Abstract
Objectives
Diabetes is a chronic disease which is common in menopause period. Performing self-care behaviors is effective method for control of diabetes. This study aimed to investigate the effect of counseling on self-care behaviors in menopause diabetes women in 2016 in Hamadan, Iran.
Methods
In this study, 80 menopausal women were randomly selected and allocated to the experimental and control groups (40 per group). Data collected by a questionnaire included of demographic information, self-care behaviors, fasting blood sugar (FBS) and glycosylated hemoglobin (HbA1c). In the experimental group, training program was run during four sessions in the form of weekly group consulting sessions. During this period, the control group only received routine cares. Three months after intervention (group consultation) self-care behaviors, FBS and HbA1c were compared between two groups. Data were analyzed using SPSS 16 software.
Results
The self-care score in the experimental group increased from 49.6 ± 12.2 before the intervention to 66.6 ± 9.3 after the intervention (P < 0.05). Also in the control group average of self-care score changed from 57.6 ± 11.5 to 62.0 ± 11.6 (P < 0.05). Three months after the group consultation, there was a significant difference between two groups in the dimensions of diet (P = 0.013), exercise (P = 0.009) and foot care (P < 0.001). In the experimental group, FBS decreased from 148.8 ± 62.4 mg/dL to 128.9 ± 46.3 mg/dL. Also, HbA1c changed from 7.2 ± 1.8 g/dL to 6.8 ± 1.6 g/dL three months after intervention (P = 0.058). No significant changes were observed in FBS and HbA1c in the control group.
Women constitute half of the world's population and the most important pillars of society and family. Community health depends on provision of women health.1 In the twenty-first century, variation in the pattern of diseases and increase in the incidence of chronic diseases such as diabetes are the results of changes in people life style and longevity.2 With increased longevity, it is expected that women spend a third of their life, on average, in postmenopausal period.3 Menopause is accompanied by hormonal changes and decreased in sensitivity to insulin. Increased fat mass followed by aging in postmenopausal women causes reduction in Adiponectin and resistance to insulin.45 Diabetes is a metabolic disease which is associated with absolute or relative deficiency of insulin, increase in blood glucose and dysfunction in fats, proteins and carbohydrate metabolism. The World Health Organization (WHO) has predicted that in 2025, about 6.8% of the population in Iran will engage in diabetes disease. It is the most common cause of kidney disease, blindness and non-traumatic amputation. Annually, more than 250 people in the country die from complications arising from diabetes and twice that number is also at risk of heart attacks and strokes.6
There are two types of diabetes in which type II diabetes is the more common and about 90% to 95% of diabetic people in the world are suffering from this type of diabetes.7 Based on studies in different places of Iran, the prevalence of diabetes was variable from 4.2% to 15.9%.8 Optimum metabolic controls, prevention of complications are the aims in controlling diabetes.9 Treatment of diabetes aims to control of blood sugar in normal range without hypoglycemia. Due to the fact that more than 95% of treatment process is done by patients and physicians/medical team have little control over patients in the intervals between meetings.10 This requires to consider promotion of self-care activities including physiological, social, emotional and spiritual ones much more.6 Patients with diabetes require to perform special self-care behaviors in the their lifetime.11 In fact, self-care is an active process and it is an activity that is driven by patients which is necessary to prevent short-term and long-term complications of diabetes.12
Promotion of self-care is possible by training. Training patient is a fundamental component in controlling diabetes. The success of diabetes treatment depends on the ability of people with diabetes to effectively have self-care behavior such as having prescribed medicine, following the diet and exercise, self-monitoring of their fasting blood sugar (FBS) and psychological adjustment to the diabetes' life. However, many patients with diabetes encounter several obstacles including lack of appropriate awareness of the disease and its treatment, lack of adequate confidence or skill to effectively control diabetes, lack of financial resources to provide medicines and physical limitations for doing efficient self-care.13 Patients' awareness about self-care strategies and continuous monitoring of blood glucose can be lead to prevention of early and late complications of the disease, ensuring patient prolonged life and reduction in health care costs. Undoubtedly, achieving these goals requires public programs and continuous trainings.14 Consultation is a process that takes steps to strengthen the skills and abilities of people in order to enhance their health.15 Consultation plays an important role in management of chronic diseases.16 Studies conducted by Baghery et al.17 and Karimoi et al.18 showed that consultation led to improvement in the quality of life (QOL) in patients with chronic disease. Although, consultation usually is done individually, group counseling can provide some advantages such as necessary sense of security and free interaction with other members in the group. In this way, the possibility of addressing the needs of each member of group using peer experiences is supplied. Besides that, it is more affordable in terms of time and cost.8 Meanwhile, consulting is one of the main roles of health providers, it is less considered by them.19 Due to the short-term and long-term complications of diabetes during menopause, diabetic patients encourage to modify their life style and performing self-care behaviors.20
