Abstract
Objectives
The present meta-analysis aimed to assess the effect of the herbal medicine on the vaginal epithelial cells (VECs) among the menopausal subjects.
Methods
The literature related to VECs exposed to various herbal medicines in menopausal women were searched on three databases, MEDLINE (1966–August 2017), Scopus (1990–August 2017) and Cochrane Library (Cochrane Central Register of Controlled Trials; 2014).
Results
Totally, the meta-analysis was conducted on 11 randomised controlled trials. Based on the findings, the standardized mean difference (SMD) of maturation value (MV) was observed to be elevated by 0.48% (95% interval confidence [CI], 0.108–0.871; P = 0.012), as well as the heterogeneity was high (I2 = 84%; P < 0.001). The MV revealed a significant increase in soy group (SMD, 0.358; 95% CI, 0.073–0.871; P = 0.014) compared to the control group.
Menopause is a natural biological transition in life experienced by all women as they age,12 which is caused by end of ovarian function resulting in permanent discontinuation of the menstrual cycle.34 Women live a third of their life in the period of menopause.5
Some of the respective consequences following the menopause characterized by estrogen deficiency are vaginal atrophy, bone loss, mood and flashes.6 The quality of life of the postmenopausal women is affected by Genitourinary syndrome 7 whose symptoms though are attenuated widely by hormone therapy. Reportedly, there are several complications following the hormone therapy, including high risk of breast cancer, endometrial cancers,8 breast tenderness and venous thromboembolism.9 Therefore, the herbal medicines nowadays have attracted further attentions as safe alternatives by many postmenopausal women.10 To the best of our knowledge, limited studies investigated the effect of herbal medicine on vaginal atrophy among menopausal women and there are some new published trials. Accordingly, it is essential to update the knowledge through the systematic review or meta-analysis in this regard.
The literature concerning the vaginal epithelial cells (VECs) exposed to various herbal medicines in menopausal women was searched on three databases of MEDLINE (1966–August 2017), Scopus (1990–August 2017) and Cochrane Library (Cochrane Central Register of Controlled Trials; 2014).
The keywords for searching were the relationship between menopause and primrose oil, St. John's wort, Hypericumperforatum, Black cohosh, Red clover, Piascledine, Avocado plus, Soy, kava, Cimicifuga racemosa rhizome, Licorice red, Trigonella foenum-graecum, Ginseng, fenugreek, Flaxseed, Dong quai, Vitex Agnus-Castus, Evening primrose oil, Yam, Salvia officinalis, alternative treatments, complementary treatments, Phytomedicine, herbal treatments or herbs.
Two reviewers independtly extracted the rerquired data among trials on the databases and the third reviwer was recruited to address the possible disagrements. The data included year of publication, first author, age of participants, rate of drop out, number of patients in the intervention and control groups. According to Physiotherrapy Eviedence Database (PEDro) scale, the two reviwers performed indepently the quality assessment of the trials.
Comprehensive meta-analysis software12 was used to determine the standardized mean difference (SMD) for each study. The high heterogeneity among trials made us to reporte the data on the basis of Random Effect Model (Dersimonian and Laird method).
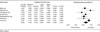
The selection process of randomized controlled trials (RCTs) for enrolling in the current meta-analysis is illustrated in Fig. 1, and the specifications of the studies have been summarized in Table 1. Overall, eleven studies1314151617181920212223 met our study inclusion criteria. The SMD of the of MV increased up to 0.48% (95% confidence interval [CI], 0.108–0.871; P = 0.012). The findings revealed high degree of heterogeneity (I2 = 84%; P < 0.001) (Fig. 2). Therefore, the sensitivity analysis was carried to explore the causes of heterogeneity in crossover trials. The individually exclusion of each study had no significant changes at the level of heterogeneity. No asymmetry was seen in the funnel plot of the trials assessing the effectiveness of herbal medicine on the of MV (Fig. 3). The absence of the publication bias was confirmed using the Egger's regression intercept test (P = 0.056) (Fig. 2). We also performed subgroup analysis for the women receiving soy. The of MV showed a significant increase by 0.358% (95% CI, 0.073–0.871; P = 0.014; I2 = 53%; P = 0.052) (Fig. 4).
This is the first meta-analysis to explore the herbal medicine effect on the VECs among menopausal women. According to our findings, the herbal medicine has had statistically significant effect on the vaginal atrophy.
The meta-analysis of several trials demonstrated that the SMD of the MV had significantly borderline increase in the soy group compared to the control group. However, heterogeneity was high. We performed the subgroup analysis in which the meta-analysis was limited to the trials evaluating the effectiveness of the soy on the VECs, which a significant increase was found in the effect size compared to previous meta-analyses. In addition, our meta-analysis had lower (I2 = 53%) homogeneity compared to the previous investigations (I2 = 81%).10
A systematic review assessed four trials on the effectiveness of administration of topical isoflavones on vaginal atrophy. The topical isoflavones had a beneficial effect on the vaginal atrophy. However, the authors concluded that there is a need to larger RCTs to confirm their results.24
In contrast to our meta-analysis that revealed a significant increase in the of MV, a systematic review and meta-analysis recently performed on the effectiveness of phytoestrogen on the of MV among menopausal women showed no significant improvement in phytoestrogen group compared to the control group 0.164% (CI, −0.419 to 0.746).25
Several limitations present in this meta-analysis included high heterogeneity, low number of trials, small sample size and methodological flaw, which are better to be addressed in the future studies. The high heterogeneity might be related to the variations and duration of treatment so that some trials did not report pre- and post-treatment means and standard deviations. In addition, no intention-to-treat has been reported in a larger portion of studies contained in the meta-analysis. The quality of trials can be improved due to further trials to follow the CONSORT guidelines.
According to the findings obtained from our meta-analysis, the use of herbal medicines in different studies showed statistically significant positive effects on the VECs. The subgroup analysis of the patients receiving soy indicated also significant effects on the VECs. However, high heterogeneity among the trials makes ambiguous the definitive conclusions on the beneficial effects of herbal on the VECs.
Figures and Tables
 | Fig. 1The process of selection of randomized controlled trials to include in the meta analysis. MV: maturation value. |
 | Fig. 2Effects of herbal medicine on vaginal epithelial cells (%). Horizontal line: 95% confidence interval (CI), █: point estimate, ♦: combined overall effect of treatment. |
References
1. Abdi F, Mobedi H, Roozbeh N. Hops for menopausal vasomotor symptoms: Mechanisms of action. J Menopausal Med. 2016; 22:62–64.

