or less in size, no major vascular invasion (e.g., main portal vein or main hepatic vein) regardless of the location of the tumor, an ASA score <4, and disease-free margins. Other indications were the same as for an open liver resection. One case with an 8-cm sized mass underwent a laparoscopic operation and was included in this study. The tumor was located in the periphery and had no major vascular invasion. Thus, it was thought that an adequate disease-free margin could be achieved.
All operations were performed under general anesthesia. A pneumoperitoneum was established using CO2 gas and then maintained below 10 mmHg to prevent a gas embolism. Laparoscopic ultrasonography was routinely used to localize tumors and to demonstrate satellite nodules. Patient position, trochar placement, and type of resection were determined according to tumor location. A Harmonic scalpel (Ethicon Endo-Surgery Inc, Cincinnati, OH, USA) was primarily applied for the parenchymal transection. An anatomically major liver resection was usually performed using an intrafascial or extrahepatic approach. The portal pedicles were dissected outside the liver parenchyma, and the portal branch, the arterial branch, and the bile duct were separated. The arterial and portal branches were clipped and divided. When the portal branch was too large to apply clips, it was divided with a linear stapler. The Pringle maneuver was not performed. The resected specimen was inserted into a plastic bag, and retrieved through an extended epigastric port site incision. After meticulous hemostasis, a fibrin glue sealant (Greenplast, Green Cross Co., Seoul, Korea) was sprayed on the cut surfaces. After irrigation, a closed suction drain was inserted, and the wound was closed in layers.
The following operative variables were collected for each patient: demographics, tumor location and histology, size of hepatic lesions, operative details, morbidity, most recent follow-up data, disease-free status (e.g., recurrence vs. non-recurrence), and date of recurrence. Morbidity and postoperative hospital stay were evaluated according to the Clavien complication grading system [13,14]. Patients were monitored for the development of postoperative hemorrhage, pleural effusion, and postoperative fluid collection. Patterns of recurrence were classified as unifocal intrahepatic, multifocal hepatic, and others (e.g., lumbar spine metastasis). Survival status was determined by review of the medical records and through use of the Chonnam Regional Cancer Center death index.
Liver resections were defined according to Brisbane
2000 terminology [15]: left lateral sectionectomy (for a segmentectomy of segments 2 to 3), segmentectomy (for a resection of one segment), right hemihepatectomy (for a segmentectomy of segments 5 to 8), and left hemihepatectomy (for a segmentectomy of segments 2 to 4).
Discharge criteria were the ability to tolerate a soft or regular hospital diet and pain control with oral analgesics. After discharge, all patients were followed with a surveillance protocol that included a multislice computed tomography scan, liver function tests, and serum alpha-fetoprotein level every 3 months after resection for 2 years, then every 4 to 6 months.
Disease-free survival was calculated from the date of the operation to the date of recurrence or last follow-up.
Summary statistics are reported using mean or median values, where appropriate. The Student's t-test and Mann-Whitney U-test were used for the mean comparison of continuous variables and for ordinal data, respectively, whereas the chi-squared and Fisher exact tests were used to compare frequencies of categorical variables between groups. Survival rates were calculated using the Kaplan-Meier method, and survival curves were compared using the log-rank test. Significance was defined as P ≤ 0.05. All statistical analyses were performed using the SPSS ver. 14.0 (SPSS Inc., Chicago, IL, USA).
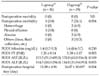
Clinicopathological features and tumor characteristics are summarized in Table 1. Additional parameters, such as transaminase levels, total bilirubin, and prothrombin time, were similar between the L- and O-groups.
The intraoperative clinical outcomes are summarized in Table 2. In the L-group, there were four right hemihepatectomies, one left hemihepatectomy, four segmentectomies, four left lateral sectionectomies, and 13 wedge resections. In the O-group, there were five right hemihepatectomies, two left hemihepatectomies, 10 segmentectomies, three left lateral sectionectomies, and nine wedge resections. No difference was found between the two groups for the type of resection (P = 0.467). Five patients (19.2%) in the L-group and seven patients (24.1%) in the O-group underwent a major (≥three segments) liver resection (P = 0.660), with a 10.3% conversion rate. The median operation time was shorter in the L-group than that in the O-group (147.5 vs. 220.0 minutes, P = 0.031). The total amount of intraoperative packed red blood cell transfusion was 0.35 units in the L-group and 0.45 units in the O-group (P = 0.666). A transfusion was required in five patients (19.2%) in the L-group and seven patients (24.1%) in the O-group (P = 0.660). In both groups, one case had tumor exposure at the surgical specimen surface (R1 resection; P = 1.000). The two groups did not differ significantly in terms of the presence of vascular invasion, satellite nodules, or Edmondson-Steiner grade.
