Abstract
Purpose
Hernia repair after recurrence is a challenging procedure, and many approaches have been suggested for it. Total extraperitoneal (TEP) hernia repair should be considered in recurrent hernia. This study was conducted for the purpose of investigating the clinical usefulness of laparoscopic TEP hernia repair for recurrent inguinal hernia.
Methods
Among the 191
patients who underwent TEP hernia repair at these authors' center from June 2006 to January 2010, the bilateral-hernia cases and the patients with a history of previous pelvic surgery were excluded. A total of 19 patients (12.5%) were enrolled in the recurrent-inguinal-hernia group (group R), and 133 patients (87.5%) in the primary-hernia group (group P). Data were investigated retrospectively, based on the medical records.
Results
The mean operation time was 97 minutes in group R and 99 minutes in group P (>0.05). In group R, no operation modality change occurred, and temporary urinary retention was developed in four patients (21.1%). In group P, on the other hand, operation modality change from TEP to the transabdominal preperitoneal approach was necessary in four patients (3%). Additionally, in group P, 30 patients (22.6%) had temporary urinary retention and six (4.5%) had testicular edema. No recurrence was identified during the follow-up period in both groups (mean follow-up period: 15.8 months for group R and 18.0 months for group P).
Inguinal hernia surgery is one of the most commonly conducted surgeries in the world; it is conducted 700,000 cases a year in the United States [1] and is also a very common surgery in South Korea. Since its introduction by Bassini [2] in 1887, various inguinal hernia surgery methods have been introduced by many surgeons. The recurrence rate after inguinal hernia surgery has been reported to be less than 5% in the case of atonic surgery, which was developed by Lichtenstei. As it is technically difficult, however, to conduct reoperation due to adhesion and the deformity of the anatomical structure caused by a previous surgery, the recurrence and complication rates have been reported to be higher by up to 25% [3,4]. Laparoscopic hernia repair has been recognized as an excellent surgery of late and is widely conducted on patients with recurrent inguinal hernia [5]. In this study, laparoscopic total extraperitoneal (TEP) hernia repair was conducted on patients with recurrent inguinal hernia to investigate its clinical usefulness.
Among the 191 patients who were diagnosed with inguinal hernia and who underwent TEP hernia repair at these authors' hospital within the period from June 2006 to January 2010, 24 patients with bilateral hernia and 15 patients with a previous history of pelvic surgery were excluded. Among the remaining 152 patients, 19 patients with recurrent hernia were selected as subjects. The patients with bilateral hernia were excluded as no bilateral hernia existed in the group with recurrent inguinal hernia. Laparoscopic TEP hernia repair was conducted by a single surgeon in all the cases. The gender, age, number and method of the previous surgeries, time elapsed from the surgery to the recurrence, recurrent hernia type, operation time, hospital stay, and recurrence after surgery were retrospectively examined based on the medical records.
Chi-square test was conducted, using SPSS (SPSS Inc., Chicago, IL, USA) for statistical analysis. Statistical significance was pegged at P < 0.05.
In a supine position after general anesthesia, a skin incision was made 15 mm vertically to the directly inferior umbilicus. The anterior rectus sheath in the direction of the hernia was exposed and then incised. The index finger was inserted between the back side of the rectus abdominis muscle and the posterior rectus sheath, and dissection was done inferiorly to create a space for two index finger knuckles. Then a distention balloon was inflated using Spacemaker (Autosuture, Norwalk, CT, USA), with a 10-mm balloon trocar and a distention balloon combined to secure the appropriate space. After removing the balloon, the balloon trocar was filled with about 25 mL air and 12 mmHg CO2 gas, followed by camera insertion. A 5-mm trocar was inserted 5 mm directly superiorly to the pubic symphysis and 5 mm superiorly to the middle of the camera insertion trocar and the pubic trocar to secure the necessary space for the surgery. The space was secured to sufficiently expose the central line and the pubic symphysis internally, the anterior superior iliac spine laterally, Cooper's ligament and the psoas muscle inferiorly, and the rectus abdominis anteriorly. The hernia sac was repaired in almost all the cases (which led to a longer operation time). In the case of large and damaged hernia sacs, they were incised and removed after ligation. Parietex (Sofradim, Formans, France) mesh, which is made of polyester with good compliance and ease of use [6], was used. MIf the patient's height was 175 cm or lower, the 13 × 9 cm size mesh was used, and if the patient was taller than 175 cm, the 15 × 10 cm size mesh was used, based on the previous related experiences. Initially, the mesh was not fixed in patients with unilateral hernia, but it was later fixed at the lateral pubic symphysis, Cooper's ligament, and lateral anterior abdominal wall, respectively, using Tacker (Autosuture), for surgical convenience, since 2009, except for the case of the easy spread of the mesh. When the mesh was sufficiently unfolded, the CO2 gas was blocked and was then slowly released through the trocar on the suprapubic area. After confirming the complete release of the CO2 gas, the trocar was removed, and the surgery was completed.