Women are considered as central pillars of their family and women health have special effects on family health.21 It is necessary to understand the problems which are reducing the health status of menopausal women. One of the important tasks of health providers to support women health in menopausal period and attempt for their empowerment.22 Consultation for self-care is useful to improve treatment results in menopausal women with diabetes. The overall objectives of counseling on self-care in the patients are supporting decision making, self-care behavior, problem solving, active cooperation with health care providers, improving clinical outcomes and improve QOL.2324 Therefore, this study has been implemented with the aim of determining the effect of group counseling on self-care behaviors among menopausal women with diabetes.
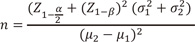
This research was a quasi-experimental study. The population of study were menopausal women with type II diabetes who referred to Diabetes Research Center of Hamadan city, Iran in year 2016. Subjects of this study randomly selected and allocated into two groups (the experimental and the control groups). The sample size in this study was calculated based on the following formula.
Sample size was estimated with information of (α = 0.05, β = 0.020), and self-care score was based on a previous study.25 According to formula, the number of samples in the each group was estimated as 40. Inclusion criteria consisted of women with confirmed diabetes with lasting at least a year from the onset of their diabetes. Lack of suffering from advanced diabetes complications (such as kidney failure, stroke, myocardial infarction, malignant tumors). Exclusion criteria included lack of participate in consultation sessions and unwillingness to continue this investigation.
Before the study, the necessary explanations were given to individuals about the purposes of this study and written consent was obtained from subjects. Data collection tool included structured questionnaire of demographic information (age, education, occupation), diabetes characteristics (duration of diabetes, medications and associated complications) and self-care behaviors of the Summary of Diabetes Self-Care Activities (SDSCA). The self-care questionnaire developed by Toobert and Glasgow26 and included 21 questions about individual caring activities.19 The validity and reliability of the questionnaire was approved by Parizad et al.25 in year 2013 with Cronbach's α of 0.80. The self-care questionnaire reported the rate of individuals' commitment toward self-care behaviors in the last 7 days. Questions included diet (5 items), exercise (2 items), glycemic control (2 items), foot care (3 items), consumption of diabetic medication regimen (3 items), two questions related to glycosylated hemoglobin (HbA1c) and FBS which were checked in the last laboratory test of patient and smoking (4 items). In case of the performing desired behavior in each day, one point was considered. Zero point was accounted for failure to do it. The sore of SDSCA ranged from 0 to 105. The highest possible score in this tool was 105 which was indicated the highest degree of self-care ability. Self-care score was classified in terms of obtained scores to three levels of good (grades of 76-105), medium (51-75) and poor (less than 50). Questionnaire were completed by the individuals of two groups before and three months after intervention. The amount of FBS and HbA1c was measured before and three months after intervention in a reference laboratory in Hamadan city.
In the experimental group, women were divided to small groups of 8 to 10 individuals to participate in counseling sessions. Counseling sessions were held once a week consisted of four 45 to 60 minute sessions. Consultation was offered based on correcting food habits, adjusting the diet according to reduction of the Glycemic index (GI) for improving nutritional quality, appropriate consumption of fruit and vegetables.5 Moreover, telephone follow-up was done twice a month for three months (a total of six times) after the last session of consultation. Time of making phone calls was determined with the agreement of the patients. The content of the telephone conversation included: assessing the status of glycemic control, diet, exercise, self-monitoring of blood glucose, medication regimen, and answering the questions of patients. During this time, control group only received routine care including control of FBS, blood pressure and treatment of complications of patients. However, after completion of the study, all educational content was also taught to the control group. Information was gathered by questionnaire before and three months after the last session of counseling from the two groups.
