Abstract
Objectives
We sought to describe the perioperative and postoperative adverse events associated with sacral colpopexy and evaluate the surgical outcome, complications, and benefits of laparoscopic sacral fixation for patients with pelvic prolapse.
Methods
Ninety-two women with uterine prolapse underwent sacral colpopexy between January 2011 and September 2016 at Chosun University Hospital. Patients' electronic medical records were investigated for demographic, intraoperative, and postoperative data. Strict definitions were used for all clinically relevant adverse events. Patients' outcomes were documented with 1 self-administered quality of life questionnaires: the Pelvic Floor Distress Inventory-20 focused on symptom distress. The primary analysis looking at perioperative and postoperative adverse events was descriptive and statistics were reported for all groups as n/N (%) with 95% confidence intervals for categorical variables and as mean ± standard deviation and mean (range) for all continuous variables.
Results
Their mean age was 69 ± 8.1 years, mean follow-up duration was 12 months, and mean operating time was 61 minutes. There were seven conversions due to anesthetic or surgical difficulties. Follow-up was performed using a telephone questionnaire and physical examination at 12 months. There were three cases of sacral pain with strong analgesics, one of vaginal erosion, two of transient urinary retentions, one of spondylitis, and two of mesh infection. Of the patients, 98.9% were satisfied with the surgical results, while none complained of sexual dysfunction or problems performing her usual activities.
Uterine prolapse is common in women of all ages. In particular, it affects 50% of parous women after menopause, with a lifetime prevalence risk of 30% to 50%.1 A large retrospective study of United States women found that, by 80 years of age, 11% of women would have undergone surgery for urogynecological complaints, and almost a one-third require repeat surgery.2
This high recurrence rate has driven attempts to gain a better understanding of prolapse and the development of more robust techniques. For women presenting with urogynecological problems, one size does not fit all. The surgeon's goal should be to offer a range of procedures and individualize surgery according to each patient's needs. Treatment should ultimately be determined by the women's wishes, with consideration of other relevant factors, including age, reproductive desire, medical co-morbidities, and previous surgery. It is often the doctor's preference, however, that influences treatment choice. Surgical methods include the vaginal and abdominal routes, with the latter being achievable using an open or laparoscopic approach. Treatment choice must consider functional and anatomical problems while minimizing morbidity and maximizing long-term efficacy.
In 1974, Scali et al.3 proposed creating suspension by placing prosthetic slings between the vagina and bladder anchored to the sacral promontory. Using this technique, Lefranc and Blondon4 reported a success rate of 97% at a mean 60 months of follow-up. Dorsey and colleagues56 were the first to describe laparoscopic sacral colpopexy involving dissection of the anterior wall of the vagina and the anterior portion of the rectum and the suturing of a mesh on the anterior aspect of the vagina and the levator ani muscles.
This minimally invasive surgery involves, just as in open surgery, the placement of two prosthetic meshes to restore and confer adequate reinforcement of the pelvic tissues.78
We aimed to report our experience with and 1-year results of the use of laparoscopic sacral fixation for the treatment of uterine prolapse.
In the current study, we retrospectively included patients who underwent laparoscopic sacral colpopexy between January 2011 and September 2016 at Chosun University Hospital. Data were extracted from the medical charts of the patients: age at the time of surgery, body mass index at the time of the preoperative appointment with the anesthetist, bone mineral density, menopausal status, initial stage of genital prolapse, operative and postoperative data, postoperative complications, and anatomical and functional results. Genital prolapse stage was classified according to the simplified International Continence Society Pelvic Organ Prolapse Quantification (POP-Q).9
The most severe stage of the three compartments defined the general stage of genital prolapse. A search for patent or masked stress urinary incontinence (SUI) was performed before and after prolapse reduction using a speculum and a cough test during the urodynamic evaluation. Laparoscopic sacral colpopexy was performed by a single trained surgeon in all cases. A non-absorbable Prolene soft mesh was sutured to the anterior or posterior wall of the vaginal stump depending on the patient's situation. A posterior mesh was placed only if there was a posterior compartment vault (elytrocele, rectocele, or enterocele).
