Abstract
Purpose
The aim of this study was to evaluate the prognostic significance of the ratio between metastatic and examined lymph nodes (LNs) in patients with stage III rectal cancer.
Methods
A review was made of 175 (male, 98) patients with stage III rectal cancer of R0 resection. LN disease was stratified both by the American Joint Committee on Cancer/International Union Against Cancer nodal classification (pN) and by quartiles of the lymph node ratio (LNR). Disease-free survivals (DFS) were made using Kaplan-Meier curves and assessed by the log rank test and multivariate analysis was performed using the Cox proportional hazards model.
Results
Patients ranged in age from 29 to 83 (median, 60) years with median follow-up of 47 months (range, 13 to 181 months). months. There was a significant correlation between the number of metastatic LNs and the LNR (r = 0.8681, P < 0.0001). Cut-off points of LNR quartiles best to separate patients with regard to 5-year DFS were between quartile 2 and 3, and between 3 and 4 (LNR1, 2, and 3); the 5-year DFS according to such stratification was 89.6%, 55.8%, and 18.2% in LNR1, 2, and 3, respectively (P < 0.0001). Cox model identified the LNR as the most significant independent prognostic covariate; LNR2 showed 3.6 times (95% confidence interval [CI], 1.682 to 7.584; P = 0.0009) and LNR3, 18.7 times (95% CI, 6.872 to 50.664; P < 0.0001) more risky than LNR1.
En-bloc surgical resection based on the concept of total mesorectal excision (TME) remains the mainstay of curative treatment options for rectal carcinoma [1,2]. Identification of lymph node (LN) metastasis is one of the most important pathologic predictors associated with both local recurrence and disease-specific survival [3,4].
In the American Joint Committee on Cancer and the International Union Against Cancer (AJCC/UICC) tumor, node, metastasis (TNM) staging system, the classification of LN metastasis (pN) in patients with stage III colorectal cancer is established on the basis of the number of LN involved (pN1, metastatic node ≤ 3; pN2, metastatic node ≥ 4) [5]. This number-based LN classification, however, may have inherent limits. As the number of LNs examined increases, accuracy in staging and long-term survival is improving [6-8]. Many studies have been performed to determine the optimal number of LNs to be examined to stage nodal disease accurately [8-10], but results showed a high degree of variability, and no definite consensus on the number of LNs to be examined for accurate staging has yet been made. Paradoxically, moreover, the number of metastatic LN(s) may increase when more LNs are retrieved in stage III disease. To overcome these ambiguities associated with simple number-based LN classification, more recent evidences emphasize the importance of ratio-based LN staging as a predictor of survival and this metastatic LN ratio (LNR), which considers the number of both metastatic and retrieved LNs, has been suggested to be an important prognostic factor in colon and rectal carcinoma [11-13]. This nodal classification may obviate the risk of over-staging or under-staging incurred in the pN classification used in the TNM staging system and may provide more accurate prognostic information from LN involvement.
The aim of this study was to discover whether the ratio between metastatic and examined LNs can predict survival in patients with stage III rectal carcinoma.
From the database of patients who underwent surgical resection for colorectal cancer under the care of the Department of Surgery, Dong-A University Medical Center from 1996 through 2002, stage III rectal carcinomas, where a radical R0 resection was performed, were reviewed. All patients underwent surgery according to the principles of TME, as previously described [14]. Postoperative chemoradiation therapy (mean radiation dose of 50.4 Gy with concurrent chemotherapy using the Mayo Clinic regimen) for stage III rectal carcinoma were standard protocols for adjuvant treatment modality in our institution. To minimize bias associated with data analyses, patients who received neoadjuvant chemoradiation therapy or who received no adjuvant therapy were not considered in this study. Other exclusions included 3 patients with familial adenomatous polyposis, 4 with synchronous tumors, 8 in whom less than 7 LNs were examined (as recommended by 2002 edition of AJCC/UICC cancer staging system), and 21 patients with inadequate follow-up data. A total of 175 (male, 98) patients were eligible for this retrospective study.
LN disease was stratified by both AJCC/UICC nodal staging system (pN) and by quartiles of the LNR. The LNR was defined as the number of metastatic LNs divided by the number of retrieved LNs for each patient. We, herein, interpreted oncologic outcome in terms of disease-free survivals (DFS) rather than overall survivals (OS) in order to avoid inherent bias associated with different inhomogeneous treatment options of postoperative metastatic or recurrent diseases, including surgeries and diverse chemotherapeutic modalities. Five-year DFS were made using Kaplan-Meier curves and assessed by the log rank test. To compare the prognostic value of LNR with other factors, multivariate analysis was performed using the Cox proportional hazards model in forward stepwise regression.