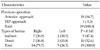
The 152 subject patients consisted of 133 patients (87.5%) with primary inguinal hernia (hereinafter referred to as "group P") and 19 patients (12.5%) with recurrent inguinal hernia (hereinafter referred to as "group R"). The male-to-female ratio was 127:6 for the primary-hernia group and 18:1 for the recurrent-hernia group, showing a higher male proportion. The mean age was 56.4 years for the primary-hernia group and 55.6 years for the recurrent-hernia group. For recurrence, there were 16 first-recurrence cases (84.2%) and three second-recurrence cases (15.8%) (Table 1).
For the time that relapsed from the surgery to the recurrence in the group R, there were two cases (10.5%) with one year or less, two cases (10.5%) with two years or less, three cases (15.8%) with five years or less, three cases (15.8%) with 10 years or less, and nine cases (47.4%) with more than 10 years (Table 2). The previous surgery methods that were used in the recurrent patients were the anterior approach technique (18 cases) and the laparoscopic TEP approach (one case). In all the 18 cases where the anterior approach technique was used, the technique was conducted in other hospitals, and in the case where the laparoscopic TEP approach was used, the approach was conducted in these authors' hospital for the treatment of bilateral inguinal hernia. In the latter case, right recurrence was shown 20 months after the surgery. For the type of recurrent, there were nine cases of indirect hernia (seven cases right, two cases left) and 10 cases of direct hernia (seven cases right, three cases left). The results showed 14 right hernia (73.7%) and five left hernia (23.6%) cases, showing no significant difference in recurrence direction according to the hernia type (P = 0.141) (Table 3).
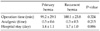
The operation time, number of analgesics used until discharge, and duration of hospital stay after surgery were 99.2 minutes, 0.5 times, and 1.4 days, respectively, in the group P, and 100.1 minutes (110 minutes for recurrence after TEP), 0.3 times, and 1.7 days in the group R, showing no significant difference between the two groups (Table 4).
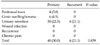
The complications after surgery included four cases of peritoneal rupture and six cases of groin swelling/seroma in the group P. Meanwhile, four cases of urinary retention (22.5%) were found in the group R, but no significant difference was found between the two groups (P = 0.839) (Table 5). All the complications occurred individually in the patients, except for one patient in the group P, who showed both groin swelling and urinary retention. No wound infection, chronic pain, or recurrence was found in both groups. The mean follow-up period after surgery was 18.0 ± 11.3 months in the group P and 15.8 ± 11.9 months in the group R.
There has been a significant change in the inguinal-hernia treatment due to the introduction of Tesionless-hernia repair by Lichtenstein et al. [3] in 1989 since Bassini [2] established hernia repair in 1887 for the first time. Laparoscopic hernia repair has drawn much attention of late as a treatment method for inguinal hernia, and its application has been increasing [5,7].
Laparoscopic hernia repair has a postoperative recurrence rate similar to that of tensionless-hernia repair, and has been considered a good indication for recurrent hernia after the bilateral anterior technique.
The mechanism [8] of the recurrence after inguinal hernia surgery includes the following cases: First, areas with possible hernia occurrence, such as unnoticed femoral defects, are not identified. Second, if the defective area in the inferior inguinal wall is repaired, a separate hernia may occur as more tensile strength is applied to the non-repaired area. Third, metabolic disorder of collagen [9], wherein type III collagen, which cannot be applied to the tensile strength of the skin tissue and the rectus abdominis muscle in patients with recurrent hernia, has a higher concentration compared to type I collagen. In addition, wound infection and unskillful surgical performance have been suggested as causes of recurrence. Small size, placement at an inaccurate position, and incomplete fixation of the mesh are also important causes of recurrence.
