Abstract
Objectives
The aim of the study was to compare bone mineral density (BMD) in healthy postmenopausal women to BMD in type 2 diabetic hypertensive postmenopausal women with hyperlipidemia.
Methods
Fifty type 2 diabetic and hypertensive postmenopausal women with hyperlipidemia and 51 age and body mass index (BMI) matched healthy postmenopausal women were included. Lumbar spine and femoral neck BMD were noted in both groups. BMD was measured using dual energy X-ray absorptiometry (DXA). Serum alkaline phosphatase (ALP), calcium and phosphorous were also measured. Pearson correlation coefficients were used to establish the relationship between various clinical characteristics.
Although it is generally accepted that type 1 diabetes is associated with ten percent less bone mineral density (BMD) value compared with no diabetic adults,1,2 there is no consensus on osteoporosis risk in people with type 2 diabetes. Nicodemus and Folsom3 found that women with type 2 diabetes had 1.70-fold higher risk of incident hip fracture than women without diabetes. Two other studies revealed no difference in bone density between type 2 diabetes patients and control subjects.4,5 Some have reported higher bone mass in type 2 diabetic patients relative to no diabetic control subjects.6,7,8
The aim of this study to compare the BMD values of postmenopausal women with diabetic, hypertensive and hyperlipidemic postmenopausal women.
The medical records and BMD measurements of 50 diabetic hypertensive postmenopausal women followed-up at our institution for 4 years were evaluated retrospectively. A cohort of women with known diabetes mellitus (DM) was identified by retrospectively reviewing our patient database. Approval (Date: 1.08.2014, Number: 115) of the Bozok University Medical School's local ethics committee has been obtained. Participants were naturally postmenopausal women under 70 years of age. Exclusion criteria included surgical menopause, smoking, chronic medical illness (Chronic Obstructive Lung Disease). Essential hypertension and diabetes diagnosis was obtained from hospital records. The diagnosis is made in our hospital according to "the Seventh Report of the Joint National Committee on prevention, detection, evaluation, and treatment of high blood pressure" and "World Health Organization (WHO) report on the diagnosis and classification of DM. Women treated with diet or drugs or both; or either a fasting serum glucose value more than 126 mg/dL describe as known DM. Patients who had essential hypertension previously or patients whose blood pressure measurements had been more than 140/90 were included in the study. Those women with and hypertension who had undergone screening BMD in our institution were identified; this group of women comprised our study group. Increase of triglyceride (> 160 mg/dL) or cholesterol levels (> 200 mg/dL) are described as hyperlipidemia. Fifty-one healthy postmenopausal women were also included in the study as the control group. Our institution as a large tertiary referral center, offers a comprehensive menopause health program to our patients with screening BMD, mammogram and Pap-test. Our control group was selected from these patients. Data included the age, gravidity, parity, body mass index (BMI), BMD measurements, serum alkaline phosphatase (ALP), calcium and phosphorous levels were collected. BMD was measured using dual energy X-ray absorptiometry (DXA). BMD measurements of the hip (femoral neck) and lumbar spine (L1-L4) were performed in the anterior posterior (AP) view for the lumbar spine DXA scanner (Hologic QDR 4500 Elite, Bedford, MA, USA). The BMD value for each region was calculated as the ratio of bone mineral content to the area of the interested region (g/cm2). According to WHO criteria, a T-score of ≥ -1 denotes normal bone, a T-score between -1 and -2.5 denotes osteopenia, and a T-score of ≤ -2.5 denotes osteoporosis. BMI wascalculatedbydividingthe weighttothesquare of height (kg/m2).
The statistical analyses were performed using the SPSS statistical package (SSPS Inc., Chicago, IL, USA). The normality of variables were assessed using the Kolmogorov-Smirnov test. The data were reported as mean ± standard deviation (for normally distributed data) or as median and range (for non-normally distributed data). For data with normal distribution, the Student t test was applied. Otherwise, the Mann-Whitney U test was used as a nonparametric test. Correlations between BMD and biochemical marker levels were made using Pearson's correlation coefficient and a partial correlation analysis after adjustments for age and menopausal time. A P value of less than 0.05 was considered significant.
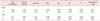
There were no significant differences between two groups in respect to lumbar and vertebral BMD values, age, BMI, gravidity, parity (Table 1). Serum cholesterol and fasting glucose levels were significantly different between each groups (P = 0.0001, P = 0.002). There were no significant differences in serum ALP, calcium and phosphorous levels between the diabetic patients and the controls. There was a negative correlation between lumbar spine BMD and duration of menopause. But we didn't find a correlation between blood glucose levels and BMD (Table 2). After adjusting for age and menopausal time, the partial correlation of BMD with biochemical marker levels were shown in Table 3.
