Abstract
Objectives
To evaluate and compare the efficacy and safety of the combination of raloxifene and alendronate with those of monotherapies in elderly women with osteoporosis.
Methods
Sixty-two postmenopausal women (mean age 63.5 ± 0.5 years) attending gynecologic osteoporosis clinics with established osteoporosis were randomly allocated to one of four treatment groups and monitored for 3 years. All patients enrolled in this study, including those in the control group (n = 14), received 1.0 g elemental calcium and 400 units of vitamin D per day. The raloxifene group (n = 16) received raloxifene 60 mg (Evista®) per day; alendronate group (n = 17) received low-dose (5 mg) alendronate with calcitriol 0.5 µg (Maxmarvil®) per day; and the combination therapy group (n = 15) received both raloxifene 60 mg and low-dose (5 mg) alendronate with calcitriol 0.5 µg. Bone mineral density (BMD) was measured in the lumbar spine and hip before and after 3 years of treatment.
Results
In patients who received the combined therapy, BMD increased in the lumbar spine and the hip by 7.2% (P<0.001) and 4.8% (P<0.001) at 3 years. For patients in the alendronate group, the increases were 6.7% (P<0.001) and 3.1% (P<0.01) respectively, for the raloxifene group, the increases were 4.36% (P<0.001) and 1.9% (P<0.05) in the vertebrae and femora, respectively; however, the BMD of patients in the control group decreased by 1.81% (P<0.05) and 1.6% (P<0.05), respectively, after 3 years. Patients who received the combination therapy had significantly higher BMD in both the vertebrae femora (P<0.01) in comparison to that in those treated with raloxifene or alendronate individually.
The impact of osteoporosis is most pronounced in elderly women who have the highest risk of fracture.12
Several medications are effective in decreasing the incidence of osteoporotic fractures. Vertebral and nonvertebral fractures can be reduced by 30% to 65% by the administration of anticatabolic agents (e.g. raloxifene, alendronate, and risedronate).34
Although the relationship between bone mineral density (BMD) and fracture reduction is not linear,567 meta-analyses of multiple clinical trials of antiresorptive therapies have revealed that an increase in BMD correlated well with the reduction in the rate of vertebral and nonvertebral fractures.789
Furthermore, Hochberg et al.8 demonstrated that women taking the bisphosphonate alendronate and who had the greatest improvement in vertebral BMD also showed the greatest reduction in vertebral fractures.
Delmas et al.10 conducted a post hoc analysis of the fracture risk during the 4-year extension period concerning raloxifene. Treatment with 60 mg raloxifene per day, decreased the risk of one or more new vertebral fractures by 39% (relative risk, 0.64; 95% confidence interval, 0.53-0.76). The risk of nonvertebral fractures did not significantly decreased.4
The rationale for combining two antiresorptive agents with different mechanisms of action is to induce a greater increase in bone mass and, hopefully, a greater reduction in fractures than that observed with a single antiresorptive agent. A 2-year study by Bone et al.11 demonstrated that BMD was higher in younger women administered the combination therapy of estrogen and alendronate than it was in women taking receiving monotherapy.
In addition, the number of reported fractures in the combination therapy group was lower than that in the respective individual therapy groups.
However, none of these studies had adequate statistical power to establish a greater decrease in fracture risk than that reported for the monotherapy. Each antiresorptive therapy achieves its therapeutic effects through different modes of action. Bisphosphonates bind to hydroxyapatite and inhibit bone resorption by decreasing the number and activity of osteoclasts.12
Theoretically the combination of estrogen and bisphosphonate is more ideal for osteoporosis therapy, but hormone replacement therapy (HRT) is no longer recommended as the first-line therapy of old postmenopausal osteoporosis after the Women's Health Initiative (WHI) study.13
Although the mechanisms of action of selective estrogen receptor modulators (SERMs) are not yet fully understood, factors that contribute to the tissue specifications of SERMs include binding to estrogen receptor and isoforms, binding of the SERM-estrogen receptor complex to target genes, and modification of gene expression by cellular proteins.14
The tissue specifications of raloxifene have been documented in clinical trials. Increases in BMD and decreases in markers for bone turnover1516 and lipid metabolism1718 are examples of the estrogen-agonist effects of raloxifene. Compared with the stimulation observed after estrogen therapies, raloxifene did not increase endometrial thickthickness 1920 or breast density21 were observed with raloxifene, which demonstrated the estrogen-antagonist effects on these tissues.
