Abstract
Purpose
To evaluate the efficacy of B-mode ultrasonography (US) in measurement of carotid stenosis% (CS%).
Methods
One hundred and thirth-three carotid arteries in 96 patients who underwent both carotid US and carotid arteriography (CA) were included in this retrospective study. To measure CS% on US, a cross sectional view of the most stenotic segment of the internal carotid artery was captured and residual diameter and original diameter of that segment were measured with electronic caliper on the same plane and in the same direction. To measure CS% on an angiogram, we used European Carotid Surgery Trial (ECST) and the North American Symptomatic Carotid Endarterectomy Trial (NASCET) methods. Pearson's correlation analysis and linear regression analysis were used to determine the correlation between CS% on an US and angiogram.
Results
Pearson's correlation coefficient (R) between CS% measured in US and CA were 0.853 (ECST method, P < 0.001) and 0.828 (NASCET method, P < 0.001). Accuracies of B-mode US were 93.2%, 88.0%, and 81.2% for estimating CS% by ECST method and 86.5%, 82.7%, and 82% for estimating CS% by NASCET method.
According to the current guidelines, the indications for treatment of carotid artery stenosis are based on the presence of clinical symptoms and the degree of carotid stenosis% (CS%) [1]. For decades, trans-femoral contrast angiography has been used as the gold standard for measurement of the CS%. However, transfemoral carotid arteriography (CA) cannot be used as a routine diagnostic procedure because of its invasiveness, potential risk of cerebral infarction due to carotid artery embolism and the side effects associated with the contrast agent. To avoid an invasiveness of transfemoral CA, computed tomography angiography or magnetic resonance angiography were also used in the diagnosis of carotid stenosis.
CA provides only luminogram showing features of arterial lumen and narrowing or dilatation of the artery. But it cannot show lesion morphology in the arterial wall and outside of the arterial wall. On the contrary, US shows plaque morphology in the arterial wall on a B-mode image and the physiological characteristics of blood flow including flow velocity and flow direction. Because of its non-invasiveness, US has become more frequently used for the diagnosis of carotid artery disease. However, CS% measured on a B-mode US has not been accepted as an independent diagnostic test in measurement of the CS%.
According to Society of Radiologists in Ultrasound Consensus Conference [2], plaque estimate (diameter reduction) on grey-scale or color Doppler US image was used as a primary parameter of criteria for the diagnosis of CS. But that image parameter was just classified into less than 50% and ≥50% not as an independent criterion for measurement of carotid stenosis.
In current practice, duplex US machine is equipped color-coded Doppler sonography, power Doppler and B-mode US image with higher resolution. Considering the advanced equipment and technique of US machine, we can assume that a more accurate measurement of vessel lumen is available with US than before.
In this study, we attempted to determine correlation between CS% measured on B-mode US and CA.
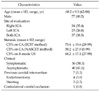
The clinical protocol for this study was approved by the Institutional Review Board. The database of carotid US and arteriogram in 101 patients who underwent both examinations for an assessment of carotid artery stenosis at a tertiary referral center in Seoul, Korea over 3 years from October 2006 to June 2009 were retrospectively reviewed. Among them, 133 carotid arteries (37 bilateral, 59 unilateral) in 96 patients were included for this correlation analysis. One severely calcified artery and five arteries with missing data were excluded. Table 1 shows the clinical and demographic features of the enrolled patients.