For statistical analysis, data were entered into a spreadsheet program and subsequently imported into statistic programs (Prism ver. 4, GraphPad Software Inc., San Diego, CA, USA; SAS ver. 8.2, SAS Institute Inc., Cary, NC, USA). Correlation between the number of metastatic LNs and LNR was analyzed by the Pearson correlation coefficient. Survival curves were calculated using the Kaplan-Meier method and analyzed by the log-rank test. To assess the relative prognostic value of covariates associated with 5-year DFS, multivariate analyses were carried out using the Cox proportional hazard regression model. A P-value of less than 0.05 was considered statistically significant.
Patients ranged in age from 29 to 83 years (median, 60 years) with median follow-up period being 47 months (range, 33 to 181 months). A total of 3,118 LNs with a median nodal yield of 16 (range, 8 to 55) per specimen were retrieved and examined, of which 911 (median, 3; range, 1 to 30) LNs proved to be metastatic. The median of the LNR in the present study was 0.21 (mean, 0.30; range, 0.02 to 0.97). During the follow- up, 69 patients experienced disease relapse; 13 local recurrences, 50 distant metastases, and 6 both local recurrence and distant metastases. The mean LNRs in each mode of relapse were not different statistically (0.35 vs. 0.49 vs. 0.59; P = 0.151). Table 1 shows the correlation between the LNR and clinicopathologic characteristics; the LNR was significantly higher in cases with lymphovascular invasion (P = 0.0002) and was significantly correlated with grade of differentiation (P < 0.0001), depth of invasion (P = 0.0023), and pN classification (P < 0.0001). Furthermore, a significant correlation, as shown in Fig. 1, was found between the number of metastatic LN(s) and the LNR (Pearson correlation coefficient, 0.8681; 95% confidence interval [CI], 0.8262 to 0.9005; P < 0.0001) and a simple linear regression demonstrated that the LNR increases 0.0395 units as the number of metastatic LN increases by one (95% CI, 0.0362 to 0.0429; P < 0.0001).
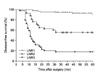
Overall 5-year DFS in this analysis was 60.2%. Patients were stratified into four groups based on quartiles of the LNR to explore if a specific cutoff could affect oncologic outcome. Based on Kaplan-Meier plots (Fig. 2), cutoff points of quartiles of the LNR considered the best indicator for separating patients with regards to 5-year DFS were between quartile 2 and 3 (95% CI, 0.0594 to 0.3398; P < 0.0001), and between 3 and 4 (95% CI, 0.1629 to 0.5059; P < 0.0001); they were restaged into 3 subgroups (LNR1, 2, and 3; Table 2). The 5-year DFS according to this LNR-based staging was 89.6%, 55.8%, and 18.2% for LNR1, LNR 2, and LNR3, respectively (P < 0.0001, Fig. 3). Table 3 demonstrates that LNR obviously discloses oncologically distinct subgroups within each AJCC/UICC pN1 and pN2 nodal category. In pN1 category, the 5-year DFS of LNR1 subgroup was significantly higher than that of LNR2 (84.4% vs. 45%; P < 0.0001), and the same in pN2 category (LNR1 vs. LNR2 vs. LNR3, 76.9% vs. 65.2% vs. 18.2%; P < 0.0001). Moreover, in each LNR category, DFS between pN1 and pN2 was not different statistically. Probability of stage migration in the AJCC/UICC nodal classification might be inferred from the finding that 5-year DFS of 45% for pN1 subgroup with LNR2 was less favorable than that of 76.9% for pN2 subgroup with LNR1, although statistically insignificant (P = 0.1094).
To determine independent prognostic covariates for 5-year DFS, a multivariate analysis using the Cox proportional hazard regression model was performed. Both pN and LNR categories were considered as a factor related to nodal status in this model. As shown in Table 4, LNR was the strongest prognostic covariate (χ2 = 33.2977, P < 0.0001), followed by pT stage (χ2 = 3.9933, P = 0.0457), and preoperative serum carcinoembryonic antigen level (χ2 = 3.9490, P = 0.0469). In addition, evaluation of 95% CI for the relative risk (hazard ratio) of relapse at each level of covariates also confirmed strong predictive ability of the LNR; LNR2 showed 3.6 times more risk of relapse than LNR1 (95% CI, 1.682-7.584) and LNR3, 18.7 times more risk than LNR1 (95% CI, 6.872-50.664). pN by the AJCC/UICC classification, however, was not found to be an independent prognostic predictor in this model.