The size of the skin incision in the L-group was 6 to 7 cm for the major (≥3 segments) liver resection hepatectomies and <5 cm for the minor (<3 segments) resections, which was shorter than that in the O-group (about 10 to 15 cm).
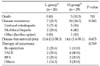
We compared the postoperative clinical outcomes between the two groups (Table 3). No perioperative death was recorded in either group. Postoperative complications occurred in one patient in the L-group (3.8%) and in seven patients in the O-group (24.1%; P = 0.054). Based on the surgical complications classification [13,14], complications in the L-group included grade II pleural effusion, which resolved successfully with diuretic treatment. In the O-group, postoperative complications included one case of grade II hemorrhage, one case of grade III hemorrhage (treated with a re-exploration for bleeding from a resection margin), two cases of grade II abscess, and one case each of ileus (grade II), ascites (grade II), and fluid collection (grade I).
The peak postoperative values of total bilirubin, aspartate aminotransferase, and alanine aminotransferase did not differ statistically between the two groups. However, the prothrombin time value at postoperative day 1 in the L-group was lower than that in the O-group (1.26 vs. 1.38 international normalized ratio, P = 0.003).
The mean hospital stay after surgery was significantly shorter in the L-group than in the O-group (11.08 vs. 16.07 days; P = 0.034).
Follow-up and survival are summarized in Table 4. The mean follow-up period was 21.75 months (range, 0.7 to 58.4 months) for the L-group and 24.75 months (range, 3.6 to 59.4 months) for the O-group. Seven of the 26 patients in the L-group developed disease recurrence (unifocal intrahepatic recurrence, n = 5; multifocal hepatic recurrence, n = 2). No patient developed tumor recurrence at the site of the resection margin, peritoneal dissemination, or port-site metastases. Ten of the 29 patients in the O-group developed tumor recurrence (unifocal intrahepatic recurrence, n = 5; multifocal hepatic recurrence, n = 4; lumbar-spine metastasis, n = 1). The 1-year disease-free survival rate was 84.6% for the L-group and 82.8% for the O-group (P = 1.000) (Fig. 1).
In the L-group, recurrence were treated by further surgery (2 patients), transarterial chemoembolization (transarterial chemoembolization [TACE]; 2), radio-frequency ablation (radiofrequency ablation [RFA]; 2), and refusal of any form of therapy [1], while patients with a recurrence were treated by re-resection [1], TACE [4], RFA [2], radiotherapy [1], and refusal of any form of therapy [2] in the O-group.
No patients died in the L-group, whereas three patients died in the O-group, and median overall survival was 25.6 months (range, 3.6 to 59.4 months).
Since the first report of laparoscopic liver resection by Gagner et al. [16] in 1992, an increasing number of small prospective studies have been published. These studies have reported encouraging results for the feasibility and safety of the procedure. Laparoscopic resection has been more frequently proposed as a curative treatment for HCC [3,6-8,11,17-19] or as a preliminary treatment before transplantation [20].
However, laparoscopic liver resection for HCC is still challenging for both surgeons and patients, because most HCCs are associated with underlying liver disease, such as chronic hepatitis and liver cirrhosis. Moreover, applying laparoscopic resection to HCC has been limited by tumor location. Most reported cases had peripheral lesions located in the anterolateral segments (segments 2, 3, 4b, 5, and 6) [3,7,17-19,21]. Additionally, major liver resections (i.e., right or left hemihepatectomies) are feasible, but remain difficult procedures that should be reserved for experienced surgeons [12]. In our study, tumor location in laparoscopic liver resections included three cases (11.5%) in segment 7 and two cases (7.7%) in segment 8. Five patients (19.2%) in the L-group underwent major (≥3 segments) liver resection. This result suggests that the limitations of laparoscopic resection based on tumor location and the extent of resection will be overcome with further experience and technical advances.
One of the advantages of laparoscopic liver resection is a shorter operation time than for the open method. Aldrighetti et al. [4] reported that the laparoscopic approach resulted in a shorter operating time (150 vs. 240 minutes, P = 0.044) in a case-matched analysis of laparoscopic (n = 16) and open liver resection (n = 16) of HCC. Additionally, Belli et al. [22] reported a retrospective analysis of a prospectively maintained database of 179 liver resections including major hepatectomies. They showed a shorter operating time with laparoscopic versus open liver resection (167 vs. 185 minutes, P = 0.012). These results are comparable with the results of the present study.
Sarpel et al. [9] matched 20 laparoscopic liver resections for HCC to 56 open resections for HCC. The adjusted odds ratio for a length of stay ≥6 days was significantly lower in patients who underwent a laparoscopic resection. These results are comparable with the results of the present study showing a shorter postoperative hospital stay for patients who underwent a laparoscopic resection (11.1 vs. 16.1 days, P = 0.034).
