Abstract
Ovarian hemangiomas are usually of the cavernous type, and are rarely encountered. A 73-year-old woman presented with lower abdominal discomfort. Subsequent physical examination depicted a palpable mass in the lower abdomen. Abdominopelvic computed tomography (CT) revealed a well-circumscribed mass with thin septa measuring 12.1 × 9.0 cm in the right ovary. Levels of the tumor markers cancer antigen (CA)-125 and CA 19-9 were within the normal range. At laparoscopy, the tumor was found to be confined to the right ovary and to have a smooth surface. The final histopathological result was ovarian cavernous hemangioma. Microscopically, the mass consisted of multiple, dilated, blood-filled vascular channels separated by loose connective tissue, and all were lined by a single layer of flattened endothelium. The authors present a case of ovarian cavernous hemangioma presenting as a large growing mass in a postmenopausal woman and review previously published literature.
Ovarian hemangiomas are rare tumors and are usually found incidentally. In fact, fewer than 5 cases have been reported in the Korean literature and only around 50 cases in the English literature. Sizes of reported hemangiomas vary, and relatively few are large and symptomatic.
Histologic types of ovarian hemangioma include the cavernous and capillary types. However, most ovarian hemangiomas are of the cavernous type and consist of multiple, dilated, blood-filled vascular channels lined by a single layer of endothelium. Occasionally, ovarian hemangiomas are associated with hemangioma of the genital tract or other sites.1 Most patients experience relatively mild symptoms. Unusual manifestations associated with ovarian hemangiomas include thrombocytopenia,1 acute abdomen with ovarian torsion,2 calcification and resultant imaging misinterpretation,2 massive ascites and elevated cancer antigen (CA)-125 mimicking ovarian cancer,34 and hyperestrogenic or hyperandrogenic manifestations.5 Ovarian hemangiomas sometimes coexist with genital tract diseases or even malignancies,67 and thus, ovarian hemangioma can be clinically significant due to these occasional conditions.
Here, we report a case of ovarian cavernous hemangioma which manifested as a large growing mass in a postmenopausal woman, and present a brief review of the literature.
A 73-year-old woman with unremarkable medical and surgical histories presented with lower abdominal discomfort and cervical atypical squamous cells of undetermined significance (ASCUS). Physical examination revealed a palpable mass in the lower abdomen, and abdominopelvic computed tomography (CT) revealed a 12.1 × 9.0 cm sized, well-circumscribed mass, located anterior to the uterus, with thin septa attached to the right ovary (Fig. 1). The mass had been first detected 5 years previously when it was 6.4 cm sized. No ascites and no cutaneous or mucosal hemangioma were present. The patient was not receiving any hormonal medication, and her laboratory findings were normal; levels of the tumor markers CA-125 and CA 19-9 were within their normal ranges. At laparoscopy, the tumor was observed to be confined to the right ovary and to have a smooth purple colored surface. No evidence of torsion was noted, and the uterus, left ovary, and salpinges were unremarkable. The mass was totally resected. Its cut surface showed large cystic spaces, and intraoperative frozen section examination revealed it to be benign. The patient underwent bilateral salpingo-oophorectomy. Cytology results for peritoneal washings were negative for malignancy. Her postoperative recovery was uneventful, and she was discharged 4 days after surgery. Postoperative pathological findings revealed ovarian hemangioma of the cavernous type.
Grossly, the hemangioma weighed 19.1 g and measured 12.0 × 8.0 cm, and was multiloculated and contained blood clots (Fig. 2). Microscopically, it consisted of multiple, dilated, blood filled vascular channels separated by loose connective tissue (Fig. 3A), and all of these vessels were lined by a single layer of flattened endothelium (Fig. 3B). No mitotic activity was noted and no atypical cells were observed. Vascular spaces within the tumor varied in size. No heterotopic tissue elements were present, and the contralateral ovary and both tubes were unremarkable.
Hemangioma of the ovary is rare despite the rich, complex ovarian vasculature.8 The majority are small, unilateral, and asymptomatic. However, large tumors present with symptoms, such as, swelling with ascites and abdominal pain, due to the mass per se or torsion. Ovarian hemangioma is mostly encountered incidentally at operation or autopsy. They may occur concomitantly with hemangiomas in the genital tract or other sites, and may cause abdominal and pelvic symptoms. Mass sizes range from 0.3 to 24 cm, and patient ages range from 4 months to 81 years, without no evidence of predominance in any age group.9
The etiology of ovarian hemangioma is controversial. Some have proposed that its pathogenesis may be stimulated by infection or hormones.3 They also constitute portions of mature teratomas or hamartomatous malformations.10 They would appear a failure of vascular formation, particularly of the canalizing process, results in the formation of abnormal vascular channels.8 Histologically, ovarian hemangiomas may be of the cavernous or capillary type, but the cavernous type is the most common. These types are differentiated by the sizes of blood vessels within tumors, that is, the capillary type consists of vessels of normal caliber, whereas the cavernous type contains larger vascular channels.