Owing to these contrasting actions, the present study was performed to test the hypothesis that the addition of alendronate would have an independent, additive effect on the changes in BMD and bone turnover markers observed with raloxifene therapy when these therapies were administered in combination.
This 3-year prospective randomized study was carried out to determine whether the combination therapy of raloxifene and low dose alendronate was efficacious and safe, in comparison with monotherapies in elderly women with osteoporosis.
The present study was conducted at the Department of Obstetrics and Gynecology at Chosun University Hospital. Between January 2012 to June 2016, 62 postmenopausal female patients who were enrolled in a non-randomized retrospective study.
Ambulatory women aged up to 75 years, who had their last menstrual period at least 5 years prior to study entry, were eligible for the study. Women with femoral neck BMD greater than 2.0 standard deviations below peak bone mass for healthy premenopausal women were eligible, regardless of the presence of prevalent vertebral fractures. Exclusion criteria for this study included: current bone disorders other than postmenopausal osteoporosis, history of cancer in the last 5 years, active venous thromboembolic disease, and endocrine disorders requiring pharmacologic therapy, except type II diabetes.
Sixty-two postmenopausal women (mean age 63.5 ± 0.5 years) attending gynecologic osteoporosis clinics for the treatment of established osteoporosis were randomly allocated to one of four treatment groups and monitored for 3 years. All patients enrolled in this study including those in the control group (n = 14) received 1.0 g elemental calcium and 400 units of vitamin D per day. The raloxifene group (n = 16) received raloxifene 60 mg (Evista®; Eli Lilly Company, Indianapolis, IN, USA) per day; alendronate group (n = 17) received low dose alendronate 5 mg with the calcitriol 0.5 µg (Maxmarvil®; Yuyu Co., Seoul, Korea) per day; and the combination therapy group (n = 15) received both raloxifene 60 mg and alendronate 5 mg with the calcitriol 0.5 µg. BMD was measured in the lumbar spine and hip before and 3 years of treatment. Urine and serum samples were obtained at baseline and weeks 2 and 4 followed by every 3 months from month 3 through month 36 after treatments for analysis of biochemical markers.
The BMD was determined using a prodigy series X-ray tube housing assembly (LUNAR; GE Medical System, Madison, WI, USA) at the posterior-anterior lumbar spine (vertebrae L1 to L4) and hip (femoral neck). The results of absorptiometry were examined by a single observer blind to the treatment regimens. The primary end-point was the lumbar spine BMD. Femoral neck BMD was considered the secondary end-points.
Urine and serum samples were obtained at baseline and weeks 2 and 4 followed by every 3 months from month 3 through month 36 after treatments for analysis of biochemical markers. Thus, early morning second void urine during fasting was collected for determination of N-telopeptide of type I collagen (NTx) by duplicate enzyme-linked immunosorbent assays with the Osteomark kit (Ostex International, Seattle, WA, USA) as a marker representing bone resorption and was expressed as a ratio over urine creatinine (Cr) to avoid bias from hydration status. Serum osteocalcin (OC) was measured by duplicate radioimmunoassay method with the OSCAtest kit (Henn, Berlin, Germany) as a marker representing bone formation.
The primary end point was the percentage change in BMD at the lumbar spine and femoral neck. The results of baseline demographic characteristics and participant-related data in the combined raloxifene plus alendronate and raloxifene only and alendronate only groups are presented as mean ± standard error of the mean (SEM) and were analyzed using a t-test. The analyses of the changes in BMD and bone markers were conducted based on the intention-to treat principle. For treatment effects, two-way analyses of variance (ANOVA) were used to test for differences between both treatment groups. For time effects, one-way ANOVA for repeated measurement was used to examine the changes within both treatment groups independently. Post-hoc test was also performed for the comparison of both treatment groups at each time point.
The characteristics of the women enrolled in the study were as follows: mean age of 63.8 years; average time after final menstrual period 17.8 years; and mean body mass index, 24.7 kg/m2. There were no differences in baseline characteristics among the groups (Table 1). Of the 70 women enrolled, 62 (88.6%) completed the study, there were no differences among the groups in the overall discontinuation rate or in the reasons for discontinuation.