Determination of regional LN status has long been considered to be one of the most important factors in predicting the likelihood of long-term survival in colon and rectal carcinoma. LN disease in the most recent AJCC/UICC TNM system revised in 2002 is categorized simply according to the number of metastatic LN(s) present [5]. This current number-based nodal staging category of the TNM system, however, can now be criticized for the fact that the number of metastatic LN(s) present may be influenced by the total number of LNs to be examined and thus, probability of stage migration cannot be ignored [6-10,15]. In an attempt to overcome these shortcomings, LNR, which defines the ratio of the number of metastatic-to-total number of LNs, has been proposed as a potentially more informative prognostic indicator for LN status. This ratio-based nodal staging has been studied extensively in gastric cancer. Compared to the number-based AJCC/UICC classification or Japanese classification of gastric carcinoma [16], ratio-based nodal staging has been suggested to be a highly reliable staging system with a strong ability to predict oncologic outcome [17-22]. Similar results have been reported in other solid tumors, as well [23-25]. A significance of the LNR relevant to oncologic prognosis in colon cancer has been presented recently [11-13]. Berger et al. [12] analyzed data from the Intergroup 0089 trial and concluded that LNR was an important prognostic factor for colon carcinoma and that LNR may decrease the potential for stage migration, which can be influenced by the number of dissected LNs. Our previous study also demonstrated that LNR was the strongest prognostic covariate in node-positive colon cancer [11]. Oncologic significance of LNR in rectal cancer might be somewhat ambiguous in interpretation because of diverse adjuvant modalities. To keep the homogeneity in study populations, the current study considered only those patients who received postoperative chemotherapy (upper rectal cancer) or chemoradiation therapy (mid or lower rectal cancer). Like in colon cancer, results clearly indicated that nodal staging according to the LNR had a significant oncologic relevance in stage III rectal cancer. Larger-scale studies also concluded that LNR was the most significant predictor of survival in patients with LN-positive rectal cancer, irrespective of adjuvant modalities [13,26,27].
Highly suggestive in this study are the findings in Table 3 that LNR obviously discloses oncologically distinct subgroups within each AJCC/UICC pN1 and pN2 nodal category. These results obviously show that the ratio-based nodal staging reflects the number of LNs examined and the quality of LN dissection. Considering the results of 5-year DFS for pN1 category with LNR2 subgroup are less favorable than those for pN2 with LNR1 subgroup (45% vs. 76.9%), it may strongly imply the probability of stage migration in number-based pN classification. The large-scale study of colon cancer by Berger et al. [12] also demonstrated a similar result; the 5-year OS for pN1 patients with an LNR of more than 40% is much worse (60%) than that for N2 patients with an LNR of less than 20% (73%). As also evidenced in gastric cancer, the ratio-based nodal staging decreased the incidence of stage migration significantly [18-20].
Although the LNR has been emphasized as a significant prognostic predictor, quantification should be followed for clinical application with validity. Contrary to the pN in the AJCC/UICC staging system where uniform parameters are adapted for stratification, no consistent categorical division for prognostic stratification has been established in the ratio-based nodal staging, yet. In literature, the methodological criteria to set cutoff levels were inconsistent with each other and different levels of cutoff for its staging have been used [19-22,24]. Statistically, stratification according to quartiles of ratio distribution seems to be sound and has been applied in diverse cancers [11,13,23]. To be of objective validity in this study, the author, at first, divided the ratio into 4 groups based on quartiles of the distribution and then, the ratio above which the 5-year DFS drastically decreased was established as a cutoff point based on Kaplan-Meier plots and log-rank test. Noticeably, the median LNR of 0.21 in this study with stage III rectal cancer compares similarly with that in other studies for colon or rectal cancers (0.16 to 0.24) [11-13,26]. Further larger-scale prospective investigations may be imperative to establish a specific valid cutoff point of the LNR for prognostic stratification in clinical application.
