Abstract
Granular cell tumor (GCT) is a rare soft tissue tumor that derived from Schwann cells. Most are benign, less than 2% are malignant and, in the malignant cases, the prognosis of survival is poor. Most of these tumors are less than 3 cm in size, and they are more common in black women. The disease usually occurs in the 40s to the 60s and occurs after menopause, but there are few cases reported in adolescence. A 45-year-old woman visited the outpatient clinic with a solid mass that developed 2 years ago and present to date on the left side of the clitoris. After complete resection, pathologic examination proved to be a granular cell. The patient has been living without recurrence for one year. We report the first case of the GCT of the clitoris in postmenopausal woman in Korea with a brief review of the literature.
Granular cell tumors (GCTs) are the first tumors reported by Abrikossoff1 in 1926, with 7% of women developing GCTs in the clitoris, cervix, ovaries, and vagina.23 Most reports are cases, so the exact shape of the tumor is unknown. It occurs mainly in the dermis and subcutaneous tissue, occurrence in the muscle layer is rare. It is palpable in less than 3 centimeters and can be seen anywhere, but internal organs are rare.4 The pathogenesis of the disease is unknown. If its size is more than 4 cm and grow fast, the possibility of malignancy is high. In 1984, Degefu et al.5 reported GCT on the clitoris, and there are only a dozen case reports worldwide.6789
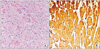
A 45-year-old married woman visited the outpatient clinic on the left side of the clitoris for a mass that had been palpable for two years. There was no history of any particular trauma. At first it was very small, but it was getting bigger. It was painless, but uncomfortable. Two children were delivered by vagina, the menstruation was menopausal two years ago. She did not take hormones after menopause. She had no specificity in family and past histories. No specific findings in the laboratories. The ultrasound showed a round 25 mm mass without blood flow (Fig. 1A). There were no abnormalities in uterus and both ovaries in vaginal ultrasound. Under general anesthesia, vasopressin was injected around the mass in the lithotomy position. After complete resection, compression bandages were wrapped for 24 hours to prevent hematoma development. The resected specimen was grossly firm, gray-white, and well-circumscribed solid mass (Fig. 1B). She was discharged without any problems the next day. Microscopically, it was composed of large ovoid cells with abundant cytoplasm, arranged in sheets and surrounded by collagen and boundaries were clear and contained eosinophilic granules (Fig. 2A). Immunohistochemical study was positive for S-100 protein (Fig. 2B). The margins were free of disease, and no malignant features were identified. So far she has been without a recurrence for one year.
Most of GCTs are less than 3 cm in size, and they are more common in black women and occur in the 40s to 60s. Benign lesions are sudden onset and grow slowly, and symptoms are nearly nothing but a solid mass.10 The patient also visited a 45-year-old woman with a solid mass that was suddenly touched. GCTs can occur anywhere in the body. However, it occurs predominantly in the surface tissues and occurs in about 25% of the tongue.11 Parenchyma, subcutaneous tissue, and dermis accounts for about 15% of all cases. And they rarely come from skeletal muscles. The patient's lesion was also parenchymal and subcutaneous, and the skin was intact. The gastrointestinal tract accounts for about 5% of all GCTs. The lesion is almost a single mass, and only 10% is multiple. Only when the lesion is large and in a critical location, it causes obstructive or pressure symptoms. The patient was also a single lesion and had no symptoms. Malignancy is rare, but the cell shape suggests malignancy or metastasis to regional the lymph nodes. The malignant grows quickly, is over 4 cm in size, and has symptoms like ulcers. Microscopically, GCTs are distinguished by the presence of eosinophilic cytoplasmic granules and rounded small nuclei with dense chromatin. The tumor cells stain positively for S-100 protein, neuron-specific enolase.11 This patient was also stained positive for S-100 protein. Ultrasonography shows a hypoechoic mass with a clear border. This disease requires differentiation from all benign diseases of the external genitalia, especially angiomyxoma, which may occur after menopause.12 There are many recent studies on the association between female disease and Jun activation-domain binding protein 1 (Jab1) and p27kip1, it would be helpful to do the test in the above disease.13 Treatment is complete resection including margin and recurrence is common. There have been attempts to treat radiation and chemotherapy, but they have not been successful.14 The recurrence rate is 2% to 8% when negative resection margin is negative, and increases to 20% when resection margin is positive.15 One study reported that surgery after isophosphamide, etoposide, and cisplatin neoadjuvant chemotherapy was successful in a GCT of the uterine cervix and there was no recurrence.16 More research is needed in the future for treatment. Even if benign, marginal invasion is common, so complete resection of the marginal zone is the best way to prevent recurrence and malignancy. We report a very rare case of GCT in the clitoris and a case without recurrence for 1 year with clear resection margins without marginal invasion.