All US examinations were performed by experienced registered vascular technologists (RVTs) under the inspection of vascular surgeon and one of the RVTs reviewed the results of examinations. To measure CS% on a B-mode US or color Doppler (Logiq 9, GE Medical Systems, Milwaukee, WI, USA; iU22, Philips Ultrasound, Bothell, WA, USA), the most stenotic segment of the ICA was captured using 9-3 MHz linear transducer on a longitudinal image and by measurement of peak systolic velocity (PSV) at the Doppler angle of insonation 60°. After capturing a transverse scan of the most stenotic segment of ICA on a B-mode US or color Doppler, the original diameter (OD) and residual diameter (RD) were measured using electronic calipers. The RD was defined as the shortest diameter of the residual lumen at the most stenotic segment of ICA and OD was defined as the measured diameter from the outer media to the outer media of the diseased artery on the same plane and at same direction with the RD (Fig. 1). The CS% on B-mode US was calculated using the following equation: CS% = (1 - [RD/OD]) × 100%. This method is used in our institution according to textbooks and previous studies [3,4].
CA was indicated only when the patients are planned for intervention such as, stent insertion and/or balloon dilatation and performed with a trans-femoral catheter on a biplane angiographic system: Allura Xper FD 20/10 system (Phillips Healthcare, Andover, MA, USA) and Altis zee system (Siemens Medical System, Forchheim, Germany). The CA images were reviewed by two investigators who were blinded to the results of the B-mode US exam. There was no significant interobserver variability. The CS% on CA was measured at the most stenotic segment of the internal carotid artery (ICA) according to North American Symptomatic Carotid Endarterectomy Trial (NASCET) and European Carotid Surgery Trial (ECST) methods using electronic calipers on a picture archiving and communication system image. Between anterior-posterior and the lateral views of the carotid artery stenosis, the more stenotic one was selected in measurement of CS%.
To determine a correlation between CSs% on a B-mode US and angiogram, Pearson's correlation analysis and linear regression analysis was conducted. The correlation analysis was performed using CS% on an angiogram measured by NASCET and ECST methods. Receiver operator characteristic curves were generated for sensitivity, specificity, positive predictive value, negative predictive value, and correlation coefficients of CS% on a B-mode US was estimated in subclass of CS% of 50 to 99%, 60 to 99%, and 70 to 99% on arteriogram. The PASW ver. 17.0 (SPSS Inc., Chicago, IL, USA) was used for all statistical calculations.
Table 2 demonstrates the distribution of carotid artery stenosis according to the CS% on B-mode US and arteriogram. The distribution of CS% on B-mode US was more similar to that of ECST method than that of NASCET method.
Correlation between CS% on B-mode US and CA (by ECST method) is shown in the scatter plot diagram (Fig. 2A). The Pearson's correlation coefficient (R) between them was 0.853 (P < 0.001). The following equations were derived by the linear regression analysis:
CS% on CA (by the ECST method) = 0.974 × CS% on B-mode US + 4.075
On a subgroup analysis according to CS%, accuracies of B-mode US were 93.2%, 88.0%, and 81.2% in a subgroup with CS% on B-mode >50%, >60%, and >65%, respectively. The sensitivity, specificity, positive and negative predictive values are listed in Table 3.
The correlation between CS% on B-mode US and CA (by NASCET method) is shown in the scatter plot diagram (Fig. 2B). The Pearson's correlation coefficient (R) between them was 0.828 (P < 0.001). The following equations were derived by the linear regression analysis:
CS% on CA (by the NASCET method) = 1.304 × CS% on B-mode US - 30.711
On a subgroup analysis according to CS%, accuracies of B-mode US were 86.5%, 82.7%, and 82.0% in a subgroup with CS% on B-mode >60%, >70%, and >75%, respectively. The sensitivity, specificity, positive and negative predictive values are shown in Table 4.
In this study, we found a strong positive correlation between CS% measured on B-mode US and an arteriogram which was calculated by either ECST or NASCET method.
The efficacy of carotid endarterectomy for symptomatic and asymptomatic patients with critical stenosis of carotid artery (>50% by NASCET method; >70% by ECST method; >60% by Asymptomatic Carotid Artherosclerosis Study [ACAS] criteria) has already been proven by many prospective randomized trials including NASCET, ECST, and the ACAS [5,6]. In ACAS trial and NASCET, arteriographic measurements were used to determine the degree of carotid stenosis, which was calculated by comparing the residual lumen at the site of maximal stenosis to the lumen of the nondiseased distal ICA.