2. Ghazanfarpour M, Kaviani M, Abdolahian S, Bonakchi H, Najmabadi Khadijeh M, Naghavi M, et al. The relationship between women's attitude towards menopause and menopausal symptoms among postmenopausal women. Gynecol Endocrinol. 2015; 31:860–865.

3. Golshiri P, Akbari M, Abdollahzadeh MR. Age at natural menopause and related factors in Isfahan, Iran. J Menopausal Med. 2016; 22:87–93.

4. Lee HH, Kim TH, Park J, Lee A, Park Y, Byun DW, et al. Expression of ezrin in vagina cells of postmenopausal rats after dietary administration of omega-3 Fatty Acid formula. J Menopausal Med. 2014; 20:97–103.

5. Direkvand-Moghadam A, Delpisheh A, Montazeri A, Sayehmiri K. Quality of life among Iranian infertile women in postmenopausal period: A cross-sectional study. J Menopausal Med. 2016; 22:108–113.

6. Levis S, Strickman-Stein N, Doerge DR, Krischer J. Design and baseline characteristics of the soy phytoestrogens as replacement estrogen (SPARE) study--a clinical trial of the effects of soy isoflavones in menopausal women. Contemp Clin Trials. 2010; 31:293–302.
7. Kim HK, Kang SY, Chung YJ, Kim JH, Kim MR. The recent review of the genitourinary syndrome of menopause. J Menopausal Med. 2015; 21:65–71.

8. Kaari C, Haidar MA, Junior JM, Nunes MG, Quadros LG, Kemp C, et al. Randomized clinical trial comparing conjugated equine estrogens and isoflavones in postmenopausal women: a pilot study. Maturitas. 2006; 53:49–58.

