Abstract
Purpose
Patients with biliary atresia (BA) treated with Kasai portoenterostomy may later develop intractable cholangitis (IC) that is unresponsive to routine conservative treatment. It may cause biliary cirrhosis and eventually hepatic failure with portal hypertension. Control of IC requires prolonged hospitalization for the administration of intravenous antibiotics. To reduce the hospitalization period, we designed a home intravenous antibiotic treatment (HIVA) which can be administered after initial inpatient treatment. In this study, we reviewed the effects of this treatment.
Methods
We reviewed medical records of 10 patients treated with HIVA for IC after successful Kasai portoenterostomies performed for BA between July 1997 and June 2009.
Results
The duration of HIVA ranged from 8 to 39 months (median, 13.5 months). The median length of hospital stay was 5.7 days per month for conventional treatments to manage IC before HIVA and, 1.5 days per month (P = 0.012) after HIVA. The median amount of medical expenses per month was reduced by about one tenth with HIVA. One patient underwent liver transplantation due to uncontrolled esophageal variceal bleeding, but the other nine patients had acceptable hepatic function with native livers.
After several years of managing cholangitis in biliary atresia (BA), we recognized that a small group of patients required prolonged intravenous (IV) antibiotic treatment to prevent recurrent cholangitis. In this group, oral antibiotic treatment was not effective enough to prevent cholangitis, and the discontinuation of IV antibiotic treatment led to recurrent cholangitis attacks. Thus, these patients had intractable cholangitis (IC) that could not be controlled by routine conservative treatment. In addition, the IC was usually associated with intrahepatic biliary cysts (IHBCs) and required hospitalization for several months or several years. The long period of hospitalization occasionally resulted in the breakup of the patient's family, which would be "the worst disaster for the patients." For the management of IC, we developed a home intravenous antibiotic treatment (HIVA) based on the idea of home total parenteral nutrition (TPN) for short bowel syndrome.
To evaluate the role of HIVA in patients with IC following Kasai portoenterostomies, we reviewed records of 10 patients who had been treated at our institution.
We retrospectively reviewed medical records of patients who had been treated with HIVA for IC after successful Kasai portoenterostomies performed for BA between July 1997 and June 2009. Successful Kasai portoenterostomy was defined as when the serum total bilirubin decreased to the level less than 2 mg/dL within 6 months of Kasai procedure. Cholangitis was diagnosed in patients who had underwent the Kasai procedure and then developed fever without another identifiable source of infection plus the following criteria: 1) clinical symptoms such as reappearance of jaundice or acholic stool; and 2) laboratory evidence of sudden elevation of serum bilirubin or liver enzymes (alanine transaminase [ALT] or aspartate transaminase [AST]); or 3) isolation of bacteria on blood culture. IC was defined as recurrent cholangitis for 1) hospitalization for the treatment of cholangitis for longer than 1 month and 2) three consecutive hospitalizations due to cholangitis with an interval less than 1 month between the previous discharge and re-admission. Abdominal ultrasonography, computed tomography or magnetic resonance cholangiopancreatography was performed to detect IHBCs in all patients diagnosed as IC.
When fever subsided and cholangitis was controlled with optimal intravenous antibiotics treatment during hospitalization, a Broviac catheter (Bard Access Systems Inc., Salt Lake City, UT, USA) was placed in the central vein of the patients before they were discharged from the hospital. The catheter was inserted under general anesthesia, and remained for the full course of HIVA. After discharge, home care nurse or the patients' parent(s) or guardians administered intravenous antibiotic treatment via the catheter in the same way it was done during hospitalization. To prevent re-hospitalization due to the recurrent cholangitis a few days later after discharge, they were managed with HIVA after discharge. They were checked up every month at out-patient clinic.
During monthly follow-up at out-patient clinic, the completion time for HIVA was determined. Within 6 to 8 months after HIVA, the discontinuation of HIVA or the switch from HIVA to oral antibiotic treatment was tried without removal of intravenous access. If cholangitis recurred without intravenous antibiotics treatment, HIVA was restarted using the intravenous catheter. If cholangitis did not recur without HIVA for a few months, intravenous catheter was removed and HIVA was completed.
If cholangitis attacks took place during the course of HIVA, patients were re-admitted and blood culture test was performed. Intravenous antibiotics were changed to the other kinds according to the sensitivity test result of blood culture if the resistant strain to the previous antibiotics was found in the blood culture study.
Admission rates (admission days per month of the conservative treatment period) and hospital expenses before HIVA (from the time of diagnosis of IC to the time HIVA started) were compared to those after HIVA (including the cost for HIVA such as drugs and home are nursing, and the cost for follow-up in out-patient clinic during and after discontinuance of HIVA) for each patient by the Wilcoxon signed rank test using the SPSS ver. 13.0 (SPSS Inc., Chicago, IL, USA). The study was approved by our institutional review board (approval number: 4-2009-0529). Anonymity and privacy of the patients were protected.