Ultimately, both experimental and control groups were compared in terms of the level of FBS, HbA1c and self-care before and after the group consultations. Data were analyzed by statistical software of SPSS version 16 (SPSS Inc., Chicago, IL, USA). Descriptive statistics were implemented in order to estimate the mean, standard deviation (SD) and frequency of distribution. Independent t-test was used to compare the mean of variables in two groups while analysis of variance (ANOVA) was utilized to compare different aspects of self-care controlling pretest score and individual characteristics. Paired-t-test was used to compare changes within the groups. The significance level was considered to be less than 0.05 (P < 0.05).
The mean ± SD age of postmenopausal women in experimental group was 55.0 ± 5.3 and in control group was 55.0 ± 4.6 years (P > 0.05). Most of them were married (77% in experimental and 85% in control group, P > 0.05). No significant difference was observed on body mass index and employment status between two groups (P > 0.05).
Based on the results in Table 1, about half of participates had a family history of diabetes. Treatment method used by the majority of patients was oral tablet, followed by injection of Insulin. Most participants (55%) had other complications. A total of 32 participants had a history of diabetes for 1 to 5 years and only 9 patients had more than 15 years history of diabetes.
Based on the results obtained in the Table 2, before the intervention, the mean ± SD score of self-care in the experimental group was at weak level that increased to moderate level after the intervention (from 49.6 ± 12.2 to 66.6 ± 9.3; P < 0.001). Self-care score in the control group increased from 57.6 ± 11.5 to 62.0 ± 11.6 (P < 0.05) as well. Comparing the two groups on self-care scores showed significant differences after the intervention (P < 0.001). To study the changes within the experimental group domains showed that scores of diet, exercise, blood sugar control and foot care have been increased significantly (P < 0.001), except in the domain of medication that not changed significantly (P = 0.148). No significant changes were seen in the control group.
Based on the results obtained in Table 3, the average HbA1c in the experimental group decreased from 7.2 ± 1.8 to 6.8 ± 1.6, although this change was not significant (P = 0.058). In the control group there was no significant change in HbA1c (P = 0.922). Average of FBS in the experimental group significantly decreased from 148.8 ± 62.4 to 128.9 ± 46.3 (P < 0.001). No significant change in FBS was observed in the control group (P = 0.861). Comparison of two groups after three months showed that the average amount of HbA1c decreased in experimental group, however no significant difference was seen between two groups in term of HbA1c three months after intervention (P = 0.052). A significant difference was observed between the two groups in term of FBS after three months of intervention (P < 0.01).
The findings of this study revealed a positive effect of group counseling on self-care and glycemic control in menopausal women with type II diabetes. In the form of four one-hour sessions of group counseling, participates' self-care behaviors significantly improved. In this study, before the intervention about half of women (49.6%) were doing self-care behaviors. It is recommended that 95% of diabetes patients perform self-care behaviors and modify their life styles.25
After the intervention, significant changes were seen in experimental group in terms of exercise, diet, foot behaviors (P < 0.001). Similar results were seen in a study Karlsen et al.27, who studied the effect of group counseling on mental health and glycemic control in adults with diabetes. They found that group counseling program in six sessions significantly reduced the stress and self-punishment related to diabetes. Although in this study, only the psychological effects of group counseling were considered, but due to association between psychological and physical aspects the results of this study may be attributed to reduction of stress in patients as well. Stress reduction is likely to cause metabolic control in patients those were participated in group counseling.
Jalilian et al.28 examined the self-care educational program in type II diabetic patients. Their results showed that the implementation of a six-session training program increased 34% in self-care behaviors. In the present study, the mean of self-care score also increased in the control group. This could be due to care given to the control group in Research Center of Diabetes during the study.
One of the most important aspects of the self-care in the present study was foot care. The foot care in diabetes patients prevent the neurological and vascular dysfunctions which lead to leg ulcers, infection and eventually gangrene of the foot. Even though, lack of appropriate treatment of diabetic foot ulcers are associated with risk of death. Unfortunately, about 15% of patients with diabetes mellitus are diagnosed with foot ulcers. This condition is leading to leg amputation in 14% to 24% of these patients. The results of this study indicated a significant increase in attention to foot care among patients in the experimental group compare to the control group which was in consistent with the results of other studies.2429 According to the results obtained foot care of patients was easy and had no cost. It seems that training be beneficial in this regard.