Although angiographic stenosis of carotid artery was used as a gold standard to give the degree of carotid stenosis in prior trials, each method of calculation is different and has its own drawbacks. In ECST, they used an anticipated outer wall of the carotid bulb as a denominator in calculation of CS% while distal normal ICA was used as a denominator in NASCET and ACAS.
The ECST Method can give the best estimate of plaque thickness which is relevant for the ensuing risk of embolism and the true extent of stenosis. However, angiography enables only a rough and indirect estimate of the local degree of a stenosis because, unlike B-mode US, it does not depict the original vessel diameter. The NASCET method is frequently used in the United States and is reliable but tends to underestimate the degree of stenosis. Some practice guideline recommended not to use NASCET method in patients with a near-occlusive stenotic lesion or with a reduced diameter at the distal internal carotid artery beyond the stenotic lesion [2,7].
In performing duplex US for patients with carotid artery disease, the criteria of CS% can be different from center to center. The main diagnostic parameters of CS% on duplex US is based on velocity criteria. Accordingly, measurement errors due to inappropriate positioning of the Doppler gate or accounting for the Doppler angle can lead to measurement error in diagnosis of the CS% during a duplex US of the carotid artery.
US image of the carotid plaque has not been commonly used for classifying CS% but for determine the presence, location and characteristics of the plaque so far. As described above, diagnostic criteria from Society of Radiologists used ICA PSV, plaque estimate (diameter reduction) on gray-scale or color Doppler US as primary parameter of criteria and ICA/common carotid artery velocity and ICA/end-diastolic velocity as additional parameters [2]. But they suggested only 2 categories of plaque estimate <50% and ≥50% as parameter of CS<50% and CS≥50%, respectively. No more detailed parameter of plaque estimate was suggested to subclassify CS≥50% [8].
With an evolution of US equipment and examination techniques, it has been available to delineate arterial wall layers and measure the thickness of the layer on a US image. In current practice, duplex US has become an initial diagnostic modality of choice in carotid artery disease. However, the duplex US has some limitations with regard to the technical, hemodynamic and anatomic factors. Furthermore, the results of the duplex US are examiner-dependent. Variability between laboratories and between examiners using the same equipment have been previously documented [8-10]. Anatomic factors such as tortuosity or kinking of the carotid artery, hemodynamic factors such as an occlusion of the contralateral carotid artery, the presence of tandem lesion or previous carotid intervention [11-14], and systemic factors such as change of blood pressure or the cardiac output can also influence velocity mesurement of the duplex US [15,16].
The measurements CS% using B-mode US is free from those limitations however, it also has limitations include possibility of angle-dependant measurement bias, difficulties in case with too high carotid bifurcation, severely calcified arterial lesions, echo-lucent lesions, or patients with near-occlusive stenotic lesions. A near-occlusive stenotic lesion can be interpreted as a total occlusion. During the measurement of CS% with B-mode US, eccentric plaque configuration can also lead to a measurement error. However, compared to velocity measurement using duplex US, measurement of the CS% on a hard copy of B-mode US is simple in its technique and examination results are less affected by such technical factors. Another advantage of US over the CA is its ability to assess carotid plaque morphology [17-19].
Some authors have reported the efficacy of CS% measured on B-mode US [2,15,16,20-23]. Among them, some authors reported increased accuracy of B-mode US of carotid stenosis when it is interpreted in conjunction with flow velocity criteria [20,23]. MacKenzie et al. [16] described that the accuracy of CS% on B-mode US was similar to that of velocity criteria in detecting CS% of 50 to 99%, 60 to 99%, and 70 to 99% on TFCA. According to them, the B-mode US image provided the best overall accuracy rates in subgroups of CS of 50 to 99%, 60 to 99%, and 70 to 99% were 85.3% (CS on B-mode US >65%), 82.2% (CS on B-mode US >70%, and 87.0% (CS on B-mode US >78%), respectively. These results are similar to our results in this study. Sprouse et al. [15] suggested that the CS% on B-mode US can be a reliable predictor of carotid stenosis independent of the velocity criteria. According to them, CS% calculated using distal non-stenotic ICA diameter as a denominator and RD of the most stenotic segment of ICA as a numerator (similar to NASCET method) also could be a reliable reliable predictor of carotid stenosis in addition to bulb diameter reduction (similar to ECST method).