9. Scarabin PY, Oger E, Plu-Bureau G. Differential association of oral and transdermal oestrogen-replacement therapy with venous thromboembolism risk. Lancet. 2003; 362:428–432.

10. Ghazanfarpour M, Sadeghi R, Roudsari RL. The application of soy isoflavones for subjective symptoms and objective signs of vaginal atrophy in menopause: A systematic review of randomised controlled trials. J Obstet Gynaecol. 2016; 36:160–171.

11. Moseley AM, Herbert RD, Sherrington C, Maher CG. Evidence for physiotherapy practice: a survey of the Physiotherapy Evidence Database (PEDro). Aust J Physiother. 2002; 48:43–49.

12. Borenstein M, Hedges LV, Higgins JPT, Rothstein HR. Comprehensive meta-analysis. Englewood, NJ: Biostat;2005.
13. Baird DD, Umbach DM, Lansdell L, Hughes CL, Setchell KD, Weinberg CR, et al. Dietary intervention study to assess estrogenicity of dietary soy among postmenopausal women. J Clin Endocrinol Metab. 1995; 80:1685–1690.

14. Murkies AL, Lombard C, Strauss BJ, Wilcox G, Burger HG, Morton MS. Dietary flour supplementation decreases post-menopausal hot flushes: effect of soy and wheat. Maturitas. 1995; 21:189–195.

15. Carmignani LO, Pedro AO, Costa-Paiva LH, Pinto-Neto AM. The effect of dietary soy supplementation compared to estrogen and placebo on menopausal symptoms: a randomized controlled trial. Maturitas. 2010; 67:262–269.

16. Chiechi LM, Putignano G, Guerra V, Schiavelli MP, Cisternino AM, Carriero C. The effect of a soy rich diet on the vaginal epithelium in postmenopause: a randomized double blind trial. Maturitas. 2003; 45:241–246.

17. Radhakrishnan G, Rashmi NA, Vaid NB. Evaluation of isoflavone rich soy protein supplementation for postmenopausal therapy. Pak J Nutr. 2009; 8:1009–1017.
18. Knight DC, Howes JB, Eden JA, Howes LG. Effects on menopausal symptoms and acceptability of isoflavone-containing soy powder dietary supplementation. Climacteric. 2001; 4:13–18.

19. Levis S, Strickman-Stein N, Ganjei-Azar P, Xu P, Doerge DR, Krischer J. Soy isoflavones in the prevention of menopausal bone loss and menopausal symptoms: a randomized, double-blind trial. Arch Intern Med. 2011; 171:1363–1369.
20. Colli MC, Bracht A, Soares AA, de Oliveira AL, Bôer CG, de Souza CG, et al. Evaluation of the efficacy of flaxseed meal and flaxseed extract in reducing menopausal symptoms. J Med Food. 2012; 15:840–845.

21. Knight DC, Howes JB, Eden JA. The effect of Promensil, an isoflavone extract, on menopausal symptoms. Climacteric. 1999; 2:79–84.

22. Manonai J, Chittacharoen A, Theppisai U, Theppisai H. Effect of Pueraria mirifica on vaginal health. Menopause. 2007; 14:919–924.

23. D'Anna R, Cannata ML, Atteritano M, Cancellieri F, Corrado F, Baviera G, et al. Effects of the phytoestrogen genistein on hot flushes, endometrium, and vaginal epithelium in postmenopausal women: a 1-year randomized, double-blind, placebo-controlled study. Menopause. 2007; 14:648–655.
24. Ghazanfarpour M, Latifnejad Roudsari R, Treglia G, Sadeghi R. Topical administration of isoflavones for treatment of vaginal symptoms in postmenopausal women: A systematic review of randomised controlled trials. J Obstet Gynaecol. 2015; 35:783–787.

25. Saghafi N, Ghazanfarpour M, Sadeghi R, Najarkolaei AH, Omid MG, Azad A, et al. Effects of phytoestrogens in alleviating the menopausal symptoms: A systematic review and meta-analysis. Iran J Pharm Res. 2017; 16:99–111.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download