Abstract
Purpose
Papillary thyroid cancer with level VII (anterior superior mediastinal lymph nodes) lymph node metastasis belongs to Stage IV a according to the Americal Joint Committee on Cancer cancer staging. The aim of our study was to identify clinicopathologic factors that are related to level VII cervical lymph node metastasis and to suggest recommendations for level VII dissection.
Methods
We reviewed 195 patients with papillary thyroid carcinoma who had their initial operation containing level VII dissection from April 2006 to June 2007. Level VII dissection involved lymph nodes in the anterior superior mediastinum and tracheoesophageal grooves, extending from the suprasternal notch to the innominate artery. Clinicophathologic factors, such as gender, age and lateral neck metastasis, related to Level VII metastasis were analyzed by tumor size, multifocality of tumor, extrathyroidal extension and lymphovascular invasion.
Significant controversy exists with respect to the prognostic significance of lymph node metastasis (LNM) in papillary thyroid carcinoma (PTC). Although several studies have shown that the presence of LNM has no impact on survival [1-4], previous studies by Mazzaferri and Jhiang [5], Scheumann et al. [6], Hughes et al. [7], and Lundgren et al. [8] have demonstrated that LNM is an dependent predictor of cancer mortality. The N category of TNM stage for PTC according to the American Joint Committee on Cancer (AJCC) cancer staging manual 6th edition (2002) are described as follow: first echelon (central compartment/level VI) or N1a, and lateral cervical and/or superior mediastinal or N1b [9]. Level VII (anterior superior mediastinal lymph nodes) LNM particularly belongs to Stage IVa. The manual defines level VII as lymph nodes in the anterior superior mediastinum and the tracheoesophageal grooves, extending from the suprasternal notch to the innominate artery (Fig. 1) [10]. Because level VII LNM is consider to be an important factor for determination of cancer staging and prediction of prognoses, we attempted to identify clinicopathologic factors that are related to level VII LNM and then to suggest recommendations for level VII dissection.
We reviewed 195 patients with PTC who had an initial operation containing level VII dissection from April 2006 to June 2007. There were 30 males and 165 females. The mean patient age was 47.7 years (range, 25 to 74 years). Thyroid lobectomy with central compartment neck dissection (CCND) was performed on 36 patients, total or near total thyroidectomy with CCND on 144 patients, and total thyroidectomy with CCND and modified radical neck dissection on 15 patients.
Level VII dissection is very difficult if the sternum is not opened, but we attempted to perform level VII dissection without opening the sternum. We preferentially dissected anterior superior mediastinal lymph nodes above the innominate artery and vein. After retracting the innominate vessel and the trachea with a Sofield Retractor (long-arm retractor, Medicon Co., Seoul, Korea), we were able to dissect lymph nodes in the tracheoesophageal grooves, extending from the suprasternal notch to the innominate artery (Fig. 2). This technique allowed for level VII dissection without opening the sternum. Thyroidectomy along with level VI and VII dissection was performed as en bloc dissection, and then level VII lymph nodes were separated from the thyroid and level VI lymph nodes (Fig. 3).
Of 195 patients with PTC who had an initial operation involving level VII dissection, 88 (45.1%) showed metastasis to the central compartment, and mean number of dissected central lymph nodes was 12.9, and the mean tumor size was 11.1 mm. Sixty-six patients (33.8%) had extrathyroidal extension, and 57 patients (29.2%) had tumor multifolcality. Fifty-six patients (28.7%) showed lymphovascular invasion (Table 1).
Nine patients (4.6%) showed level VII LNM, and we analyzed clinicophathologic factors related to level VII LNM. Table 2 shows relationships between gender, age, multifocality, extrathyroidal extension and level VII LNM. All patients with level VII LNM were females. The level VII LNM rate was 1.2% for patients aged <45 years and 7.1% for those aged ≥45 years. Five patients (8.8%) with multifocal tumor had level VII LNM. The level VII LNM rate was 7.6% for tumors presenting extrathyroidal extension and 3.1% for those whose tumors did not present extrathyroidal extension. All factors in Table 2 were not significantly related to level VII LNM.