In this study, we compared the prognostic determinant of the number-based pN together with the ratio-based LNR. To compare the predictability of pN and LNR on survival, we applied the multivariate Cox stepwise proportional hazards model. To be more specific, we considered 3 cases of models (case A, case B, and case C). Case A included all covariates except LNR, case B all except pN, and finally case C included both LNR and pN as well as other covariates. Results are summarized in Table 5. We noted that the covariate pN was selected when LNR was not included. On the other hand, LNR, not pN, was selected when both were included in the final Cox regression and proved to be the most predictive covariate among all others. The similar method of multivariate analysis in recent studies with rectal cancer also showed that the covariate AJCC/UICC pN classification was not associated with prognosis in any cases, whereas the LNR was the most powerful factor associated with overall and DFS rates [13,26,27]. When impact of the LNR according to the number of LNs examined was analyzed, the LNR was an independent prognostic factor for overall survival even in the subgroup of patients in whom fewer than 12 LNs were examined [27]. Therefore, nodal classification according to the LNR is considered a better qualified independent prognostic determinant than the number-based pN and could replace total number of metastatic LN in future staging systems.
In conclusion, the current study suggests that the LNR displays a better stratification of the LN disease from an oncologic point of view and minimize the probability of stage migration compared with pN which may be influenced by the number of LNs examined. The ratio-based LN staging can be considered a simple and reliable system to assess oncologic prognosis of patients who underwent a potentially curative radical resection for LN-positive rectal cancer.
Figures and Tables
Fig. 1
The correlation between the metastatic lymph node ratio and number of lymph node metastases. The lymph node ratio is closely correlated with the number of lymph node metastases (Pearson correlation coefficient, 0.8681; P < 0.0001).
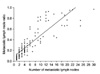
Fig. 2
Kaplan-Meier survival curves for 4 groups based on quartiles of the distribution of metastatic lymph node ratio. Differences in 5-year disease-free survivals between quartile (Q) 2 and 3 and between 3 and 4 were statistically significant (P < 0.0001, each).
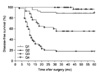
Fig. 3
Kaplan-Meier survival curves for the ratio-based staging. Five-year disease-free survival was 89.6%, 55.8%, and 18.2% for lymph node ratio (LNR)1, LNR2, and LNR3, respectively (P < 0.0001).
References
1. Heald RJ, Moran BJ, Ryall RD, Sexton R, MacFarlane JK. Rectal cancer: the Basingstoke experience of total mesorectal excision, 1978-1997. Arch Surg. 1998. 133:894–899.
2. Havenga K, Enker WE, Norstein J, Moriya Y, Heald RJ, van Houwelingen HC, et al. Improved survival and local control after total mesorectal excision or D3 lymphadenectomy in the treatment of primary rectal cancer: an international analysis of 1411 patients. Eur J Surg Oncol. 1999. 25:368–374.
3. Law WL, Chu KW. Anterior resection for rectal cancer with mesorectal excision: a prospective evaluation of 622 patients. Ann Surg. 2004. 240:260–268.
4. Kapiteijn E, Putter H, van de Velde CJ. Cooperative investigators of the Dutch ColoRectal Cancer Group. Impact of the introduction and training of total mesorectal excision on recurrence and survival in rectal cancer in The Netherlands. Br J Surg. 2002. 89:1142–1149.
5. Greene FL, Page DL, Fleming ID, Fritz AG, Balch CM, Haller DG, et al. AJCC cancer staging manual. 2002. 6th ed. New York: Springer-Verlag.
6. Tepper JE, O'Connell MJ, Niedzwiecki D, Hollis D, Compton C, Benson AB 3rd, et al. Impact of number of nodes retrieved on outcome in patients with rectal cancer. J Clin Oncol. 2001. 19:157–163.
7. Le Voyer TE, Sigurdson ER, Hanlon AL, Mayer RJ, Macdonald JS, Catalano PJ, et al. Colon cancer survival is associated with increasing number of lymph nodes analyzed: a secondary survey of intergroup trial INT-0089. J Clin Oncol. 2003. 21:2912–2919.
8. Joseph NE, Sigurdson ER, Hanlon AL, Wang H, Mayer RJ, MacDonald JS, et al. Accuracy of determining nodal negativity in colorectal cancer on the basis of the number of nodes retrieved on resection. Ann Surg Oncol. 2003. 10:213–218.
9. Goldstein NS, Sanford W, Coffey M, Layfield LJ. Lymph node recovery from colorectal resection specimens removed for adenocarcinoma. Trends over time and a recommendation for a minimum number of lymph nodes to be recovered. Am J Clin Pathol. 1996. 106:209–216.
