Abstract
Objectives
This study was done to determine the effect of multiparity and prolonged lactation on bone mineral density (BMD).
Methods
This cross-sectional study included 196 perimenopausal and postmenopausal women aged 40 to 60 years old. Age, body mass index (BMI), menopausal status, duration of menopause, parity and total duration of lactation, nutritional history were recorded. Lumbar spine (LS; L2-L4) and femur neck (FN) BMD were measured using dual energy X-ray absorptiometry. Correlation of parity and lactation with BMD were investigated using multiple regression analysis.
Results
Parity was inversely correlated to BMD for LS (β = −0.266, P = 0.001) and FN (β = −0.380, P = 0.000). This relation remained significant even after adjusting for age, BMI and duration of menopause. Duration of lactation was inversely correlated with BMD for LS (β = −0.271, P = 0.001) but no for FN (β = −0.124, P = 0.130).
Osteoporosis is characterized by low bone mass with micro architectural deterioration of bone tissue leading to enhance bone fragility, thus increasing the susceptibility to fracture.1 Osteoporotic fractures are a major cause of morbidity and mortality (3%) in the elderly. Bone mineral density (BMD) is the best predictor for osteoporotic bone fractures. Several contributory factors like genetics, nutrition, and physical activity are considered essential in regulating bone metabolisms as well as reaching peak bone mass in young age. Both pregnancy and lactation are intense physiologic conditions with high calcium homeostasis, mostly occurring in young woman. In pregnancy 2% to 3% of maternal calcium is transferred to fetus mostly in second half of pregnancy, approximately 30 mg calcium mobilized from maternal sources. During lactation mother loses further 300 to 400 mg calcium per day in breast milk.2 Lactational amenorrhea (Hypoestrogenemia) further accentuate bone loss. Endocrine changes induce compensatory mechanism like higher circulating levels of dihydroxy-vitamin D, changes in parathyroid hormone (PTH), growth hormone, prolactin, as well as increase intestinal absorption, renal conservation of calcium and pregnancy associated weight gain. These changes counterbalance the negative effect of pregnancy on BMD. Despite the involvement of several counter-regulatory pathways during pregnancy BMD decreases about 3%. During initial 6 months of lactation there is 5% to 6% decrease in BMD which resolves in next 6 months period. Thus, pregnancy and lactation can be beneficial or detrimental to BMD. Several studies have shown positive, negative and no correlation between parity and BMD. Most of these studies were done in developed countries where parity is not that high, and not that frequent, breast feeding is not that prolonged and nutrition of the women are good. There is no study from India which showed effect of multiparty and prolonged lactation on BMD. We undertook this study to see effect of multiparty and prolonged lactation on BMD for lumbar spine (LS) and femur neck (FN).
This was hospital based, cross-sectional study done in department of obstetrics and gynecology in tertiary care institute from June 2013 to May 2015. Consecutively 196 women aged 40 to 60 years were enrolled in the study after taking the informed consent. The study protocol was approved by institute ethics committee. A questionnaire including age, height, weight, parity, total lactation period, food habits, any medicinal intake which affect BMD, smoking, excessive coffee intake, menopausal status, age at menopause and years since menopause and socioeconomic status were noted for all the subjects. Total lactation period was described in total months for all the combined pregnancies. Detailed history and examination were carried out on all the subjects. Our exclusion criteria were history of fracture, uncontrolled thyroid disorder, parathyroid disorder, women on steroids or other drugs which affects BMD and prolonged physical immobilization. LS (L2-L4) and FN BMD was measured by dual energy X-ray absorptiometry (DXA) using the equipment (QDR-4500SL; Hologic Inc., Bedford, MA, USA).
Firstly, descriptive statistics was used to calculate the mean ± standard deviation (SD). Correlation between independent variables and the dependent variables - LS and FN BMD was analyzed using the Pearson’s correlation. Secondly, simple linear regression was performed to assess the effect of parity and lactation independently on BMD. Thirdly, multiple regression analysis models were then constructed to evaluate the effect of parity, lactation, age, body mass index (BMI), lactation and years since menopause on BMD. Enter method was used for multiple regression analysis. A 95% limit and 5% level of significance were adopted. Therefore, a P value of less than 0.05 was considered significant. Statistical analysis was performed using the SPSS software package (version 22.0; SPSS Inc., Chicago, IL, USA).
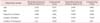
The clinical characteristics are given in Table 1. In this study parity was found to be inversely proportional to BMD in relation to LS (r2 = 0.405, standardized regression coefficient (β = −0.637, P = 0.000) as well as to FN (r2 = 0.390, β = −0.625, P = 0.000) in linear regression analysis. The same relationship was found after adjusting for age, BMI, lactation, duration of menopause (β= −0.266, P = 0.001 and β= −0.380, P = 0.000 for LS and FN respectively) (Table 2, Fig. 1, 2). Duration of lactation was also inversely proportional to BMD for LS (r2 = 0.336, β = −0.580, P = 0.000) and for FN (r2 = 0.266, β = −0.516, P = 0.000) in linear regression. But in multiple regression analysis, this relationship remained significant after adjusting for age, BMI, parity and duration of menopause only for LS (β = −0.271, P = 0.001) but not for FN (β = −0.124, P = 0.130) (Table 2, Fig. 3, 4).