Data regarding the impact of DM on the BMD are controversial. Studies have found that people with type 2 diabetes have increased,6,7,8 similar4,5 or decreased bone mass in comparison to healthy control subjects.3 Although BMD measurements of femur neck and lumbar (L2-L4) spines were lower in study group. We couldn't find significant differences between study and control group. Regarding the effect of glycaemia on BMD, there are some data that depict the relation between glycaemia and BMD. Hyperglycemia induces decreased bone turnover with osteoblast dysfunction and suppresses serum osteocalcin levels.9,10 According to the previous studies that defend a relation between DM and osteoporosis, osteoporosis is more frequent among chronic DM patients, who have retinopathies, neuropathies or vascular disease.11 Kanazawa et al.12 claimed a negative correlation between serum osteocalcin and hemoglobin A1c (HbA1c) levels. Viegas et al.13 found remarkable osteoporosis and vertebral fracture ratios among chronic diabetic postmenopausal women who have retinopathy and renal dysfunction. But there are also some studies that claim no relation between DM and osteoporosis. For example Anaforoglu et al.14 found no relation between type 2 diabetes and osteoporosis among postmenopausal women but a negative correlation between femoral neck BMD and micro albuminuria due to DM. Other studies showed that BMD values of type 2 DM patients were higher than non-diabetic patient's values.15
Although there is no consensus about the effects of hypercholesterolemia on BMD, many authors noticed a negative correlation between hypercholesterolemia and BMD. In vitro studies, it was shown that lipids and lipoprotein oxidation products hampered the functions and differentiation of osteoblasts.16 Low-density lipoproteins (LDL) cholesterol has got direct negative effect on bone metabolism. This negative effect of LDL cholesterol particles is explained by increased catabolism rather than bone production.17,18 Similarly, Poli et al.19 found low BMD among 1303 postmenopausal patients who have high plasma LDL levels. Cui et al.20 reported a negative correlation between LDL levels and lumber BMD values in postmenopausal patients. In another study lumber BMD values found lesser among postmenopausal women who have high serum cholesterol and LDL levels.21 On the other hand Demir et al.22 couldn't find any correlation between cholesterol levels and BMD. In another study it was reported that lipid profile wasn't a unique factor on BMD besides lipids duration of menopause and level of estrogen were also effective on BMD.23
In our study we couldn't find significant differences between diabetic, hyperlipidemic and hypertensive women and control group. There is expediency with literature. In our study we didn't inquire medication among hypertensive and hyperlipidemic patients. In the literature positive effects of antihypertensive and antihyperlipidemic drugs on BMD were reported. Some previous studies reported positive effects of anti-lipid drugs on BMD.24,25,26 In another study Olmos et al.27 reported that thiazide group drugs were effective in increasing BMD in hypertensive patients. The relation between BMD and Cardiovascular Disease risk factors such as hypertension and hyperlipidemia couldn't be clearly defined. In another study, no relation was found between hypertension and BMD.28,29
There are no significant differences between study group and control group in terms of BMD measurements. We found that, accompanying chronic diseases such as diabetes, hypertension and hyperlipidemia don't affect the BMD measurements at postmenopausal period. So these postmenopausal women don't have excess risk regarding osteoporosis.
Figures and Tables
Table 1
Demographic and clinical characteristics of the two groups

Values are expressed as mean ± standard deviation (SD)
*Values are median (minimum-maximum)
ALP: alkaline phosphatase, BMI: body mass index, Ca: calcium, FSH: follicle stimulating hormone, HDL: high-density lipoprotein, LDL: low-density lipoprotein, LH: luteinizing hormone, P: phosphorus, TG: triglycerides, TSKF: T score femoral neck, TSKV: T score lumbar vertebra spine
References
1. Tuominen JT, Impivaara O, Puukka P, Rönnemaa T. Bone mineral density in patients with type 1 and type 2 diabetes. Diabetes Care. 1999; 22:1196–1200.
2. Compston JE, Smith EM, Matthews C, Schofield P. Whole body composition and regional bone mass in women with insulin-dependent diabetes mellitus. Clin Endocrinol (Oxf). 1994; 41:289–293.
3. Nicodemus KK, Folsom AR. Type 1 and type 2 diabetes and incident hip fractures in postmenopausal women. Diabetes Care. 2001; 24:1192–1197.
4. Avery L. Diabetes mellitus types 1 and 2: an voerview. Nurs Stand. 1998; 13:35–38.
5. Sosa M, Dominguez M, Navarro MC, Segarra MC, Hernández D, de Pablos P, et al. Bone mineral metabolism is normal in non-insulin-dependent diabetes mellitus. J Diabetes Complications. 1996; 10:201–205.
6. Johnston CC Jr., Hui SL, Longcope C. Bone mass and sex steroid concentrations in postmenopausal Caucasian diabetics. Metabolism. 1985; 34:544–550.
7. van Daele PL, Stolk RP, Burger H, Algra D, Grobbee DE, Hofman A, et al. Bone density in non-insulin-dependent diabetes mellitus. The Rotterdam Study. Ann Intern Med. 1995; 122:409–414.
8. Stolk RP, Van Daele PL, Pols HA, Burger H, Hofman A, Birkenhager JC, et al. Hyperinsulinemia and bone mineral density in an elderly population: The Rotterdam Study. Bone. 1996; 18:545–549.