Patients outcomes were documented with 1 self-administered quality of life questionnaires: the Pelvic Floor Distress Inventory (PFDI-20) focused on symptom distress. The satisfaction rate was evaluated using the following scale: worsened, stable or improved.10
The primary analysis looking at perioperative and postoperative adverse events was descriptive and statistics were reported for all groups as n/N (%) with 95% confidence intervals (CIs) for categorical variables and as mean ± standard deviation and mean (range) for all continuous variables.
The Mann-Whitney U test was used to compare continuous variables, while Fisher's exact test was used to compare categorical variables. The Statistical analyses were performed with the SPSS version 12.0 software package (SPSS Inc., Chicago, IL, USA).
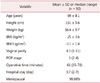
A total of 106 patients with a clinical diagnosis of symptomatic uterine prolapse with or without SUI underwent laparoscopic sacral colpopexy, but a complete medical chart and questionnaire for the analysis were available for only 92 of them. Table 1 described in the mean patient age was 69 ± 8.1 years.
Laparoscopic sacral colpopexy was performed in all patients; however, the data of 14 patients were not included in the final analysis because of conversion to open surgery owing to extensive peritoneal adherence in 4 patients and bleeding in 3 patients. In the other excluded cases, the patients did not attend the postoperative follow-up evaluation.
While blood loss was minimal and varied from 10 to 100 mL except in two patients. The bladder catheter was removed on day 2. The postoperative hospital stay was a mean 3.7 days (range, 2–7 days) following the French Health Policy (Table 1). All patients were discharged with laxatives prescribed until normal stools were achieved due to the high frequency of constipation in the immediate postoperative period.
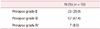
Among those with a history of previous surgical treatments, nine patients (9.8%) underwent anterior and posterior repair of the vagina to prevent progression of the uterine prolapse and 5 patients (5.4%) underwent a hysterectomy (Table 2). More than half (48 patients; 52.2%) had associated urinary incontinence that was verified in the urodynamic evaluation as sphincter insufficiency or bladder instability. All patients suffered from symptomatic prolapse of different degrees according to the Baden-Walker grading system (Table 3).
There were no adverse events about intraoperative injuries. However, 1.08% (95% CI, 0.01–0.5) of cases were complicated by transfusion and 2.17% (95% CI, 0.05–0.6) of cases were complicated by hematoma in the postoperative events.
The postoperative complications involved five patients with de novo postoperative urge incontinence treated medically, two cases of vaginal stump hematoma that was resolved after opening the vaginal stump, and one case of vaginal erosion of the mesh that was managed with local treatment and partial vaginal removal of the prosthesis (Table 4). These complications were followed up until their resolution. There were no other serious complications.
Mean follow-up was 12 months. The cure rate at the last follow-up physical examination was 98.9%, with the patients reporting their condition as worsened, stable, or improved in the telephone questionnaire survey (Table 5).
Of the three cases of sacral pain, two resolved spontaneously in 2 months, while the third persisted for >1 year. Concerning the functional results, two of the patients had persistent constipation during the first 6 months that resolved within this period, and no patient complained of dyspareunia after the surgery.