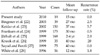
Although the literatures that reported recurrence from the long-term results of laparoscopic TEP hernia repair are not adequate, Taylor and Wilson [10] conducted 100 cases of TEP for two years and reported a five-year recurrence rate of approximately 1%. Czechowski and Schafmayer [11] reported that the five-year recurrence rates of the trasnperitoneal preperitoneal and TEP approaches were 2.3 and 1.5%, respectively; that their re-recurrence rates were 6.7 and 4.8%, respectively; and that the mean times elapsed from the surgery to the recurrence were 45 and 36.6 months, respectively. Scheurlein et al. [12] conducted laparoscopic TEP hernia repair on 179 patients with recurrent inguinal hernia and reported a 0.4% recurrence rate. Ferzil et al. [13] reported that they found no technical or safety issue in the application of the TEP approach to patients who showed recurrence after laparoscopic TEP hernia repair. Despite a smaller subject size and a follow-up period of less than five years, these authors conducted laparoscopic TEP hernia repair on 191 patients with inguinal hernia. As a result, one recurrence case was found, and no recurrence has been found so far in the 19 patients with recurrent hernia after laparoscopic TEP hernia repair, showing excellent outcomes compared to the various related literatures (Table 6). The single recurrence case that was reported in this study was a right recurrent hernia that occurred 20 months after bilateral inguinal hernia surgery using the TEP approach. Re-operation was conducted using the TEP approach, and no recurrence has been found to date, after 19 months. At the time of the surgery, as the mesh was dislocated from its original position and was located at the posterior rectus sheath, the mesh was fixed with Tacker for bilateral hernia.
In the case of TEP conduction due to recurrence after TEP, when the area between the back side of the rectus abdominis muscle and the posterior rectus sheath is dissected and the balloon trocar is inserted after anterior-rectus-sheath incision, and when peritoneal dissection is done to secure the necessary space for the surgery, precautions should be required so as not to cause bleeding and peritoneal rupture.
In the case of recurrent hernia, the importance of mesh [12,14,15] should be emphasized as weakened tissue repair cannot be appropriately done due to tissue weakening, despite its suture.
The complication rate after laparoscopic TEP hernia repair was reported to be 14.59% in a study conducted by Arregui and Nagan [16], 5% in a study by Fitzgibbons et al. [17], 10.67% in a study by Fiennes and Taylor [18], and 16.8% in a study by MacFadyen and Mathis [19]. In the study conducted by MacFadyen and Mathis, the complication rate after posterior peritoneal repair included recurrence (3.2%), testicular edema (1.6%), bladder injury (1%), abdominal distension (0.5%), urinary retention (0.5%), and pelvic osteitis (0.5%); the complication rate after the transabdominal preperitoneal approach included recurrence (0.8%), hematoma (3%), thigh pain (2.2%), scrotal emphysema (2.2%), and urinary retention (1.1%); and the complication rate after the anterior extraperitoneal approach included hematoma (6.6%) and testicular pain (1.1%). Most of the complications were improved with conservative treatments within three weeks. Chronic pain [20,21] has been reported to occur in approximately 9.2-14% after TEP surgery. Chronic pain after TEP surgery is likely to be attributable to nociceptive, neurogenic, and combined pain associated with tissue injury. It is difficult, however, to exactly identify whether the precise cause of the pain is attributable to a neuronal injury occurring during the surgery or to a chronic response to foreign materials due to mesh.
In this study, the complication rate was shown to be 21.1%. No major complications, such as vascular injury, infection, visceral organ injury, hematoma, recurrence, and chronic pain, were found, and four cases of temporary urinary retention were observed.
In conclusion, despite the shorter follow-up period and the smaller subject size, considering its hernia correction which cannot be found in the previous surgeries, advantage of less invasive surgery, and lower complication and recurrence rates, laparoscopic TEP hernia repair can be considered a safe and useful treatment of recurrent inguinal hernia.
References
1. Nathan JD, Pappas TN. Inguinal hernia: an old condition with new solutions. Ann Surg. 2003. 238:6 Suppl. S148–S157.
2. Bassini E. Nuovo metodo per la cura radicale dell'ernia inguinale. Atti Congr Assoc Med Ital. 1887. 2:179.
3. Lichtenstein IL, Shulman AG, Amid PK, Montllor MM. The tension-free hernioplasty. Am J Surg. 1989. 157:188–193.
4. Lichtenstein IL, Shulman AG, Amid PK. The cause, prevention, and treatment of recurrent groin hernia. Surg Clin North Am. 1993. 73:529–544.
5. Feliu X, Torres G, Viñas X, Martínez-Ródenas F, Fernández-Sallent E, Pie J. Preperitoneal repair for recurrent inguinal hernia: laparoscopic and open approach. Hernia. 2004. 8:113–116.
6. Ramshaw B, Abiad F, Voeller G, Wilson R, Mason E. Polyester (Parietex) mesh for total extraperitoneal laparoscopic inguinal hernia repair: initial experience in the United States. Surg Endosc. 2003. 17:498–501.