Figures and Tables
References
1. Abrikossoff A. Myomas originating from transversely striated voluntary musculature. Virchows Arch Pathol Anat Physiol Klin Med. 1926; 260:215–233.
2. Koh MW, Bae JJ, Kim MJ. A case of granular cell tumor of anterior vaginal wall. Korean J Obstet Gynecol. 2007; 50:1171–1174.
3. Cheewakriangkrai C, Sharma S, Deeb G, Lele S. A rare female genital tract tumor: benign granular cell tumor of vulva: case report and review of the literature. Gynecol Oncol. 2005; 97:656–658.
4. Kardhashi A, Assunta Deliso M, Renna A, Trojano G, Zito FA, Trojano V. Benign granular cell tumor of the vulva: first report of multiple cases in a family. Gynecol Obstet Invest. 2012; 73:341–348.
5. Degefu S, Dhurandhar HN, O'Quinn AG, Fuller PN. Granular cell tumor of the clitoris in pregnancy. Gynecol Oncol. 1984; 19:246–251.
6. Nakayama M, Kobayashi H, Takahara T, Nishimura Y, Fukushima K, Yoshizawa K. A comparison of overall survival with 40 and 50 mg/m2 pegylated liposomal doxorubicin treatment in patients with recurrent epithelial ovarian cancer: Propensity score-matched analysis of real-world data. Gynecol Oncol. 2016; 143:246–251.
7. Slavin RE, Christie JD, Swedo J, Powell LC, Jr . Locally aggressive granular cell tumor causing priapism of the crus of the clitoris. A light and ultrastructural study, with observations concerning the pathogenesis of fibrosis of the corpus cavernosum in priapism. Am J Surg Pathol. 1986; 10:497–507.
8. Ortiz-Hidalgo C, de la Vega G, Moreno-Collado C. Granular cell tumor (Abrikossoff tumor) of the clitoris. Int J Dermatol. 1997; 36:935–937.
9. Laxmisha C, Thappa DM. Granular cell tumour of the clitoris. J Eur Acad Dermatol Venereol. 2007; 21:392–393.
10. Levavi H, Sabah G, Kaplan B, Tytiun Y, Braslavsky D, Gutman H. Granular cell tumor of the vulva: six new cases. Arch Gynecol Obstet. 2006; 273:246–249.
11. Hale JL, Schwenk GR Jr, Wilson DB, Moriarty AT, Crabtree WN. Diagnosis of a vulvar granular cell tumor by fine needle aspiration biopsy A case report. Acta Cytol. 2002; 46:373–376.
12. Lee SH, Cho YJ, Han M, Bae JW, Park JW, Oh SR, et al. Superficial angiomyxoma of the vulva in a postmenopausal woman: a case report and review of literature. J Menopausal Med. 2016; 22:180–183.
13. Kim M, Kim TH, Lee HH. The relevance of women's diseases, jun activation-domain binding protein 1 (JAB1) and p27kip1. J Menopausal Med. 2016; 22:6–8.
14. Papalas JA, Shaco-Levy R, Robboy SJ, Selim MA. Isolated and synchronous vulvar granular cell tumors: a clinicopathologic study of 17 cases in 13 patients. Int J Gynecol Pathol. 2010; 29:173–180.
15. Goel G, Singh N, Gupta R, Jain S. Recurrent benign cutaneous granular cell tumor: A case report. J Cytol. 2013; 30:287–288.
16. Guo N, Peng Z, Yang K, Lou J. Uterine cervical malignant granular cell tumor. J Obstet Gynaecol Res. 2012; 38:944–947.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download