Traditional surgical approaches for correcting POP fall into two categories: transvaginal and transabdominal. Although generally more durable, transabdominal surgery is believed to be associated with greater morbidity rates than transvaginal surgery. Laparoscopy has the potential to combine the advantages of transabdominal repair with the low morbidity of transvaginal surgery. Transabdominal sacral colposuspension is considered by many as an excellent option to repair genital prolapse.1112 Several researchers have reported on this technique, including Snyder and Krantz13, Fox and Stanton14, who reported success rates of 93% to 100%.1314
The reported success of the open standardized technique prompted us to investigate the same using a laparoscopic approach. Here we report the placement of a mesh on the anterior or posterior wall of the vaginal stump after the resection of uterine prolapse. Our results have superior to those of open surgery in terms of side effects and patient satisfaction, with no reported cases of dyspareunia, making it an excellent option for young sexually active patients with pelvic prolapse; however, it should be considered that our follow-up period was short.15
Most of the patients in this study had an obstetric or gynecological history (9.8% had already undergone anterior and posterior repair of the vagina to prevent progression of genitourinary prolapse, while 5.4% had undergone a hysterectomy), which combined with their hormonal status (mean age, 69 years), further supports the use of prosthetic materials in the treatment of pelvic prolapse.16 The use of an artificial mesh theoretically carries a higher risk of tissue erosion and wound infection.17 Although these factors together represented < 1.1% of cases in this series.
Use of the laparoscopic approach enables complete anatomical repositioning of the pelvic organs that will influence their various functions and prevent new prolapse as confirmed by our 0% relapse rate the 1-year follow-up period. These good long-term results are comparable to those of Deval and Ocelli, who reported success rates of 91% and 98% in their series performed using an open approach.18 By contrast, patients with concomitant SUI, as reported in the literature, benefit from surgical procedures that simultaneously correct severe POP and SUI.12
On the contrary, postoperative urinary retention or dysuria could be caused by a hypocontractile bladder due to sympathetic stimulation resulting from surgical trauma, local irritation, or the presence of an anourethral reflex.19 Since these complications were rather infrequent in our series and all of the above points are speculative, this issue remains to be further investigated in electrophysiology studies.
The final group of complications involves relapse of prolapse, which could be due to surgical error; inadequate fibrosis inherent to the laparoscopic approach that may diminish the surgically obtained elevation; or dehiscence of the supporting fibrous bands from the paravaginal tissue, presumably precipitated by the early return to normal activity intrinsic to this technique.20
Our results without recurrence (0%) comparable to those reported by Deval could have resulted from meticulous mesh suturing and total hysterectomy before sacral colpopexy, which directly impacts lower rectocele relapse. Total hysterectomy in particular can reduce the downward gravity of the uterus, so its use before sacral colpopexy can prevent recurrent prolapse. Our results also reflect the important benefits of the laparoscopic approach, including excellent vision and the use of small instruments resulting in minimal dissection, tissue damage, and scarring. These factors will reduce postoperative pain and expedite postoperative recovery. However, further follow-up of our patients must be performed and a prospective comparative study must be conducted to confirm our findings.
Sacral colpopexy has been classified as a slightly difficult (degree, 3/5) laparoscopic urologic procedure,21 and it does not present a steep learning curve in surgeons who already practice laparoscopy except for the anatomical references and dissection, that can be easily learned.
Surgical correction of pelvic prolapse using laparoscopic sacral colpopexy with non-absorbable Prolene soft mesh to reposition these organs is a feasible alternative to open procedures, which ensures good anatomical repositioning of the pelvic organs within the pelvis and an expected return to physiological functionality. It is a highly effective procedure with excellent medium-term results and complication rates. Laparoscopic sacral colpopexy after total hysterectomy for uterine prolapse features better results than open surgery with the added benefit of being a minimally invasive approach.
Figures and Tables
References
1. Subak LL, Waetjen LE, van den Eeden S, Thom DH, Vittinghoff E, Brown JS. Cost of pelvic organ prolapse surgery in the United States. Obstet Gynecol. 2001; 98:646–651.
2. Olsen AL, Smith VJ, Bergstrom JO, Colling JC, Clark AL. Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol. 1997; 89:501–506.
3. Scali P, Blondon J, Bethoux A, Gerard M. Operations of support-suspension by upper route in the treatment of vaginal prolapse. J Gynecol Obstet Biol Reprod (Paris). 1974; 3:365–378.