One hundred six patients underwent Kasai portoenterostomies at our hospital between July 1997 and June 2009. Among them, 90 patients had follow-up records over the last 3 years.
Kasai portoenterostomies were unsuccessful in nine patients. The levels of serum bilirubin never dropped to less than 2 mg/dL after these nine Kasai procedures. Three patients among these nine patients presented with IC. Eighty-one patients were followed-up after successful Kasai procedures. Another patient was referred to our institution for IC management after undergoing a successful Kasai procedure at another hospital. Among these 82 patients whose postoperative levels of serum bilirubin were normalized (less than 2 mg/dL) within 6 months after Kasai portoenterostomies, 13 patients (15.9%) suffered from IC. Only 10 of them received HIVA. HIVA could not be applied for the other three patients because IC was not controlled by intravenous antibiotics treatment during hospitalization. Two of them underwent liver transplantation because of IC, and one died of sepsis and variceal bleeding following IC (Fig. 1).
Table 1 summarizes the clinical characteristics of the 10 patients enrolled in HIVA program. They underwent Kasai portoenterostomies from 23 to 86 days (median, 56 days) of age. The median age at diagnosis of IC was 7 months (range, 4 to 35 months).
Fig. 2 outlines the progression and resolution of IC in some of the patients. Before conceiving the idea of HIVA, we struggled to control recurrent cholangitis by surgical or interventional modalities, such as hepatic cystojejunostomy, revision of portoenterostomy, percutaneous transhepatic biliary drainage, alcohol sclerosing treatment, or metal stent insertion in the initial two patients (patients 1 and 2). In spite of those many attempts, cholangitis attacked recurrently in those two patients. A few days after they were discharged from long hospitalization, they suffered from recurrent cholangitis and were re-admitted. Fig. 3 shows the IHBCs detected after the diagnosis of IC (Fig. 3A) and remained after hepatic cystojejunostomy (Fig. 3B) in patient 1. The time interval between the diagnosis of IC and the start of HIVA in patients 1 and 2 was longer than in other patients (54 months for patient 1 and 28 months for patient 2), because we attempted to treat IC with conventional procedures before using HIVA in these two patients. The unsuccessful outcomes of the interventions for these first two patients led us to develop HIVA. For patients 3 to 10, HIVA was applied as soon as IC was diagnosed. The median interval between the diagnosis of IC and the application of HIVA was 2 months. The duration of HIVA was determined by the tolerance of discontinuance of intravenous antibiotics treatment without recurrent cholangitis in each patient. It ranged from 8 to 39 months (median, 13.5 months) (Table 1).
Cholangitis recurred a few times after completion of HIVA in patients 1, 2, and 5 (Fig. 2). However, it was easily controlled with routine conservative management in hospitalization. All patients, except one (patient 3) who underwent liver transplantation due to variceal bleeding, are free of IC with native liver on last follow-up (median duration of follow-up: 58 months after HIVA) as shown in Table 2. All patients with native liver showed acceptable hepatic function and were jaundice-free. Their serum levels of total bilirubin on last follow-up are listed in Table 2.
IHBCs disappeared on the follow-up abdominal ultrasonography within 2 years after the completion of HIVA in all patients who were followed up. Recurrent IHBCs associated with cholangitis were detected on long-term (more than 2 years) follow-up in only the first two patients for whom application of HIVA was delayed (Table 2). IHBC was not detected in the other five patients (patients 5 to 9) for median duration for follow-up of 40 months (range, 15 to 68 months).
The catheter related complication was occurred in two patients. One patient had catheter infection and the other had catheter occlusion. The complicated catheter was removed and new catheter was reinserted. No patients developed antibiotics related complication.
The median hospital stay with conventional treatment before HIVA was 5.7 days per month and, after HIVA, 1.5 days per month for eight patients for whom this data was recorded. This decrease in the admission rate after the completion of HIVA was significant (P = 0.012) (Table 3). The median amount of medical expenses for IC was about KRW 3.22 million per month before HIVA. It was reduced by about one tenth to KRW 392,806 per month after the initiation of HIVA. These results show that the median value of monthly medical expenses significantly decreased when HIVA was applied (P = 0.012).