Though opponents of B-mode US in the measurement of CS% reported the above-described limitations of US, Sprouse et al. [15] reported that B-mode US assessment was available in 91% of patients. They expected that B-mode US measurement of CS% will be available on more than 95% of patients as examiner's experience and US equipment continues to improve. It was hard for us to determine technical availability of B-mode US examination of the carotid artery in this retrospective study.
In conclusion, although we take some drawbacks of B-mode US in measurement of CS%, we found that US measurement of carotid stenosis was simpler compared to velocity measurement, available in most patients and its results showed a strong positive correlation with CS% measured on transfemoral CA either ECST or NASCET methods (R = 0.853, P < 0.001 and R = 0. 828, P < 0.001, respectively).
Figures and Tables
Fig. 1
Calculation of carotid stenosis% on a transverse scan color flow ultrasonography image of the internal carotid artery: residual diameter (RD) indicates the shortest diameter of residual lumen of the most stenotic segment of the internal carotid artery and original diameter (OD) indicates a diameter from the outer media-to-outer media in a same plane and a same direction with RD.

Fig. 2
Scatter diagrams of the carotid stenosis% (CS%) measured ultrasonography (US) in reference to CS% measured on carotid angiogram. (A) Angiographic CS% measured by European Carotid Surgery Trial method. (B) Angiographic CS% measured by North American Symptomatic Carotid Endarterectomy Trial method.

Table 3
Accuracy of B-mode ultrasonography in measurement of CS% according to the angiographic CS% calculated by the ECST method

References
1. Hobson RW 2nd, Mackey WC, Ascher E, Murad MH, Calligaro KD, Comerota AJ, et al. Management of atherosclerotic carotid artery disease: clinical practice guidelines of the Society for Vascular Surgery. J Vasc Surg. 2008. 48:480–486.
2. Grant EG, Benson CB, Moneta GL, Alexandrov AV, Baker JD, Bluth EI, et al. Carotid artery stenosis: gray-scale and Doppler US diagnosis--Society of Radiologists in Ultrasound Consensus Conference. Radiology. 2003. 229:340–346.
3. Lemne C, Jogestrand T, de Faire U. Carotid intima-media thickness and plaque in borderline hypertension. Stroke. 1995. 26:34–39.
4. Wendelhag I, Gustavsson T, Suurküla M, Berglund G, Wikstrand J. Ultrasound measurement of wall thickness in the carotid artery: fundamental principles and description of a computerized analysing system. Clin Physiol. 1991. 11:565–577.
5. Executive Committee for the Asymptomatic Carotid Atherosclerosis Study. Endarterectomy for asymptomatic carotid artery stenosis. JAMA. 1995. 273:1421–1428.
6. North American Symptomatic Carotid Endarterectomy Trial Collaborators. Beneficial effect of carotid endarterectomy in symptomatic patients with high-grade carotid stenosis. N Engl J Med. 1991. 325:445–453.
7. Higashida RT, Meyers PM, Phatouros CC, Connors JJ 3rd, Barr JD, Sacks D, et al. Reporting standards for carotid artery angioplasty and stent placement. J Vasc Interv Radiol. 2004. 15:421–422.
8. Corriveau MM, Johnston KW. Interobserver variability of carotid Doppler peak velocity measurements among technologists in an ICAVL-accredited vascular laboratory. J Vasc Surg. 2004. 39:735–741.