9. Gerdhem P, Isaksson A, Akesson K, Obrant KJ. Increased bone density and decreased bone turnover, but no evident alteration of fracture susceptibility in elderly women with diabetes mellitus. Osteoporos Int. 2005; 16:1506–1512.
10. Son GH, Kim JH, Kwon JY, Kim YH, Park YW. Risk factors for cesarean delivery after induction of labor in nulliparous women with an unfavorable cervix at or beyond 41 weeks of gestation. Gynecol Obstet Invest. 2013; 76:254–259.
11. Carnevale V, Romagnoli E, D'Erasmo L, D'Erasmo E. Bone damage in type 2 diabetes mellitus. Nutr Metab Cardiovasc Dis. 2014; 24:1151–1157.
12. Kanazawa I, Yamaguchi T, Sugimoto T. Relationship between bone biochemical markers versus glucose/lipid metabolism and atherosclerosis; a longitudinal study in type 2 diabetes mellitus. Diabetes Res Clin Pract. 2011; 92:393–399.
13. Viegas M, Costa C, Lopes A, Griz L, Medeiro MA, Bandeira F. Prevalence of osteoporosis and vertebral fractures in postmenopausal women with type 2 diabetes mellitus and their relationship with duration of the disease and chronic complications. J Diabetes Complications. 2011; 25:216–221.
14. Anaforoglu I, Nar-Demirer A, Bascil-Tutuncu N, Ertorer ME. Prevalence of osteoporosis and factors affecting bone mineral density among postmenopausal Turkish women with type 2 diabetes. J Diabetes Complications. 2009; 23:12–17.
15. Kao WH, Kammerer CM, Schneider JL, Bauer RL, Mitchell BD. Type 2 diabetes is associated with increased bone mineral density in Mexican-American women. Arch Med Res. 2003; 34:399–406.
16. Sarkis KS, Pinheiro Mde M, Szejnfeld VL, Martini LA. High bone density and bone health. Endocrinol Nutr. 2012; 59:207–214.
17. Parhami F, Garfinkel A, Demer LL. Role of lipids in osteoporosis. Arterioscler Thromb Vasc Biol. 2000; 20:2346–2348.
18. Parhami F, Jackson SM, Tintut Y, Le V, Balucan JP, Territo M, et al. Atherogenic diet and minimally oxidized low density lipoprotein inhibit osteogenic and promote adipogenic differentiation of marrow stromal cells. J Bone Miner Res. 1999; 14:2067–2078.
19. Poli A, Bruschi F, Cesana B, Rossi M, Paoletti R, Crosignani PG. Plasma low-density lipoprotein cholesterol and bone mass densitometry in postmenopausal women. Obstet Gynecol. 2003; 102:922–926.
20. Cui LH, Shin MH, Chung EK, Lee YH, Kweon SS, Park KS, et al. Association between bone mineral densities and serum lipid profiles of pre- and post-menopausal rural women in South Korea. Osteoporos Int. 2005; 16:1975–1981.
21. Makovey J, Chen JS, Hayward C, Williams FM, Sambrook PN. Association between serum cholesterol and bone mineral density. Bone. 2009; 44:208–213.
22. Demir B, Haberal A, Geyik P, Baskan B, Ozturkoglu E, Karacay O, et al. Identification of the risk factors for osteoporosis among postmenopausal women. Maturitas. 2008; 60:253–256.
23. Begic Z, Balic D, Rizvanovic M. The association between lipid profile and bone density in postmenopausal women. Med Arch. 2012; 66:378–381.
24. Lupattelli G, Scarponi AM, Vaudo G, Siepi D, Roscini AR, Gemelli F, et al. Simvastatin increases bone mineral density in hypercholesterolemic postmenopausal women. Metabolism. 2004; 53:744–748.
25. Montagnani A, Gonnelli S, Cepollaro C, Pacini S, Campagna MS, Franci MB, et al. Effect of simvastatin treatment on bone mineral density and bone turnover in hypercholesterolemic postmenopausal women: a 1-year longitudinal study. Bone. 2003; 32:427–433.
26. Uzzan B, Cohen R, Nicolas P, Cucherat M, Perret GY. Effects of statins on bone mineral density: a meta-analysis of clinical studies. Bone. 2007; 40:1581–1587.
27. Olmos JM, Hernández JL, Martínez J, Castillo J, Valero C, Pérez Pajares I, et al. Bone turnover markers and bone mineral density in hypertensive postmenopausal women on treatment. Maturitas. 2010; 65:396–402.
28. Shen C, Deng J, Zhou R, Chen J, Fan S, Li Z, et al. Relation between bone mineral density, bone loss and the risk of cardiovascular disease in a Chinese cohort. Am J Cardiol. 2012; 110:1138–1142.
29. Javed F, Khan SA, Ayers EW, Aziz EF, Akram MS, Nadkarni GN, et al. Association of hypertension and bone mineral density in an elderly African American female population. J Natl Med Assoc. 2012; 104:172–178.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download