One of the important steps in controlling diabetes is taking the prescribed medications. The study results indicated that modest rose in the consumption of medications in study groups that was not consistent with previous studies.2830 This could be due to patients gastrointestinal discomfort, illiteracy, age over 50 years, believed in herbal and traditional medicine rather than medications prescribed regimen in our patients. The current results did not show a significant change in individual control of blood sugar. The result could be due to lack of sufficient knowledge in the use of glucometer for blood glucose in patients which is in line with another study conducted in Iran.31
In the experimental group physical activity increased significantly, whereas FBS and HbA1c decreased (P < 0.001). Considering, the relationship between physical activity and blood glucose levels in diabetic patients, it can be claimed that physical activity decreased blood sugar in patients. Parham and colleagues study31 showed a significant relationship between physical activity and blood sugar, and physical activity improved blood sugar control that were in consistent with our findings. Other research done at the University of Queensland, Australia in 2012 showed beneficial effects of exercise for preventing the type 2 diabetes and to improve glycemic control in diabetic patients.32
The self-care consultations increased 55% in consumption of fruit and vegetables. Most of participates in the participants consumed fruit and vegetables four times per day. Only 18% of them consumed high-fat foods per week. Fifty three per cent of them had 3 to 4 times a week consumption of carbohydrates. Overall, three months after intervention a significant increase was seen in the score of diet domain in the experimental group (P < 0.01). Another study had done in Iran showed 38.8% of diabetes patients continually followed the recommended diet.33 A good adherence of food plan and diet control in patients of this study can be due to effects of group counseling and follow-up by telephone.
In general, three months after the intervention, FBS and HbA1c decreased in the experimental group compared to the control group. Monitoring of FBS and HbA1c evaluated metabolic control and effectiveness of treatment in diabetes patients. Similarly, previous study showed a significant relationship between self-care behaviors and HbA1c in patients with type II diabetes.34 Rakhshandero and colleagues35 showed counseling program could improve metabolic control. Kashfi and colleagues36 suggested that diet and walking could reduce the HbA1c levels in diabetic patients. Milenković et al.37 investigated the impact of education on well-being and metabolic control of diabetes patients. They found training sessions significantly improved metabolic control of patients and reduced 16% of their HbA1c.37 Obviously, counseling with diabetes patients should be in accordance of ethical issues in medical education.38
The limitations of current study were: limited number of menopausal women, short period of follow-up and conducting the study only in one center. Although, the patients were referred to this center from all parts of Hamadan city. Therefore, the results may not be generalized for other people and other communities. It is suggested that such studies will conduct in a larger population and wider ranges. It also recommended that future studies will compare the impact of individual counseling with group counseling on self-care behaviors among diabetes patients.
Figures and Tables
Acknowledgement
This paper was extracted from Master of Science thesis in Consulting in Midwifery in Hamadan University of Medical Sciences. The Ethics Committee approval code of this study was IR.UMSHA.REC.1394.207. This research was registered in Iranian Registry of Clinical Trials (IRCT2015062713405N10). The authors sincerely appreciated from Research Deputy of Hamadan University of Medical Sciences for his financial support. In addition, all participants and personnel in Research Center of Diabetes Control who helped us in the research process are appreciated.
References
1. Rossouw JE, Anderson GL, Prentice RL, LaCroix AZ, Kooperberg C, Stefanick ML, et al. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results from the Women’s Health Initiative randomized controlled trial. JAMA. 2002; 288:321–333.
2. Aghamolaei T, Eftekhar H, Mohammad K, Sobhani A, Shojaeizadeh D, Nakhjavani M, et al. Influence of educational intervention using interaction approach on behavior change, hemoglobin A1c and health-related quality of life in diabetic patients. J Sch Public Health Inst Public Health Res. 2005; 3:1–2.
3. Speroff L, Fritz MA. Clinical gynecologic endocrinology and infertility. 7th ed. Philadelphia, PA: Lippincot Williams Wilkins;2005.