Cholangitis is a common complication that develops after Kasai procedures for BA [1]. The reported incidence of postoperative cholangitis in BA ranges from 40 to 93% [2]. IC that cannot be controlled by routine conservative treatment may lead to biliary cirrhosis and hepatic failure with portal hypertension. IC is considered as one of the most important and difficult complications to manage after Kasai portoenterostomy because of the poor prognosis and the occasional requirement of liver transplantation. Recurrent cholangitis is one of the most important determinants of prognosis after a successful Kasai procedure. The number of cholangitis episodes negatively affects long-term postoperative survival. IHBCs favor bacterial persistence and cause recurrent cholangitis [3]. The reported incidence of IHBCs after hepatic portoenterostomy in biliary atresia ranges from 6.4 to 25.3% [4-7]. Major complications that induce mortality from recurrent cholangitis include massive variceal bleeding and hepatic failure [8]. For these conditions, aggressive treatment and preventive modalities are needed.
In our patients with IC, cholangitis was not controlled by routine conservative management including intravenous antibiotics treatment during hospitalization. In less than one month, cholangitis recurred and the patient must be re-admitted. Frequent recurrence of cholangitis made the patients' hepatic function poorer. The patients and their parents' quality of life also became poorer after prolonged and repeated hospitalization for cholangitis treatment.
Many surgical and medical treatments have been suggested for cholangitis and IHBCs, including systemic antibiotic therapy [4,7], percutaneous transhepatic cholangiodrainage (PTCD) [4,5,7,9], alcohol injections [4], revision of portoenterostomy [4,10], laparotomy with internal intestinal drainage of an IHBC [5], Roux-en-Y reconstruction by limb lengthening and antireflux valve creation for mechanical problems related to bile drainage in Roux-en-Y limb [11], and liver resection for the localized IHBC [12]. These treatment modalities are limited in their ability to manage refractory cholangitis or IHBCs. PTCD is not effective in cases of noncommunicating cysts, and is difficult if the cysts are located in the porta hepatis because of the risk of jejunal or portal injury [4]. Bu et al. [7] reported that IHBCs disappeared with PTCD in only one of 39 patients with multiple IHBCs. Surgical intervention is also difficult to perform if cysts are located in the deep portion of the liver [4]. In the first two patients (patients 1 and 2) of 10 patients who received HIVA, huge IHBC was drained by PTCD to resolve the IC because the IHBCs detected on imaging study were considered to be the infectious source of IC (Fig. 3A). However, cholangitis was not controlled by PTCD. We struggled to control IC with other interventions. To control IC in these initial two patients, we performed alcohol injections via the PTCD catheter, hepatic cystojejunostomy, internal metal stent insertion, or revision of portoenterostomy, but cholangitis still did not resolve (Fig. 2, 3B). Failures of the above interventions led us to conceive of the HIVA program. Patients can be treated with IV antibiotics effective against cholangitis during a brief initial hospitalization and then discharged with HIVA. They can continue the treatment at home for a few months, controlling cholangitis.
During the HIVA follow-up period, cholangitis attacks became controllable in short hospitalization. The frequency of cholangitis attack was reduced after HIVA application. In some patients, there was no cholangitis event at all after HIVA. Their hepatic function did not deteriorate during long-term follow-up, and they are good enough with their native liver. HIVA may be an effective primary treatment for IC after successful Kasai procedures for BA. IHBCs related to IC can also be controlled and resolved with HIVA. IHBCs disappeared on the follow-up imaging studies once recurrent cholangitis was controlled. IHBC recurred with cholangitis in patients 1 and 2. However, cholangitis was controllable with routine treatment, and the size of IHBC was smaller than when it was accompanied with IC. According to the recurrence of IHBC in these 2 patients, the duration of suffering IC before HIVA and the duration before receiving Kasai portoenterostomy may have some important meaning. Considering cirrhotic change from bile congestion, longer the duration of IC or BA not controlled, more the biliary cirrhosis can be aggravated.
Three patients who suffered from IC after successful Kasai portoenterostomies did not respond to continuous IV antibiotics treatment while being hospitalized. In these patients, HIVA could not be applied (Fig. 1). One of them died from uncontrolled cholangitis and subsequent sepsis and variceal bleeding. In such a case, liver transplantation should be considered. The other two patients underwent liver transplantation, and the graft functioned well without recurrent cholangitis after transplantation. If IC initially respond to IV antibiotics, HIVA can be applied to reduce the likelihood of high morbidity from liver transplantation. Before considering liver transplantation for IC, HIVA can be applied with effective IV antibiotics. Liver transplantation should be considered if they present hepatic failure or other complications from biliary cirrhosis or portal hypertension even after or during the IC treatment with HIVA as was the case for patient 3.
This would reduce the morbidity and mortality associated with recurrent cholangitis in this population. The length of hospital stay and medical expenses associated with the control of IC can be significantly reduced by HIVA. Moreover, the hospital stay can be shortened or at least broken-up can be avoided by reducing stress placed on the family.