The main concern with using the laparoscopic technique for malignancies is the risk of inadequate tumor resection. However, no difference has been observed in margin-free resections between laparoscopic and open liver resection in many comparative studies [3,5-6,9,12,23-26]. In our series, one case in each group had tumor exposure at the surgical specimen surface (R1 resection); this was not significant (P = 1.000).
Another concern about laparoscopic resection of malignancies is the risk for a port-site tumor recurrence, which was not recorded in our patients. With more than 3,000 cases of minimally invasive hepatic resection in the literature, no incidence of port-site recurrence or tumor seeding has been reported [3-8,22]. Thus, this concern should not prevent surgeons from conducting a laparoscopic approach.
Both groups underwent surgery performed by the same surgeon, confirming the feasibility and safety of the laparoscopic approach when performed by a surgeon with experience in both open and laparoscopic liver surgery. In fact, the mortality and the morbidity rates for the laparoscopic resection group were 0% and 3.8%, respectively.
No prospective, randomized controlled trial has been reported comparing laparoscopic with open liver resection. However, several studies have provided outcomes of matched comparisons between laparoscopic and open hepatic resection for HCC (Table 5). Belli et al. [22] provided the largest matched comparison of laparoscopy (n = 54) with open liver resection (n = 125) of HCC in patients with cirrhosis. Mortalities at 30 days were similar between the two groups; however, morbidity was significantly lower in the laparoscopic group (19 vs. 36%, P = 0.020). The 3-year overall survival (67 vs. 62%, P = 0.347) and disease-free survival (52 vs. 59%, P = 0.864) were not significantly different between the laparoscopic and open groups. These results are comparable with the results of other studies showing an overall 3-year survival of 60 to 93%, and 3-year disease-free survival of 52 to 64% after laparoscopic liver resection for HCC [11,18,19]. In our study, three patients died in the O-group, and the 2-year overall survival rate was 93.1%. No patients died in the L-group during the follow-up period. Thus, overall survival in the L-group could not be calculated and compared with that of the O-group. Nevertheless, our study confirmed the feasibility, safety, and benefits of laparoscopic liver resection for selected patients, including HCCs located in segments 7 and 8 and major hepatectomies.
The results of our study are limited by the non-randomized design, small number of cases, and the selection bias related to the choice of approach based merely on tumor characteristics. Although the potential historical bias was reduced by the study design, resulting in an open resection group that was well matched with a laparoscopic resection group for age, gender, ASA class, tumor location and size, type of liver resection, and degree of liver cirrhosis, our disease-free survival results after laparoscopic liver resection for HCC are short-term results. Thus, a larger group of patients and further examinations (longer-term follow-up) are necessary to analyze the role of laparoscopic liver resection.
In conclusion, the present study showed that laparoscopic liver resection for HCC is feasible and safe in selected patients and can lead to good surgical results with a shorter postoperative hospital stay, shorter operating time, less intraoperative bleeding, and similar outcomes in terms of disease-free survival when compared with open surgery.
Figures and Tables
Fig. 1
Disease-free survival curves after laparoscopic and open liver resection for hepatocellular carcinoma (P = 0.073).

Table 1
Clinicopathological characteristics of patients with hepatocellular carcinoma (HCC)

Values are presented as mean ± SD, median (range), or number (%).
HBV, hepatitis-B virus; HCV, hepatitis-C virus; AFP, alpha fetoprotein; ICG-R15, indocyanine green-retention rate at 15 minutes; PT, prothrombin time; INR, international normalized ratio; AST, aspartate aminotransferase; ALT, alanine aminotransferase; ASA, American Society of Anesthesiologists physical status score.
a)Laparoscopic liver resection-group. b)Open liver resection-group.
References
1. Nguyen KT, Gamblin TC, Geller DA. World review of laparoscopic liver resection-2,804 patients. Ann Surg. 2009. 250:831–841.
2. Mala T, Edwin B. Role and limitations of laparoscopic liver resection of colorectal metastases. Dig Dis. 2005. 23:142–150.
3. Laurent A, Cherqui D, Lesurtel M, Brunetti F, Tayar C, Fagniez PL. Laparoscopic liver resection for subcapsular hepatocellular carcinoma complicating chronic liver disease. Arch Surg. 2003. 138:763–769.
4. Aldrighetti L, Guzzetti E, Pulitanò C, Cipriani F, Catena M, Paganelli M, et al. Case-matched analysis of totally laparoscopic versus open liver resection for HCC: short and middle term results. J Surg Oncol. 2010. 102:82–86.
5. Tranchart H, Di Giuro G, Lainas P, Roudie J, Agostini H, Franco D, et al. Laparoscopic resection for hepatocellular carcinoma: a matched-pair comparative study. Surg Endosc. 2010. 24:1170–1176.