9. Kuntz KM, Polak JF, Whittemore AD, Skillman JJ, Kent KC. Duplex ultrasound criteria for the identification of carotid stenosis should be laboratory specific. Stroke. 1997. 28:597–602.
10. Mead GE, Lewis SC, Wardlaw JM. Variability in Doppler ultrasound influences referral of patients for carotid surgery. Eur J Ultrasound. 2000. 12:137–143.
11. AbuRahma AF, Robinson PA, Strickler DL, Alberts S, Young L. Proposed new duplex classification for threshold stenoses used in various symptomatic and asymptomatic carotid endarterectomy trials. Ann Vasc Surg. 1998. 12:349–358.
12. Hood DB, Mattos MA, Mansour A, Ramsey DE, Hodgson KJ, Barkmeier LD, et al. Prospective evaluation of new duplex criteria to identify 70% internal carotid artery stenosis. J Vasc Surg. 1996. 23:254–261.
13. Moneta GL, Edwards JM, Papanicolaou G, Hatsukami T, Taylor LM Jr, Strandness DE Jr, et al. Screening for asymptomatic internal carotid artery stenosis: duplex criteria for discriminating 60% to 99% stenosis. J Vasc Surg. 1995. 21:989–994.
14. Moneta GL, Edwards JM, Chitwood RW, Taylor LM Jr, Lee RW, Cummings CA, et al. Correlation of North American Symptomatic Carotid Endarterectomy Trial (NASCET) angiographic definition of 70% to 99% internal carotid artery stenosis with duplex scanning. J Vasc Surg. 1993. 17:152–157.
15. Sprouse LR 2nd, Meier GH, Parent FN, Demasi RJ, Lesar CJ, Nelms C, et al. Are we undertreating carotid stenoses diagnosed by ultrasound alone? Vasc Endovascular Surg. 2005. 39:143–151.
16. MacKenzie KS, French-Sherry E, Burns K, Pooley T, Bassiouny HS. B-mode ultrasound measurement of carotid bifurcation stenoses: is it reliable? Vasc Endovascular Surg. 2002. 36:123–135.
17. Handa N, Matsumoto M, Maeda H, Hougaku H, Ogawa S, Fukunaga R, et al. Ultrasonic evaluation of early carotid atherosclerosis. Stroke. 1990. 21:1567–1572.
18. O'Donnell TF Jr, Erdoes L, Mackey WC, McCullough J, Shepard A, Heggerick P, et al. Correlation of B-mode ultrasound imaging and arteriography with pathologic findings at carotid endarterectomy. Arch Surg. 1985. 120:443–449.
19. Wolverson MK, Bashiti HM, Peterson GJ. Ultrasonic tissue characterization of atheromatous plaques using a high resolution real time scanner. Ultrasound Med Biol. 1983. 9:599–609.
20. Rotstein AH, Gibson RN, King PM. Direct B-mode NASCET-style stenosis measurement and Doppler ultrasound as parameters for assessment of internal carotid artery stenosis. Australas Radiol. 2002. 46:52–56.
21. Jmor S, El-Atrozy T, Griffin M, Tegos T, Dhanjil S, Nicolaides A. Grading internal carotid artery stenosis using B-mode ultrasound (in vivo study). Eur J Vasc Endovasc Surg. 1999. 18:315–322.
22. Golledge J, Ellis M, Sabharwal T, Sikdar T, Davies AH, Greenhalgh RM. Selection of patients for carotid endarterectomy. J Vasc Surg. 1999. 30:122–130.
23. Beebe HG, Salles-Cunha SX, Scissons RP, Dosick SM, Whalen RC, Gale SS, et al. Carotid arterial ultrasound scan imaging: a direct approach to stenosis measurement. J Vasc Surg. 1999. 29:838–844.




 Citation
Citation Print
Print




 XML Download
XML Download