10. Wong JH, Severino R, Honnebier MB, Tom P, Namiki TS. Number of nodes examined and staging accuracy in colorectal carcinoma. J Clin Oncol. 1999. 17:2896–2900.
11. Lee HY, Choi HJ, Park KJ, Shin JS, Kwon HC, Roh MS, et al. Prognostic significance of metastatic lymph node ratio in node-positive colon carcinoma. Ann Surg Oncol. 2007. 14:1712–1717.
12. Berger AC, Sigurdson ER, LeVoyer T, Hanlon A, Mayer RJ, Macdonald JS, et al. Colon cancer survival is associated with decreasing ratio of metastatic to examined lymph nodes. J Clin Oncol. 2005. 23:8706–8712.
13. Peng J, Xu Y, Guan Z, Zhu J, Wang M, Cai G, et al. Prognostic significance of the metastatic lymph node ratio in node-positive rectal cancer. Ann Surg Oncol. 2008. 15:3118–3123.
14. Heald RJ, Husband EM, Ryall RD. The mesorectum in rectal cancer surgery--the clue to pelvic recurrence? Br J Surg. 1982. 69:613–616.
15. Swanson RS, Compton CC, Stewart AK, Bland KI. The prognosis of T3N0 colon cancer is dependent on the number of lymph nodes examined. Ann Surg Oncol. 2003. 10:65–71.
16. Japanese Gastric Cancer Association. Japanese classification of gastric carcinoma. 2nd English ed. Gastric Cancer. 1998. 1:10–24.
17. Saito H, Fukumoto Y, Osaki T, Yamada Y, Fukuda K, Tatebe S, et al. Prognostic significance of the ratio between metastatic and dissected lymph nodes (n ratio) in patients with advanced gastric cancer. J Surg Oncol. 2008. 97:132–135.
18. Persiani R, Rausei S, Biondi A, Boccia S, Cananzi F, D'Ugo D. Ratio of metastatic lymph nodes: impact on staging and survival of gastric cancer. Eur J Surg Oncol. 2008. 34:519–524.
19. Kodera Y, Yamamura Y, Shimizu Y, Torii A, Hirai T, Yasui K, et al. Lymph node status assessment for gastric carcinoma: is the number of metastatic lymph nodes really practical as a parameter for N categories in the TNM Classification? Tumor Node Metastasis. J Surg Oncol. 1998. 69:15–20.
20. Inoue K, Nakane Y, Iiyama H, Sato M, Kanbara T, Nakai K, et al. The superiority of ratio-based lymph node staging in gastric carcinoma. Ann Surg Oncol. 2002. 9:27–34.
21. Nitti D, Marchet A, Olivieri M, Ambrosi A, Mencarelli R, Belluco C, et al. Ratio between metastatic and examined lymph nodes is an independent prognostic factor after D2 resection for gastric cancer: analysis of a large European monoinstitutional experience. Ann Surg Oncol. 2003. 10:1077–1085.
22. Bando E, Yonemura Y, Taniguchi K, Fushida S, Fujimura T, Miwa K. Outcome of ratio of lymph node metastasis in gastric carcinoma. Ann Surg Oncol. 2002. 9:775–784.
23. Megale Costa LJ, Soares HP, Gaspar HA, Trujillo LG, Santi PX, Pereira RS, et al. Ratio between positive lymph nodes and total dissected axillaries lymph nodes as an independent prognostic factor for disease-free survival in patients with breast cancer. Am J Clin Oncol. 2004. 27:304–306.
24. Berger AC, Watson JC, Ross EA, Hoffman JP. The metastatic/examined lymph node ratio is an important prognostic factor after pancreaticoduodenectomy for pancreatic adenocarcinoma. Am Surg. 2004. 70:235–240.
25. Herr HW. Superiority of ratio based lymph node staging for bladder cancer. J Urol. 2003. 169:943–945.
26. Kim YS, Kim JH, Yoon SM, Choi EK, Ahn SD, Lee SW, et al. Lymph node ratio as a prognostic factor in patients with stage III rectal cancer treated with total mesorectal excision followed by chemoradiotherapy. Int J Radiat Oncol Biol Phys. 2009. 74:796–802.
27. Peschaud F, Benoist S, Julié C, Beauchet A, Penna C, Rougier P, et al. The ratio of metastatic to examined lymph nodes is a powerful independent prognostic factor in rectal cancer. Ann Surg. 2008. 248:1067–1073.




 Citation
Citation Print
Print







 XML Download
XML Download