Fifteen patients had lateral neck metastasis, and 4 (26.7%) of the 15 patients had level VII LNM. Of the 180 patients who did not have lateral neck metastasis, 5 (2.8%) had level VII LNM (P < 0.01). The level VII LNM rate was 2.5% for tumors measuring <1.5 cm, 15.6% for those measuring ≥1.5 cm (P < 0.01) (Table 3). The level VII LNM rate was 10.7% for tumors presenting lymphovascular invasion and 2.2% for those whose tumors did not present lymphovascular invasion (P < 0.05) (Table 3). The level VII LNM rate was significantly elevated when there was lateral neck metastasis, tumor size >1.5 cm or lymphovascular invasion.
Complication after level VII LN dissection is that 5 patients (2.6%) had chyle leakage, 4 patients (2%) had right pleural injury, and 1 patient had left innominate vein injury. Four patients (2%) displayed permanent hypoparathyroidism, and 2 patients (1%) displayed unintentional permanent nerve injuries.
It has been generally recognized that surgical resection is the most effective treatment modality for thyroid carcinoma. However, the optimal treatment for differentiated thyroid carcinoma controversial with respect to the extent of thyroid resection, extent and technique of nodal dissection, and use of prophylactic radioiodine therapy [11,12]. Several studies have defined different prognostic factors and treatment strategies for papillary thyroid carcinoma [1,3,5]. Central and lateral compartments are representative of regional lymph nodes related to thyroid carcinoma. Since the central compartment can be dissected through the same incision as thyroidectomy, these nodes have been routinely dissected by most endocrine surgeons. A standardized classification system for neck dissection was published in 1991 [13] with a recent update in 2002 [14]. This neck dissection classification did not recommend inclusion of additional levels such as level VII for the superior mediastinum. It is believed that the 6 levels in current use encompass the complete topographic anatomy of the neck. Level VII is considered to be a specific nodal group. However, according to the AJCC cancer staging, level VII (anterior superior mediastinal lymph nodes) LNM belongs to Stage IVa [9], which means that level VII LNM influences mortality due to PTC. Thus, it is not right that level VII belongs to a specific group, and we should know how many patients with PTC have level VII LNM. Level VII lymph nodes are defined as lymph nodes in the anterior superior mediastinum and the tracheoesophageal grooves, extending from the suprasternal notch to the innominate artery [10]. Level VII nodes have been routinely dissected by most endocrine surgeons, and it has been recognized that level VII dissection is difficult to perform through the same incision as thyroidectomy. Despite the aforementioned results, we were able to dissect level VII lymph nodes through the same incision after retracting the innominate vessel and the trachea with a Sofield Retractor (Medicon Co.) (Fig. 3).
There have been some reports on relations between clinicopathologic factors and LNM. Goropoulos et al. [15] have reported that there is a significant correlation between multicentric tumor and LNM. Hay et al. [16] and Scheumann et al. [6] have reported that there is a significant correlation between tumor size and LNM.
There have been few reports on correlations between clinicopathologic factors and level VII LNM. In this study, we attempted to investigate the feasibility of level VII dissection without opening the sternum rather than the effects of level VII dissection on survival or recurrence in PTC. According to our study, the level VII LNM rate was significantly elevated in patients with lateral neck metastasis, or those with a tumor size >1.5 cm or lymphovascular invasion. Thus, level VII dissection should be considered in patients with lateral neck metestasis or those with a tumor size of >1.5 cm. If histopathological examination of surgical specimens reveals that there is lymphovascular invasion, special attention should be paid to the detection of level VII recurrence.
It is thought that there may be a higher rate of permanent hypoparathyroidism, unintentional permanent nerve injury, chyle leakage, pleural injury and vessel injury when level VII LN dissection is performed than for level VI LN dissection alone. But our study is similar other large data [17]. If closed attentional operation is performed, complication is due to level VII LN dissection is not higher rate than level VI LN dissection alone.
Further studies on the rates of mortality and recurrence are needed to confirm our results.
Figures and Tables
Fig. 1
Anatomical boundaries of nodal levels VI (central compartment group) and Vll (superior mediastinal group) (reprinted from Shah JP, Patel SG. Head and neck surgery and oncology. 3rd ed. London: Mosby; 2002. p.355, with permission of Elsevier.) [10].

Fig. 2
The surgical field following level Vll dissection. (A) The right innominate artery was dissected free from the level Vll lymph nodes. (B) The left innominate vein was dissected from the level Vll lymph nodes and the left common carotid artery was retracted laterally with a long-arm retractor.

