Abstract
Purpose
The incidence of papillary thyroid carcinoma (PTC) is increasing worldwide. Positive associations between indices of body size and thyroid cancer have been reported. However, the relationships to cancer severities and/or behaviors are uncertain.
Methods
We performed a retrospective analysis of the data of patients who underwent total thyroidectomy due to PTC. The epidemiologic factor and pathologic report after operation were determined based on chart review. The relationships between indices of body size and these parameters were assessed.
Results
Positive association between body mass index and T stage was found, but it was not statically significant. In neck lymph node metastasis, the group with metastasis had a tendency for larger mean height and weight, but significant difference was found only in height. However, in the multivariate analysis, the age and size of nodules were only identified as independent risk factors of neck lymph node metastasis (P = 0.000 and 0.019).
The incidence of papillary thyroid carcinoma (PTC), which is the most common histologic type of thyroid malignancy, is increasing worldwide [1]. High cure rates are achieved after initial treatment of patients who develop PTC. However, some patients are at a high risk of recurrence and even of death. Many publications have been devoted to finding prognostic factors for PTC, focusing on epidemiological, biological, clinical and pathological data [2-5].
In recent years, positive associations between height, weight and body mass index (BMI) and PTC have been reported [6-13]. The World Cancer Research Fund (WCRF) report concludes to a potential association between thyroid cancer and body size, possibly through changes in iodine requirement [14].
Most of these studies have looked into the etiology of thyroid cancer by comparing with healthy controls, however, it is unclear whether prognostic role of the body size in the severity and recurrence of PTC. Recently, Paes et al. [15] suggested that obesity may be correlated with a less aggressive tumor invasion, however it was not significant. Thus, more studies on effects of obesity for the thyroid cancer are needed.
In this study, we aimed to examine the association of indices of body size with aggressiveness and recurrence of PTC. So, we performed a retrospective investigation of the body size and cancer characteristics of patients who underwent total thyroidectomy PTC in our hospital.
We reviewed the charts of the persons who underwent a health examination from January 2007 to December 2009 in Health Examination Center of Gyeongsang National University. Among these, the patients who underwent total thyroidectomy for PTC were selected for the study. In each operation, when lymph node metastasis was suspected from the preoperative or intraoperative findings, central neck and/or lateral neck lymph node dissection were performed.
The epidemiologic factor and pathologic report after operation were determined based on chart review. Tumor-node-metastasis stage was based on the American Joint Committee on Cancer cancer staging manual seventh edition [16]. For each patients, the height and weight reported in the anesthesia summary was used to calculate the BMI according to its determined formula (i.e., BMI = weight [kg] / height [m2]).
All data are expressed as mean (± standard deviation). The SPSS (SPSS Inc., Chicago, IL, USA) was used for statistical analysis, and the one way analysis of variance test and chi-square test were used to compare the indices of body size and other parameters between T and N stage sub-groups.
Multivariate analysis was performed with logic regression analysis to identify the independent predictors of lymph node metastasis. P < 0.05 was considered statistically significant.
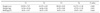
A total of 315 PTC patients (47 men and 268 women) were studied. The mean age was 51.09 years (range, 12 to 88 years). The mean BMI was 24.51 ± 3.20 kg/m2 and 133 patients (42.2%) had a BMI same or higher than 25 kg/m2. One hundred seventh-nine patients (56.8%) had nodules which were extrathyroidal extension, and 121 patients had regional lymph node metastasis (Table 1).
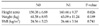
The correlation between the body size and T stage is shown in Table 2. Although positive association between BMI and T stage was found, it was not statically significant. The mean age of T1 and T2 (49.4 ± 12.37 years old) was significantly lower than that of T3 and T4 (52.34 ± 13.46 years old, P = 0.046).
A total of 124 patients had neck lymph node metastasis: 87 patients had only central neck lymph node metastasis, 7 patients had only lateral neck lymph node metastasis and 26 patients had both central and lateral neck lymph node metastasis. The higher rates of lymph node metastasis were seen in men when compared to women (55.3% vs. 35.4%, P = 0.014). And, the patients with lymph node metastasis were younger than patients of non-metastasis (48.93 years old vs. 52.44 years old, P = 0.020).
In the patients who were founded to have neck lymph node metastasis, the mean height and weight were larger than the others, but significant difference were founded only on height (Table 3). A multivariate analysis was conducted to find factors affecting the metastasis of neck lymph nodes, and age and size of nodules were only identified as independent risk factors (P = 0.000 and 0.019).
Recently many studies on the correlations between thyroid cancer and height, weight, and BMI have been published [6,11,17,18]. However, great heterogeneity exists among studies as to the actual association between body size and thyroid malignancy. The WCRF report concludes to a potential association between thyroid cancer and body size, possibly through changes in iodine requirement [14]. Renehan et al. [8] conducted a meta-analysis of five prospective studies on thyroid cancer and BMI, and reported that the risk of thyroid cancer for each increase of 5 in BMI among men and women were 1.52 and 1.14, respectively. According to a study by Sung et al. [18] on the development of various cancers by height, the greater the height, the higher the frequency of thyroid cancer became for both men and women.