We observed negative and statistically significant correlation between parity and BMD. With increasing parity there is decrease in BMD at both places for LS as well as for FN. This relationship remained significant after adjusting for age, BMI, and menopausal years. It may be that pregnancies are too many and quite frequent in this population. Nutritional status of the subjects was also marginal as our subjects belonged to low or lower middle socioeconomic background. Our subjects were not on any supplements and their diet didn’t contain dairy products or other calcium rich foods. The subjects were not on any oral contraceptive pill, hormonal replacement therapy or any other drugs which might affect BMD. Our finding are consistent with the finding of Allali et al.3 They reported a significant negative correlation between parity with the spine as well as the FN BMD but Gur et al.4 observed significant decrease in BMD with parity for spine but not for FN. Hreshchyshyn et al.5 reported that BMD of FN decreased with an increasing number of live birth, whereas there was no change for the LS. Other authors also observed that multiparity was a risk factor for lower BMD.6789101112 On the contrary, association of high parity with high BMD was observed by Karlsson et al.13 and Cure-Cure et al.14 The relationship between parity and BMD has also been evaluated among old Amish women characterized by high parity. Streeten et al.15 observed in this population a positive and statistically significant correlation between parity and BMD. Weight gain associated with increasing parity possibly could explain this finding. All these studies suggested an association between parity and BMD. Few studies found no association between parity and BMD.161718 The number of pregnancies and duration of lactation are related to each other and it is difficult to differentiate their individual effect on BMD. In our observation with lactation there is decrease in BMD for spine only. Although in graph 4 there is inverse relationship between lactation and BMD for FN but it is not statically significant by multiple regression analysis (P = 0.130). Our observation is similar to the findings of Kojima et al.17 They observed LS BMD was lower in women aged 40 to 44 years who breast feed for a longer duration. Different observation was made by Lenora et al.16 They found lactation didn’t seem to have deteriorating effect on BMD later in the life. In their study, Okyay et al.19 observed that although parity was a protective factor against the development of osteoporosis but extended breast feeding for more than 1 year per child has the highest risk for osteoporosis among their study group specially in the developing countries. Lactation induced hypoestrogenemia superimposed by burden of frequent pregnancies with marginal nutrition couldn’t be compensated by various protective mechanism against osteoporosis. Some previous studies mentioned on the protective effect of lactation on BMD.202122 Some new studies indicate detrimental effect.42324 while some others conclude no significant effect.2526 Our observations are similar to that in the report by Yilmaz et al.27, demonstrating high parity and long term lactation having negative effect on BMD in women of postmenopausal age group.
The reasons to get these discrepancies among different studies are quality of study, different types of studies (comparative groups, population characteristics, number of subjects, follow-up period, statistics), nutritional status of the women, ethnicity, age, age at menarche and menopause, parity, duration of lactation, different skeletal sites for BMD measurement and different method (DXA or quantitative ultrasonography [QUS]) to measure BMD.
Present study suggests that multiparity has detrimental effect on BMD for LS and FN both. Duration of lactation has adverse effect on BMD only for LS. We conclude that multiparity and prolonged lactation have negative impact on BMD especially in a socioeconomic group whose nutritional intake is borderline. Our data support that parity and duration of lactation can be regarded as risk factor for future osteoporosis.
There are certain drawbacks in our study. Firstly it was not a population based study. Secondly sample size was small. Thirdly subjects had to recall duration of lactation in the past. Lastly we didn’t consider physical activity in our subjects. To confirm the findings of the present study a well-designed, observational, population based study with more subjects is desirable.
Figures and Tables
References
1. NIH Consensus Development Panel on Osteoporosis Prevention, Diagnosis and Therapy. Osteoporosis prevention, diagnosis, and therapy. JAMA. 2001; 285:785–795.
2. Kovacs CS. Calcium and bone metabolism in pregnancy and lactation. J Clin Endocrinol Metab. 2001; 86:2344–2348.
3. Allali F, Maaroufi H, Aichaoui SE, Khazani H, Saoud B, Benyahya B, et al. Influence of parity on bone mineral density and peripheral fracture risk in Moroccan postmenopausal women. Maturitas. 2007; 57:392–398.
4. Gur A, Nas K, Cevik R, Sarac AJ, Ataoglu S, Karakoc M. Influence of number of pregnancies on bone mineral density in postmenopausal women of different age groups. J Bone Miner Metab. 2003; 21:234–241.
5. Hreshchyshyn MM, Hopkins A, Zylstra S, Anbar M. Associations of parity, breast-feeding, and birth control pills with lumbar spine and femoral neck bone densities. Am J Obstet Gynecol. 1988; 159:318–322.