To improve the prognosis of IC or IHBCs, every effort should be made to diagnose IC as early as possible. If a patient with biliary atresia is found to have IC, HIVA should be applied without delay, as this may help maintain hepatic function, and reduce the risk of biliary cirrhosis and reduce length of hospital stay and medical expense.
Figures and Tables
Fig. 1
The occurrence of intractable cholangitis (IC) and the application of home intravenous antibiotic treatment (HIVA) after Kasai portoenterostomies between July 1997 and June 2009.

Fig. 2
Progression and resolution of intractable cholangitis (IC) with home intravenous antibiotic treatment (HIVA): cholangitis events recurred in spite of several attempts to control IC before HIVA in the first 2 patients (patients 1 and 2). IC was eventually controlled by HIVA in all patients. PTBD, percutaneous transhepatic biliary drainage; Tx, treatment.

Fig. 3
(A) Intrahepatic biliary cysts (IHBCs) related to intractable cholangitis in patient 1 shown by magnetic resonance cholangiopancreatography. (B) Remaining IHBCs after hepatic cystojejunostomy in patient 1 shown by computed tomography.
Table 1
Clinical characteristics of 10 patients treated by the home intravenous antibiotic treatment (HIVA) program
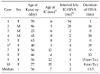
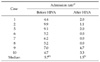
Table 2
Results of home intravenous antibiotic treatment (HIVA)

IC, intractable cholangitis; IHBC, intrahepatic biliary cyst; T.Bil, serum total bilirubin; NC, not checkable due to liver transplantation.
a)Recurred with cholangitis after disappearance of IHBC with HIVA, but the size of IHBC was reduced compare with initial huge one by imaging studies (abdominal US, CT, or MRCP). b)Case of liver transplantation due to esophageal variceal bleeding at 31 months after HIVA. c)Before liver transplantation; d)On HIVA treatment.
References
1. Ecoffey C, Rothman E, Bernard O, Hadchouel M, Valayer J, Alagille D. Bacterial cholangitis after surgery for biliary atresia. J Pediatr. 1987. 111(6 Pt 1):824–829.
2. Ernest van Heurn LW, Saing H, Tam PK. Cholangitis after hepatic portoenterostomy for biliary atresia: a multivariate analysis of risk factors. J Pediatr. 2003. 142:566–571.
3. Luo Y, Zheng S. Current concept about postoperative cholangitis in biliary atresia. World J Pediatr. 2008. 4:14–19.
4. Nakama T, Kitamura T, Matsui A, Makino S, Senyuz OF, Kanazawa K. Ultrasonographic findings and management of intrahepatic biliary tract abnormalities after portoenterostomy. J Pediatr Surg. 1991. 26:32–36.
5. Tsuchida Y, Honna T, Kawarasaki H. Cystic dilatation of the intrahepatic biliary system in biliary atresia after hepatic portoenterostomy. J Pediatr Surg. 1994. 29:630–634.
6. Takahashi A, Tsuchida Y, Suzuki N, Kuroiwa M, Ikeda H, Hirato J, et al. Incidence of intrahepatic biliary cysts in biliary atresia after hepatic portoenterostomy and associated histopathologic findings in the liver and porta hepatis at diagnosis. J Pediatr Surg. 1999. 34:1364–1368.
7. Bu LN, Chen HL, Ni YH, Peng S, Jeng YM, Lai HS, et al. Multiple intrahepatic biliary cysts in children with biliary atresia. J Pediatr Surg. 2002. 37:1183–1187.
8. Wu ET, Chen HL, Ni YH, Lee PI, Hsu HY, Lai HS, et al. Bacterial cholangitis in patients with biliary atresia: impact on short-term outcome. Pediatr Surg Int. 2001. 17:390–395.
9. Kimura K, Hashimoto S, Nishijima E, Muraji T, Tsugawa C, Matsutmo Y. Percutaneous transhepatic cholangiodrainage after hepatic portoenterostomy for biliary atresia. J Pediatr Surg. 1980. 15:811–816.
10. Altman RP, Anderson KD. Surgical management of intractable cholangitis following successful Kasai procedure. J Pediatr Surg. 1982. 17:894–900.
11. Muraji T, Tsugawa C, Nishijima E, Satoh S, Takamizawa S, Ise K, et al. Surgical management for intractable cholangitis in biliary atresia. J Pediatr Surg. 2002. 37:1713–1715.
12. Yamanaka J, Iimuro Y, Hirano T, Kosaka H, Fujimoto J. Successful liver resection for biliary atresia with intrahepatic biliary cysts after Kasai procedure. J Pediatr Surg. 2005. 40:E9–E11.




 Citation
Citation Print
Print


 XML Download
XML Download