In patients who received the combined therapy, BMD increased in the lumbar spine and the hip by 7.2% (P<0.001) and 4.8% (P<0.001) at 3 years. For patients in the alendronate group, the increases were 6.7% (P<0.001) and 3.1% (P<0.01) respectively, for the raloxifene group, the increases were 4.36% (P<0.001) and 1.9% (P<0.05) in the vertebrae and femora, respectively; however, the BMD of patients in the control group decreased by 1.81% (P<0.05) and 1.6% (P<0.05), respectively, after 3 years. Patients who received the combination therapy had significantly higher BMD in both the vertebrae femora (P<0.01) in comparison to that in those treated with raloxifene or alendronate individually (Table 2).
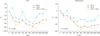
A significant decline in urine NTx/Cr was observed at week 4 in the raloxifene and the alendronate group, whereas in the raloxifene only group, a significant decline in urine NTx/Cr occurred at month 9. By the end of 36 months, urine NTx/Cr decreased by 47.7% in the raloxifene and the alendronate group (P=0.001) compared with a 22.1% increase in the raloxifene group). A significant decline in serum OC level occurred at month 3 in the raloxifene and the alendronate group, whereas a similar decline was observed at month 6 in the raloxifene group. By the end of 36 months, serum OC decreased by 48.6% in the raloxifene and the alendronate group (P<0.001) compared with a 1.6% increase in the raloxifene group) (Fig. 1).
There were no statistically significant differences among the groups with respect to the incidences of any of the adverse events that were associated with either raloxifene or alendronate therapy. More side effects occurred with longer duration of treatment. Pain in the bones and arthralgia increased after 3 years of treatment (Table 3).
Several treatment combinations have been evaluated in patients with postmenopausal osteoporosis. The BMD variation at the lumbar spine or proximal femur was chosen as the primary evaluation criterion.
Valuable additions to the treatment armamentarium for osteoporosis have been over a number of years. Randomized placebo-controlled trials in large populations have established that anticatabolic and anabolic agents reduce the risk of vertebral and nonvertebral osteoporotic fractures.
In the past, combination therapy consisted of the combination of two anticatabolic agents, such as HRT and a bisphosphonate. The combination of HRT and etidronate was shown to increase BMD compared to that reported with either agent alone.22 In two studies of postmenopausal women with low bone mass, the HRT and alendronate combination was associated with larger BMD increases than that observed with HRT alone.1123
However, HRT is no longer recommended for the first-line prevention and treatment of established postmenopausal osteoporosis after the WHI study.
It is well established that both raloxifene and alendronate can treat and prevent new vertebral fractures and increase BMD in postmenopausal women with osteoporosis. A randomized, double-blind 3-year study evaluated the effects of raloxifene and alendronate in 62 postmenopausal women with osteoporosis (femoral neck BMD T-score, < -2.5). Women (age ≤ 75 years and ≥ 2 years since their last menstrual period) received placebo, raloxifene 60 mg/day, alendronate 5 mg/day, or raloxifene 60 mg/day and alendronate 5 mg/day combined. At baseline and after 3 years, BMD was measured by dual x-ray absorptiometry.
Raloxifene and alendronate, alone or in combination, increased lumbar spine and femoral neck BMD in postmenopausal women with osteoporosis.
The present results for the combination therapy of raloxifene and alendronate were similar to those reported with other combinations of antiresorptive agents. After 3 years, the combination therapy of raloxifene and alendronate increased lumbar spine and femoral neck BMD by 7.2 and 4.8% from baseline, respectively. Combinations of HRT with etidronate22 and of conjugated equine estrogens with alendronate11 also increased lumbar spine and femoral neck BMD by approximately 6% and 4% from baseline, respectively. The addition of alendronate to existing HRT increased lumbar spine and femoral neck BMD by 3.6 and 1.7% from baseline, respectively.23
Increased BMD in lumbar spine and femoral neck of 3.8% and 2.6% from baseline, respectively,24 was observed in women treated with risedronate and HRT combination.
Some women did not respond to treatment and a loss of BMD was observed when a single antiresorptive agent was administered,2526 therefore, combinations of antiresorptive therapies may be an effective approach. Although there are possible BMD benefits of combination therapy, fracture efficacy data are lacking. Other factors that should be considered include the extraskeletal benefits associated with each therapy and the patient's concomitant illnesses or risk factors for other disorders.