4. Tofighi A. Impact of water training on serum adiponectin level and insulin resistance in obese postmenopausal women. Iran J Endocrinol Metab. 2010; 12:260–267.
5. Chae HD, Choi SY, Cho EJ, Cho YM, Lee SR, Lee ES, et al. Awareness and experience of menopausal symptom and hormone therapy in korean postmenopausal women. J Menopausal Med. 2014; 20:7–13.
6. Shidfar F, Yarahmadi SH, Jalali M, Eftekhari MH, Hosseyni SH, Ahari L. Effects of purified omega-3 fatty acids in postmenopausal women with type 2 diabetes. Iran J Endocrinol Metab. 2007; 9:229–234.
7. Darvishpoor Kakhki A, Abed Saeedi Z, Yaghmaie F, Alavi Majd H, Montazeri A. Survey correlation between quality of life and disease and demographic variables of diabetic patients referred to Tehran hospitals in 2004. Iran J Endocrinol Metab. 2006; 8:49–56.
8. Esmaili A, Asadnia S, Easazadeh A, Amirsardari L, Issazadeghan A, Ansari B. Evaluation of the effectiveness of cognitive behavioral therapy on decreasing depression levels and improving the lifestyle of patients with type 2 diabetes. J Urmia Univ Med Sci. 2013; 24:812–822.
9. Vosoghi Karkazloo N, Abootalebi Daryasari G, Farahani B, Mohammadnezhad E, Sajjadi A. The study of self-care agency in patients with diabetes (Ardabil). Mod Care J. 2012; 8:197–204.
10. Vinter-Repalust N, Petricek G, Katić M. Obstacles which patients with type 2 diabetes meet while adhering to the therapeutic regimen in everyday life: qualitative study. Croat Med J. 2004; 45:630–636.
11. Mazlom S, Firooz M, Hasanzade F, Kimiaee S, Raoufsaeb A. The effect of group counseling on physiological aspect of self-care and HbA1C level of patients with diabetes type II. Evid Based Care J. 2015; 5:25–36.
12. Aghvamy MS, Mohammadzadeh S, Gallalmanesh M, Zare R. Assessment the education compariment to two ways: groupe education and computer education on quality of life in the children 8-12 years suffering from asthma in the Valiasr hospital of Zanjan. ZUMS J. 2011; 19:78–85.
13. Gallant MP. The influence of social support on chronic illness self-management: a review and directions for research. Health Educ Behav. 2003; 30:170–195.
14. Mahmoodi A, Alavi M, Mosavi N. The relationship between self-care behaviors and HbA1c in diabetic patients. Sci J Hamadan Nurs Midwifery Fac. 2012; 20:20–30.
15. United States Agency for International Development. Population reports GATHER approach to counseling about injectables: Depo-Provera and Noristerat. Baltimore, MD: United States Agency for International Development;Cited by 1995 Aug 2. Available from: https://www. k4health.org/sites/default/files/305360.pdf.
16. Adler AI, Stratton IM, Neil HA, Yudkin JS, Matthews DR, Cull CA, et al. Association of systolic blood pressure with macrovascular and microvascular complications of type 2 diabetes (UKPDS 36): prospective observational study. BMJ. 2000; 321:412–419.
17. Baghery H, Memarian R, Elhani F. Survey the effect of group counseling on quality of life in myocardial infarction patients who have been referred to the clinics of Imam Khomeini and Shariati Hospitals in Tehran. Hakim. 2004; 6:89–95.
18. Karimoi HM, Pourdehghan M, Faghihzadeh S, Montazeri A, Milani JM. The effects of group counseling on symptom scales of life quality in patients with breast cancer treated by chemotherapy. J Kermanshah Univ Med Sci. 2006; 10:10–22.
19. Taylor CR, Lillis C, LeMone P, Lynn P, LeBon M. Study guide for fundamentals of nursing: the art and science of nursing care. 7th ed. Philadelphia, PA: Lippincott Williams & Wilkins;2011.
20. Taechakraichana N, Jaisamrarn U, Panyakhamlerd K, Chaikittisilpa S, Limpaphayom KK. Climacteric: concept, consequence and care. J Med Assoc Thai. 2002; 85:Suppl 1. S1–S15.