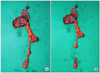
Fig. 3
(A) Right thyroid lobectomy, along with level Vl and Vll dissection was performed as en bloc dissection. (B) We separated level Vll lymph nodes from thyroid and level Vl lymph nodes after resection.
References
1. McConahey WM, Hay ID, Woolner LB, van Heerden JA, Taylor WF. Papillary thyroid cancer treated at the Mayo Clinic, 1946 through 1970: initial manifestations, pathologic findings, therapy, and outcome. Mayo Clin Proc. 1986. 61:978–996.
2. Rossi RL, Cady B, Silverman ML, Wool MS, Horner TA. Current results of conservative surgery for differentiated thyroid carcinoma. World J Surg. 1986. 10:612–622.
3. Hay ID, Bergstralh EJ, Goellner JR, Ebersold JR, Grant CS. Predicting outcome in papillary thyroid carcinoma: development of a reliable prognostic scoring system in a cohort of 1779 patients surgically treated at one institution during 1940 through 1989. Surgery. 1993. 114:1050–1057.
4. Sato N, Oyamatsu M, Koyama Y, Emura I, Tamiya Y, Hatakeyama K. Do the level of nodal disease according to the TNM classification and the number of involved cervical nodes reflect prognosis in patients with differentiated carcinoma of the thyroid gland? J Surg Oncol. 1998. 69:151–155.
5. Mazzaferri EL, Jhiang SM. Long-term impact of initial surgical and medical therapy on papillary and follicular thyroid cancer. Am J Med. 1994. 97:418–428.
6. Scheumann GF, Gimm O, Wegener G, Hundeshagen H, Dralle H. Prognostic significance and surgical management of locoregional lymph node metastases in papillary thyroid cancer. World J Surg. 1994. 18:559–567.
7. Hughes CJ, Shaha AR, Shah JP, Loree TR. Impact of lymph node metastasis in differentiated carcinoma of the thyroid: a matched-pair analysis. Head Neck. 1996. 18:127–132.
8. Lundgren CI, Hall P, Dickman PW, Zedenius J. Clinically significant prognostic factors for differentiated thyroid carcinoma: a population-based, nested case-control study. Cancer. 2006. 106:524–531.
9. Greene FL, Page DL, Fleming ID, Fritz AG, Balch CM, Haller DG, et al. AJCC cancer staging manual. 2002. 6th ed. New York: Springer-Verlag;77–87.
10. Shah JP, Patel SG. Head and neck surgery and oncology. 2002. 3rd ed. London: Mosby;355.
11. Grebe SK, Hay ID. Prognostic factors and management in thyroid cancer--consensus or controversy? West J Med. 1996. 165:156–157.
12. Clark OH. Predictors of thyroid tumor aggressiveness. West J Med. 1996. 165:131–138.
13. Robbins KT, Medina JE, Wolfe GT, Levine PA, Sessions RB, Pruet CW. Standardizing neck dissection terminology. Official report of the Academy's Committee for Head and Neck Surgery and Oncology. Arch Otolaryngol Head Neck Surg. 1991. 117:601–605.
14. Robbins KT, Clayman G, Levine PA, Medina J, Sessions R, Shaha A, et al. Neck dissection classification update: revisions proposed by the American Head and Neck Society and the American Academy of Otolaryngology-Head and Neck Surgery. Arch Otolaryngol Head Neck Surg. 2002. 128:751–758.
15. Goropoulos A, Karamoshos K, Christodoulou A, Ntitsias T, Paulou K, Samaras A, et al. Value of the cervical compartments in the surgical treatment of papillary thyroid carcinoma. World J Surg. 2004. 28:1275–1281.
16. Hay ID, Thompson GB, Grant CS, Bergstralh EJ, Dvorak CE, Gorman CA, et al. Papillary thyroid carcinoma managed at the Mayo Clinic during six decades (1940-1999): temporal trends in initial therapy and long-term outcome in 2444 consecutively treated patients. World J Surg. 2002. 26:879–885.
17. White ML, Gauger PG, Doherty GM. Central lymph node dissection in differentiated thyroid cancer. World J Surg. 2007. 31:895–904.




 Citation
Citation Print
Print





 XML Download
XML Download