Most importantly, the additional costs of with combination therapy may be prohibitive for some patients. The patient and physician should carefully weigh the risks and benefits of combination antiresorptive therapy before deciding on such a regimen.
Changes in bone markers are known to occur early in the treatment course.27 In our study, a significant decrease in urine NTx/Cr from baseline was observed at week 4 in the raloxifene and the alendronate group, whereas it occurred at month 9 in the raloxifene group. A significant decrease in serum OC level from baseline occurred at month 3 in the raloxifene and the alendronate group, whereas it was observed at month 6 in the raloxifene-only group. Our findings suggest that the use of the raloxifene and the alendronate group is effective in slowing the rate of bone turnover, and in our study its effect occurred early and persisted throughout the treatment period. Although raloxifene group also slowed the bone turnover rate, this occurred later with lesser magnitude in our study (Fig. 1).
In summary, raloxifene and alendronate individually, and in combination increased lumbar spine and femoral neck BMD and decreased all biochemical markers of bone turnover. The combination of alendronate and raloxifene produced a greater increase in femoral neck BMD compared to that with either agent alone. Although the increases in lumbar spine BMD and changes in bone turnover markers with alendronate individually and in combination therapy were similar to or greater than that observed with raloxifene alone, the effects of the combination of raloxifene and alendronate on BMD were independent and additive.
The effect of the combination of raloxifene and alendronate on fracture risk is unknown, and the long-term clinical safety of combination therapy on the risk of fracture remains to be determined.
Although this randomized study involved a relatively modest number of patients, strict drug compliance and a follow-up duration of 3 years enabled us to conclude that the combination therapy of raloxifene and alendronate was highly efficacious in improving spine and hip BMD, and preventing height loss in postmenopausal women with established osteoporosis. A long-term study with an adequate sample size is necessary to assess the impact of combination therapy, in comparison with that of individual therapies, on fracture rates.
Figures and Tables
Fig. 1
Percentage changes in urine N-terminal telopeptide/creatinine and serum osteocalcin at each time point. Filled diamonds, raloxifene (RLX) only group; filled squares alendronate (ALN) only group; filled triangles, RLX plus ALN group. P < 0.05 compared with baseline.
References
1. Cummings SR, Melton LJ. Epidemiology and outcomes of osteoporotic fractures. Lancet. 2002; 359:1761–1767.
2. NIH consensus declares osteoporosis a major public health issue. Osteoporos Rep. 2000; 16:1.
3. Jeong EH, Choi H, Jung HJ, Lee K, Jung HR, Kim MH, et al. The effects of three-year hormone therapy, raloxifene and alendronate on bone miner al density in postmenopausal women. J Korean Soc Menopause. 2009; 15:41–47.
4. Rossouw JE, Anderson GL, Prentice RL, LaCroix AZ, Kooperberg C, Stefanick ML, et al. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results From the Women's Health Initiative randomized controlled trial. JAMA. 2002; 288:321–333.
5. Faulkner KG. Bone matters: are density increases necessary to reduce fracture risk? J Bone Miner Res. 2000; 15:183–187.
6. Silva BC, Broy SB, Boutroy S, Schousboe JT, Shepherd JA, Leslie WD. Fracture Risk Prediction by Non-BMD DXA Measures: the 2015 ISCD Official Positions Part 2: Trabecular Bone Score. J Clin Densitom. 2015; 18:309–330.
7. Wasnich RD, Miller PD. Antifracture efficacy of antiresorptive agents are related to changes in bone density. J Clin Endocrinol Metab. 2000; 85:231–236.
8. Hochberg MC, Greenspan S, Wasnich RD, Miller P, Thompson DE, Ross PD. Changes in bone density and turnover explain the reductions in incidence of nonvertebral fractures that occur during treatment with antiresorptive agents. J Clin Endocrinol Metab. 2002; 87:1586–1592.
9. Cummings SR, Karpf DB, Harris F, Genant HK, Ensrud K, LaCroix AZ, et al. Improvement in spine bone density and reduction in risk of vertebral fractures during treatment with antiresorptive drugs. Am J Med. 2002; 112:281–289.
10. Delmas PD, Ensrud KE, Adachi JD, Harper KD, Sarkar S, Gennari C, et al. Efficacy of raloxifene on vertebral fracture risk reduction in postmenopausal women with osteoporosis: four-year results from a randomized clinical trial. J Clin Endocrinol Metab. 2002; 87:3609–3617.