21. Lazarus JV, Rasch V, Liljestrand J. Midwifery at the crossroads in Estonia: attitudes of midwives and other key stakeholders. Acta Obstet Gynecol Scand. 2005; 84:339–348.
22. Parsa P, Tabesh RA, Soltani F, Karami M. Effect of group counseling on quality of life among postmenopausal women in Hamadan, Iran. J Menopausal Med. 2017; 23:49–55.
23. Barati M, Ahmadpanah M, Shirahmadi S, Bashirian S, Parsa P, Holsboer-Trachsler E, et al. Differential impact of sociodemographic variables on the quality of life of menopausal Iranian women. Avicenna J Neuro Psycho Physiol. 2016; 3:e39026.
24. Funnell MM, Brown TL, Childs BP, Haas LB, Hosey GM, Jensen B, et al. National standards for diabetes self-management education. Diabetes Care. 2010; 33:S89–S96.
25. Parizad N, Hemmati Maslakpak M, Khalkhali HR. Promoting self-care in patients with type 2 diabetes: Teleeducation. Hakim. 2013; 16:220–227.
26. Toobert D, Glasgow R. Assessing diabetes self-management: the summary of diabetes self-care activities questionnaire. In: Bradley C, editor. Handbook of psychology and diabetes: a guide to psychological measurement in diabetes research and practice. London, UK: Harwood Academic Publishers;1994.
27. Karlsen B, Idsoe T, Dirdal I, Rokne Hanestad B, Bru E. Effects of a group-based counselling programme on diabetes-related stress, coping, psychological well-being and metabolic control in adults with type 1 or type 2 diabetes. Patient Educ Couns. 2004; 53:299–308.
28. Jalilian F, Motlagh FZ, Solhi M. Effectiveness of education program on increasing self management among patients with type II diabetes. J Ilam Univ Med Sci. 2012; 20:26–34.
29. Hazavehei S, Sharifirad G, Mohabi S. The effect of educational program based on health belief model on diabetic foot care. Int J Diabetes Dev Ctries. 2007; 27:82–90.
30. Rubin RR, Peyrot M, Saudek CD. Differential effect of diabetes education on self-regulation and life-style behaviors. Diabetes Care. 1991; 14:335–338.
31. Parham M, Riahin AA, Jandaghi M, Darivandpour A. Self care behaviors of diabetic patients in Qom. Qom Univ Med Sci J. 2012; 6:81–87.
32. Hordern MD, Dunstan DW, Prins JB, Baker MK, Singh MA, Coombes JS. Exercise prescription for patients with type 2 diabetes and pre-diabetes: a position statement from Exercise and Sport Science Australia. J Sci Med Sport. 2012; 15:25–31.
33. Aghamilaei T, Sobhani A, Yusefi H, Asadi Noghabi F. Behavior and metabolic control in diabetic patients in Bandar Abbas diabetic clinic. Med J Hormozgan Univ. 2003; 7:5–11.
34. Shayeghian Z, Aguilar-Vafaie M, Ali Besharat M, Amiri P, Parvin M, Roohi Gilani K. The association between self-care and control of blood sugar and health-related quality of life in type II diabetes patients. Iran J Endocrinol Metab. 2014; 15:545–551.
35. Rakhshandero S, Ghafari M, Heidarnia AR, Rajab A. Effectiveness of an educational intervention on metabolic control of diabetic patients attending Iranian diabetes association. Iran J Diabetes Lipid Disord. 2009; 1:57–64.
36. Kashfi SM, Khani Jyhouni A, Bahadori Khalili R, Hatami M. Evaluation of the effects of educating about nutrition and jogging on the blood sugar of type II diabetic patients of a clinic in Shiraz, Iran. Hakim Health Sys Res. 2009; 12:54–60.
37. Milenković T, Gavrilović S, Percan V, Petrovski G. Influence of diabetic education on patient well-being and metabolic control. Diabetol Croat. 2004; 33:91–96.
38. Kim TH, Choi SD, Woo SH. An ethical issue in medical education of obstetrics and gynecology. J Menopausal Med. 2015; 21:130–132.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download