4. Lefranc JP, Blondon J. Surgery of genital prolapse using the abdominal approach. Experience of the surgery and gynecology department at the Salpetriere Hospital. J Chir (Paris). 1983; 120:431–436.
5. Dorsey JH, Peagues RF. Laparoscopic reconstructive procedures. Obstet Gynecol Forum. 1993; 4:2–6.
6. Dorsey JH, Cundiff G. Laparoscopic procedures for incontinence and prolapse. Curr Opin Obstet Gynecol. 1994; 6:223–230.
7. Cosson M, Bogaert E, Narducci F, Querleu D, Crépin G. Laparoscopic sacral colpopexy: short-term results and complications in 83 patients. J Gynecol Obstet Biol Reprod (Paris). 2000; 29:746–750.
8. Fedele L, Garsia S, Bianchi S, Albiero A, Dorta M. A new laparoscopic procedure for the correction of vaginal vault prolapse. J Urol. 1998; 159:1179–1182.
9. Bump RC, Mattiasson A, Bo K, Brubaker LP, DeLancey JO, Klarskov P, et al. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol. 1996; 175:10–17.
10. Barber MD, Kuchibhatla MN, Pieper CF, Bump RC. Psychometric evaluation of 2 comprehensive condition-specific quality of life instruments for women with pelvic floor disorders. Am J Obstet Gynecol. 2001; 185:1388–1395.
11. Moore RD, Miklos JR. Colpocleisis and tension-free vaginal tape sling for severe uterine and vaginal prolapse and stress urinary incontinence under local anesthesia. J Am Assoc Gynecol Laparosc. 2003; 10:276–280.
12. Culligan PJ, Murphy M, Blackwell L, Hammons G, Graham C, Heit MH. Long-term success of abdominal sacral colpopexy using synthetic mesh. Am J Obstet Gynecol. 2002; 187:1473–1480.
13. Snyder TE, Krantz KE. Abdominal-retroperitoneal sacral colpopexy for the correction of vaginal prolapse. Obstet Gynecol. 1991; 77:944–949.
14. Fox SD, Stanton SL. Vault prolapse and rectocele: assessment of repair using sacrocolpopexy with mesh interposition. BJOG. 2000; 107:1371–1375.
15. Roovers JP, van der Vaart CH, van der Bom JG, van Leeuwen JH, Scholten PC, Heintz AP. A randomised controlled trial comparing abdominal and vaginal prolapse surgery: effects on urogenital function. BJOG. 2004; 111:50–56.
16. Shah DK, Paul EM, Rastinehad AR, Eisenberg ER, Badlani GH. Short-term outcome analysis of total pelvic reconstruction with mesh: the vaginal approach. J Urol. 2004; 171:261–263.
17. Cosson M, Debodinance P, Boukerrou M, Chauvet MP, Lobry P, Crépin G, et al. Mechanical properties of synthetic implants used in the repair of prolapse and urinary incontinence in women: which is the ideal material? Int Urogynecol J Pelvic Floor Dysfunct. 2003; 14:169–178.
18. Deval B, Fauconnier A, Repiquet D, Liou Y, Montuclard B, Fritel X, et al. Surgical treatment of genitourinary prolapse by the abdominal approach. Apropos of a series of 232 cases. Ann Chir. 1997; 51:256–265.
19. Ben Amna M, Grise P, Michot F, Sibert L. Impact of rectal prolapse and rectocele on TVT results. Prog Urol. 2003; 13:453–458.
20. el-Toukhy TA, Davies AE. The efficacy of laparoscopic mesh colposuspension: results of a prospective controlled study. BJU Int. 2001; 88:361–366.
21. Guillonneau B, Abbou CC, Doublet JD, Gaston R, Janetschek G, Mandressi A, et al. Proposal for a “ European Scoring System for Laparoscopic Operations in Urology”. Eur Urol. 2001; 40:2–6.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download