11. Bone HG, Greenspan SL, McKeever C, Bell N, Davidson M, Downs RW, et al. Alendronate/Estrogen Study Group. Alendronate and estrogen effects in postmenopausal women with low bone mineral density. J Clin Endocrinol Metab. 2000; 85:720–726.
12. Fleisch H. Bisphosphonates: mechanisms of action. Endocr Rev. 1998; 19:80–100.
13. Chung SH, Kim TH, Lee HH, Park J, Sang JH. Hormone therapy in postmenopausal women according to the correlation of changes in bone mineral density. J Korean Soc Menopause. 2013; 19:101–105.
14. Mitlak BH, Cohen FJ. Selective estrogen receptor modulators: a look ahead. Drugs. 1999; 57:653–663.
15. Ettinger B, Black DM, Mitlak BH, Knickerbocker RK, Nickelsen T, Genant HK, et al. Multiple Outcomes of Raloxifene Evaluation (MORE) Investigators. Reduction of vertebral fracture risk in postmenopausal women with osteoporosis treated with raloxifene: results from a 3-year randomized clinical trial. JAMA. 1999; 282:637–645.
16. Hlaing TT, Compston JE. Biochemical markers of bone turnover - uses and limitations. Ann Clin Biochem. 2014; 51:189–202.
17. Walsh BW, Kuller LH, Wild RA, Paul S, Farmer M, Lawrence JB, et al. Effects of raloxifene on serum lipids and coagulation factors in healthy postmenopausal women. JAMA. 1998; 279:1445–1451.
18. Walsh BW, Paul S, Wild RA, Dean RA, Tracy RP, Cox DA, et al. The effects of hormone replacement therapy and raloxifene on C-reactive protein and homocysteine in healthy postmenopausal women: a randomized, controlled trial. J Clin Endocrinol Metab. 2000; 85:214–218.
19. Goldstein SR, Scheele WH, Rajagopalan SK, Wilkie JL, Walsh BW, Parsons AK. A 12-month comparative study of raloxifene, estrogen, and placebo on the postmenopausal endometrium. Obstet Gynecol. 2000; 95:95–103.
20. Cho YH, Um MJ, Kim SJ, Kim SA, Jung H. Raloxifene Administration in Women Treated with Long Term Gonadotropin-releasing Hormone Agonist for Severe Endometriosis: Effects on Bone Mineral Density. J Menopausal Med. 2016; 22:174–179.
21. Freedman M, San Martin J, O'Gorman J, Eckert S, Lippman ME, Lo SC, et al. Digitized mammography: a clinical trial of postmenopausal women randomly assigned to receive raloxifene, estrogen, or placebo. J Natl Cancer Inst. 2001; 93:51–56.
22. Wimalawansa SJ. A four-year randomized controlled trial of hormone replacement and bisphosphonate, alone or in combination, in women with postmenopausal osteoporosis. Am J Med. 1998; 104:219–226.
23. Lindsay R, Cosman F, Lobo RA, Walsh BW, Harris ST, Reagan JE, et al. Addition of alendronate to ongoing hormone replacement therapy in the treatment of osteoporosis: a randomized, controlled clinical trial. J Clin Endocrinol Metab. 1999; 84:3076–3081.
24. Harris ST, Eriksen EF, Davidson M, Ettinger MP, Moffett Jr AH Jr, Baylink DJ, et al. Effect of combined risedronate and hormone replacement therapies on bone mineral density in postmenopausal women. J Clin Endocrinol Metab. 2001; 86:1890–1897.
25. Greendale GA, Wells B, Marcus R, Barrett-Connor E. How many women lose bone mineral density while taking hormone replacement therapy? Results from the Postmenopausal Estrogen/Progestin Interventions Trial. Arch Intern Med. 2000; 160:3065–2071.
26. Choi HJ. New antiresorptive therapies for postmenopausal osteoporosis. J Menopausal Med. 2015; 21:1–11.
27. Greenspan SL, Resnick NM, Parker RA. Early changes in biochemical markers of bone turnover are associated with long-term changes in bone mineral density in elderly women on alendronate, hormone replacement therapy, or combination therapy: a three-year, double-blind, placebo-controlled, randomized clinical trial. J Clin Endocrinol Metab. 2005; 90:2762–2767.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download