6. Belli G, Fantini C, D'Agostino A, Cioffi L, Langella S, Russolillo N, et al. Laparoscopic versus open liver resection for hepatocellular carcinoma in patients with histologically proven cirrhosis: short- and middle-term results. Surg Endosc. 2007. 21:2004–2011.
7. Kaneko H, Takagi S, Otsuka Y, Tsuchiya M, Tamura A, Katagiri T, et al. Laparoscopic liver resection of hepatocellular carcinoma. Am J Surg. 2005. 189:190–194.
8. Shimada M, Hashizume M, Maehara S, Tsujita E, Rikimaru T, Yamashita Y, et al. Laparoscopic hepatectomy for hepatocellular carcinoma. Surg Endosc. 2001. 15:541–544.
9. Sarpel U, Hefti MM, Wisnievsky JP, Roayaie S, Schwartz ME, Labow DM. Outcome for patients treated with laparoscopic versus open resection of hepatocellular carcinoma: case-matched analysis. Ann Surg Oncol. 2009. 16:1572–1577.
10. Vittimberga FJ Jr, Foley DP, Meyers WC, Callery MP. Laparoscopic surgery and the systemic immune response. Ann Surg. 1998. 227:326–334.
11. Lai EC, Tang CN, Ha JP, Li MK. Laparoscopic liver resection for hepatocellular carcinoma: ten-year experience in a single center. Arch Surg. 2009. 144:143–147.
12. Buell JF, Cherqui D, Geller DA, O'Rourke N, Iannitti D, Dagher I, et al. The international position on laparoscopic liver surgery: The Louisville Statement, 2008. Ann Surg. 2009. 250:825–830.
13. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004. 240:205–213.
14. Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009. 250:187–196.
15. Belghiti J, Clavien P, Gadzijev E, Garden J, Lau W, Makuuchi M, et al. The Brisbane 2000 terminology of liver anatomy and resections terminology committee of the international hepato-pancreato-biliary association: Chairman, SM Strasberg (USA). HPB (Oxford). 2000. 2:333–339.
16. Gagner M, Rheault M, Dubuc J. Laparoscopic partial hepatectomy for liver tumor [abstract]. Surg Endosc. 1992. 6:99.
17. Chen HY, Juan CC, Ker CG. Laparoscopic liver surgery for patients with hepatocellular carcinoma. Ann Surg Oncol. 2008. 15:800–806.
18. Dagher I, Lainas P, Carloni A, Caillard C, Champault A, Smadja C, et al. Laparoscopic liver resection for hepatocellular carcinoma. Surg Endosc. 2008. 22:372–378.
19. Cherqui D, Laurent A, Tayar C, Chang S, Van Nhieu JT, Loriau J, et al. Laparoscopic liver resection for peripheral hepatocellular carcinoma in patients with chronic liver disease: midterm results and perspectives. Ann Surg. 2006. 243:499–506.
20. Laurent A, Tayar C, Andréoletti M, Lauzet JY, Merle JC, Cherqui D. Laparoscopic liver resection facilitates salvage liver transplantation for hepatocellular carcinoma. J Hepatobiliary Pancreat Surg. 2009. 16:310–314.
21. Belli G, Fantini C, D'Agostino A, Belli A, Russolillo N. Laparoscopic liver resections for hepatocellular carcinoma (HCC) in cirrhotic patients. HPB (Oxford). 2004. 6:236–246.
22. Belli G, Limongelli P, Fantini C, D'Agostino A, Cioffi L, Belli A, et al. Laparoscopic and open treatment of hepatocellular carcinoma in patients with cirrhosis. Br J Surg. 2009. 96:1041–1048.
23. Ito K, Ito H, Are C, Allen PJ, Fong Y, DeMatteo RP, et al. Laparoscopic versus open liver resection: a matched-pair case control study. J Gastrointest Surg. 2009. 13:2276–2283.
24. Cai XJ, Yang J, Yu H, Liang X, Wang YF, Zhu ZY, et al. Clinical study of laparoscopic versus open hepatectomy for malignant liver tumors. Surg Endosc. 2008. 22:2350–2356.
25. Endo Y, Ohta M, Sasaki A, Kai S, Eguchi H, Iwaki K, et al. A comparative study of the long-term outcomes after laparoscopy-assisted and open left lateral hepatectomy for hepatocellular carcinoma. Surg Laparosc Endosc Percutan Tech. 2009. 19:e171–e174.
26. Topal B, Fieuws S, Aerts R, Vandeweyer H, Penninckx F. Laparoscopic versus open liver resection of hepatic neoplasms: comparative analysis of short-term results. Surg Endosc. 2008. 22:2208–2213.




 ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download