6. Demir B, Haberal A, Geyik P, Baskan B, Ozturkoglu E, Karacay O, et al. Identification of the risk factors for osteoporosis among postmenopausal women. Maturitas. 2008; 60:253–256.
7. Kosnayani SA. Calcium intake, relations, physical activities, parity, BMI, and bone density, in post menopausal women. Tasikmalaya, ID: Ciawi;2007.
8. Keramat A, Patwardhan B, Larijani B, Chopra A, Mithal A, Chakravarty D, et al. The assessment of osteoporosis risk factors in Iranian women compared with Indian women. BMC Musculoskelet Disord. 2008; 9:28.
9. Kidambi S, Partington S, Binkley N. Low bone mass prevalence and osteoporosis risk factor assessment in African American Wisconsin women. WMJ. 2005; 104:59–65.
10. Jang SN, Choi YH, Choi MG, Kang SH, Jeong JY, Choi YJ, et al. Prevalence and associated factors of osteoporosis among postmenopausal women in Chuncheon: Hallym Aging Study (HAS). J Prev Med Public Health. 2006; 39:389–396.
11. El Maghraoui A, Guerboub AA, Mounach A, Ghozlani I, Nouijai A, Ghazi M, et al. Body mass index and gynecological factors as determinants of bone mass in healthy Moroccan women. Maturitas. 2007; 56:375–382.
12. Shin CS, Choi HJ, Kim MJ, Kim JT, Yu SH, Koo BK, et al. Prevalence and risk factors of osteoporosis in Korea: a community-based cohort study with lumbar spine and hip bone mineral density. Bone. 2010; 47:378–387.
13. Karlsson C, Obrant KJ, Karlsson M. Pregnancy and lactation confer reversible bone loss in humans. Osteoporos Int. 2001; 12:828–834.
14. Cure-Cure C, Cure-Ramirez P, Terán E, López-Jaramillo P. Bone-mass peak in multiparity and reduced risk of bonefractures in menopause. Int J Gynaecol Obstet. 2002; 76:285–291.
15. Streeten EA, Ryan KA, McBride DJ, Pollin TI, Shuldiner AR, Mitchell BD. The relationship between parity and bone mineral density in women characterized by a homogeneous lifestyle and high parity. J Clin Endocrinol Metab. 2005; 90:4536–4541.
16. Lenora J, Lekamwasam S, Karlsson MK. Effects of multiparity and prolonged breast-feeding on maternal bone mineral density: a community-based cross-sectional study. BMC Womens Health. 2009; 9:19.
17. Kojima N, Douchi T, Kosha S, Nagata Y. Cross-sectional study of the effects of parturition and lactation on bone mineral density later in life. Maturitas. 2002; 41:203–209.
18. Hiz O, Ediz L, Tekeoglu I. Effect of number of pregnancies on bone mineral density. J Int Med Res. 2010; 38:1816–1823.
19. Okyay DO, Okyay E, Dogan E, Kurtulmus S, Acet F, Taner CE. Prolonged breast-feeding is an independent risk factor for postmenopausal osteoporosis. Maturitas. 2013; 74:270–275.
20. Hu JF, Zhao XH, Chen JS, Fitzpatrick J, Parpia B, Campbell TC. Bone density and lifestyle characteristics in premenopausal and postmenopausal Chinese women. Osteoporos Int. 1994; 4:288–297.
21. Feldblum PJ, Zhang J, Rich LE, Fortney JA, Talmage RV. Lactation history and bone mineral density among perimenopausal women. Epidemiology. 1992; 3:527–531.
22. Dursun N, Akin S, Dursun E, Sade I, Korkusuz F. Influence of duration of total breast-feeding on bone mineral density in a Turkish population: does the priority of risk factors differ from society to society? Osteoporos Int. 2006; 17:651–655.
23. Chowdhury S, Sarkar NR, Roy SK. Impact of lactational performance on bone mineral density in marginally-nourished Bangladeshi women. J Health Popul Nutr. 2002; 20:26–30.
24. Khoo CC, Woo J, Leung PC, Kwok A, Kwok T. Determinants of bone mineral density in older postmenopausal Chinese women. Climacteric. 2011; 14:378–383.
25. Jones G, Scott FS. A cross-sectional study of smoking and bone mineral density in premenopausal parous women: effect of body mass index, breastfeeding, and sports participation. J Bone Miner Res. 1999; 14:1628–1633.
26. Carranza-Lira S, Mera JP. Influence of number of pregnancies and total breast-feeding time on bone mineral density. Int J Fertil Womens Med. 2002; 47:169–171.
27. Yilmaz H, Erkin G, Polat HA, Küçükşen S, Salli A, Uğurlu H. Effects of reproductive factors on bone mineral densitometry. Turk J Osteoporos. 2012; 18:8–12.




 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download