Studies have been carried out on BMI and cancer risk, but the relationship between obesity and thyroid cancer stage or behavior remains unclear. Recently, Paes et al. [15] reported that a higher BMI was found not be associated with more aggressive tumor features or a greater likelihood of recurrence or persistence. Rather, they suggested that obesity may be correlated with a less aggressive tumor invasion, though it was not significant.
This study also found no statically significant difference between indices of body size and T and N stage. In neck lymph node metastasis, the group of positive metastasis had taller mean height, but there was no significant difference in multivariate analysis. Because the younger patients had an increased tendency to be taller than older patients, and the patients of positive lymph node metastasis were younger than the others.
Since this study was a retrospective study, it was limited in that various biases could not be excluded. This study was also limited in that it could not represent the patients who underwent lobectomy of the thyroid (small size and solitary cancer) since the subjects were only selected from patients who underwent total thyroidectomy among the PTC patients. Moreover, because this study had short period of follow-up and was carried out with a relatively small group of patients, the prognosis was not directly compared.
In this study, our findings suggest that PTC severity and recurrence are not associated with indices of body size. A further confirmatory study should be conducted.
Figures and Tables
References
1. Davies L, Welch HG. Increasing incidence of thyroid cancer in the United States, 1973-2002. JAMA. 2006. 295:2164–2167.
2. Mazzaferri EL. Management of a solitary thyroid nodule. N Engl J Med. 1993. 328:553–559.
3. Hay ID, Bergstralh EJ, Goellner JR, Ebersold JR, Grant CS. Predicting outcome in papillary thyroid carcinoma: development of a reliable prognostic scoring system in a cohort of 1779 patients surgically treated at one institution during 1940 through 1989. Surgery. 1993. 114:1050–1057.
4. Cady B. Papillary carcinoma of the thyroid gland: treatment based on risk group definition. Surg Oncol Clin N Am. 1998. 7:633–644.
5. Loh KC, Greenspan FS, Gee L, Miller TR, Yeo PP. Pathological tumor-node-metastasis (pTNM) staging for papillary and follicular thyroid carcinomas: a retrospective analysis of 700 patients. J Clin Endocrinol Metab. 1997. 82:3553–3562.
6. Engeland A, Tretli S, Akslen LA, Bjørge T. Body size and thyroid cancer in two million Norwegian men and women. Br J Cancer. 2006. 95:366–370.
7. Goodman MT, Kolonel LN, Wilkens LR. The association of body size, reproductive factors and thyroid cancer. Br J Cancer. 1992. 66:1180–1184.
8. Renehan AG, Tyson M, Egger M, Heller RF, Zwahlen M. Body-mass index and incidence of cancer: a systematic review and meta-analysis of prospective observational studies. Lancet. 2008. 371:569–578.
9. Iribarren C, Haselkorn T, Tekawa IS, Friedman GD. Cohort study of thyroid cancer in a San Francisco Bay area population. Int J Cancer. 2001. 93:745–750.
10. Mack WJ, Preston-Martin S, Bernstein L, Qian D. Lifestyle and other risk factors for thyroid cancer in Los Angeles County females. Ann Epidemiol. 2002. 12:395–401.
11. Dal Maso L, La Vecchia C, Franceschi S, Preston-Martin S, Ron E, Levi F, et al. A pooled analysis of thyroid cancer studies. V. Anthropometric factors. Cancer Causes Control. 2000. 11:137–144.
12. Ron E, Kleinerman RA, Boice JD Jr, LiVolsi VA, Flannery JT, Fraumeni JF Jr. A population-based case-control study of thyroid cancer. J Natl Cancer Inst. 1987. 79:1–12.
13. Flegal KM, Carroll MD, Ogden CL, Curtin LR. Prevalence and trends in obesity among US adults, 1999-2008. JAMA. 2010. 303:235–241.
14. World Cancer Research Fund/American Institute for Cancer Research. Food, nutrition, physical activity, and the prevention of cancer: a global perspective. 2007. Washigton, DC: Americal Institute for Cancer Research.
15. Paes JE, Hua K, Nagy R, Kloos RT, Jarjoura D, Ringel MD. The relationship between body mass index and thyroid cancer pathology features and outcomes: a clinicopathological cohort study. J Clin Endocrinol Metab. 2010. 95:4244–4250.
16. Edge SB, Byrd DR, Compton CC, Frits AG, Greene FL, Trotti A. AJCC cancer staging manual. 2010. 7th ed. New York: Springer.
17. Leitzmann MF, Brenner A, Moore SC, Koebnick C, Park Y, Hollenbeck A, et al. Prospective study of body mass index, physical activity and thyroid cancer. Int J Cancer. 2010. 126:2947–2956.
18. Sung J, Song YM, Lawlor DA, Smith GD, Ebrahim S. Height and site-specific cancer risk: a cohort study of a Korean adult population. Am J Epidemiol. 2009. 170:53–64.




 Citation
Citation Print
Print



 XML Download
XML Download