7. Ferzli GS, Massaad A, Dysarz FA 3rd, Kopatsis A. A study of 101 patients treated with extraperitoneal endoscopic laparoscopic herniorrhaphy. Am Surg. 1993. 59:707–708.
8. Janu PG, Sellers KD, Mangiante EC. Recurrent inguinal hernia: preferred operative approach. Am Surg. 1998. 64:569–573.
9. Klinge U, Zheng H, Si Z, Schumpelick V, Bhardwaj RS, Muys L, et al. Expression of the extracellular matrix proteins collagen I, collagen III and fibronectin and matrix metalloproteinase-1 and -13 in the skin of patients with inguinal hernia. Eur Surg Res. 1999. 31:480–490.
10. Taylor CJ, Wilson T. Long-term results of laparoscopic totally extraperitoneal inguinal herniorrhaphy. ANZ J Surg. 2005. 75:637–639.
11. Czechowski A, Schafmayer A. TAPP versus TEP: a retrospective analysis 5 years after laparoscopic transperitoneal and total endoscopic extraperitoneal repair in inguinal and femoral hernia. Chirurg. 2003. 74:1143–1149.
12. Scheuerlein H, Schiller A, Schneider C, Scheidbach H, Tamme C, Köckerling F. Totally extraperitoneal repair of recurrent inguinal hernia. Surg Endosc. 2003. 17:1072–1076.
13. Ferzli GS, Shapiro K, DeTurris SV, Sayad P, Patel S, Graham A, et al. Totally extraperitoneal (TEP) hernia repair after an original TEPIs it safe, and is it even possible? Surg Endosc. 2004. 18:526–528.
14. Read RC. Recurrence after preperitoneal herniorrhaphy in the adult. Arch Surg. 1975. 110:666–671.
15. Amid PK, Lichtenstein IL. Current assessment of Lichtenstein tension-free hernia repair. Chirurg. 1997. 68:959–964.
16. Arregui ME, Nagan R. Inguinal hernia: advances or controversies. 1994. Oxford: Radcliffe Medical Press.
17. Fitzgibbons RJ Jr, Camps J, Cornet DA, Nguyen NX, Litke BS, Annibali R, et al. Laparoscopic inguinal herniorrhaphy. Results of a multicenter trial. Ann Surg. 1995. 221:3–13.
18. Fiennes AG, Taylor RS. Learning laparoscopic hernia repair: pitfalls and complications among 178 repairs. 1994. Oxford: Radcliffe Medical Press.
19. MacFadyen BV Jr, Mathis CR. Inguinal herniorrhaphy: complications and recurrences. Semin Laparosc Surg. 1994. 1:128–140.
20. Lau H, Patil NG, Yuen WK, Lee F. Prevalence and severity of chronic groin pain after endoscopic totally extraperitoneal inguinal hernioplasty. Surg Endosc. 2003. 17:1620–1623.
21. Amid PK. Causes, prevention, and surgical treatment of postherniorrhaphy neuropathic inguinodynia: triple neurectomy with proximal end implantation. Hernia. 2004. 8:343–349.
22. Bingener J, Dorman JP, Valdes G. Recurrence rate after laparoscopic repair of recurrent inguinal hernias: have we improved? Surg Endosc. 2003. 17:1781–1783.
23. Keidar A, Kanitkar S, Szold A. Laparoscopic repair of recurrent inguinal hernia. Surg Endosc. 2002. 16:1708–1712.
24. Frankum CE, Ramshaw BJ, White J, Duncan TD, Wilson RA, Mason EM, et al. Laparoscopic repair of bilateral and recurrent hernias. Am Surg. 1999. 65:839–842.
25. Järhult J, Håkanson C, Akerud L. Laparoscopic treatment of recurrent inguinal hernias: experience from 281 operations. Surg Laparosc Endosc Percutan Tech. 1999. 9:115–118.
26. Knook MT, Weidema WF, Stassen LP, van Steensel CJ. Endoscopic total extraperitoneal repair of primary and recurrent inguinal hernias. Surg Endosc. 1999. 13:507–511.
27. Sayad P, Ferzli G. Laparoscopic preperitoneal repair of recurrent inguinal hernias. J Laparoendosc Adv Surg Tech A. 1999. 9:127–130.
28. White SI, O'Rourke N, Fielding GA. Laparoscopic mesh repair of recurrent inguinal hernia. Aust N Z J Surg. 1996. 66:91–93.




 Citation
Citation Print
Print




 XML Download
XML Download