The most common locations of ovarian hemangioma are the medulla and hilar regions, which usually have larger vascular channels, and thus, ovarian hemangioma should be differentiated from proliferations of dilated blood vessels in ovarian hilum. These hemangiomas can be distinguished from hilar vascular proliferations when a circumscribed nodule or a mass is observed.11 Our case presented a well demarcated mass consisting of dilated vessels throughout the whole cystic lesion, which suggested ovarian hemangioma.
Clinical issues related to ovarian hemangioma are uncommon, but various, and include acute abdomen with ovarian torsion, calcification, massive ascites, co-occurrence with genital tract diseases, and hormonal manifestations (Table 1). Several cases of acute abdomen in patients with a twisted ovarian hemangioma sized from 6 to 18 cm,8 and several cases of calcified ovarian hemangioma have been reported.1213 Ovarian hemangioma should also be included in the differential diagnosis of adnexal masses with calcification. Unusual presentations including massive ascites and elevated CA-125 mimicking ovarian cancer have been reported.314 Kaneta et al.4 described a case of ovarian hemangioma with massive ascites, pleural effusion, and elevated serum CA-125 suggesting pseudo-Meigs' syndrome. The cause of the association between ovarian hemangioma and massive ascites has not been definitively identified, although vascular disturbance caused by hemangioma is a possible cause.15 Although highly unusual, ovarian hemangioma should be considered in the differential diagnosis of patients with ascites and elevated CA-125, for example, Akbulut et al.6 reported an ovarian hemangioma occurring synchronously with serous papillary carcinoma of the ovary.
In the majority of cases, ovarian hemangiomas are nonfunctional neoplasms, but functioning ovarian stroma containing luteinized stromal cells may result in hormonal effects. These cells produce androgen, which is subsequently converted to estrone in adipose tissue and finally causes unopposed estrogenic stimulation in endometrium. A few cases of ovarian hemangioma-induced endometrial stimulation have been reported. Endometrial hyperplasia or endometrial carcinoma associated with ovarian hemangiomas was reported.57 Shitsukawa et al.16 presented a case of ovarian hemangioma characterized by male pattern baldness and an elevated testosterone level.
Debate continues on the pathogenesis of ovarian hemangioma and its association with hormonal disorders. Carder et al.7 suggested preexisting stromal luteinization of ovaries might stimulate the development of ovarian hemangioma.
Imaging findings characteristic of cavernous ovarian hemangioma have been suggested. Yamawaki et al.15 described the CT and magnetic resonance imaging (MRI) findings of cavernous ovarian hemangioma. CT showed a complex mass with cystic and solid components, MRI showed a marked enhancement pattern on contrast-enhanced T1 weighted images. Although nonspecific, these findings are suggestive of ovarian hemangiomas. However, our case differs from previously reported cases, as CT did not visualize the pattern of characteristic hemangioma. It is possible MRI might help differentiate hemangioma and other tumors, but MRI was not performed in our case
In summary, we report a cavernous ovarian hemangioma that manifested as a large growing mass in a postmenopausal woman. Although the presence of ovarian hemangioma could not accurately predicted by preoperative CT, hemangioma should be considered in the differential diagnosis when a growing adnexal mass or a hemorrhagic ovarian lesion (Fig. 2) is encountered in postmenopausal women.
Figures and Tables
Fig. 1
(A) Contrast enhanced computed tomography (CT) image showing a 6.4 cm, well-defined, thin-walled cyst with thin septa in the right ovary. (B) Follow-up CT image obtained 5 years later showing an increase in mass size to a maximal diameter of 12.1 cm.
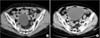
Fig. 2
Gross findings of the ovarian mass. The multiloculated cystic lesion contained occasional blood clots (▸). The remnant ovary is also seen in left lower part (arrow).

References
1. Lawhead RA, Copeland LJ, Edwards CL. Bilateral ovarian hemangiomas associated with diffuse abdominopelvic hemangiomatosis. Obstet Gynecol. 1985; 65:597–599.
2. Kim MY, Rha SE, Oh SN, Lee YJ, Jung ES, Byun JY. Case report: Ovarian cavernous haemangioma presenting as a heavily calcified adnexal mass. Br J Radiol. 2008; 81:e269–e271.
3. Erdemoglu E, Kamaci M, Ozen S, Sahin HG, Kolusari A. Ovarian hemangioma with elevated CA125 and ascites mimicking ovarian cancer. Eur J Gynaecol Oncol. 2006; 27:195–196.
4. Kaneta Y, Nishino R, Asaoka K, Toyoshima K, Ito K, Kitai H. Ovarian hemangioma presenting as pseudo-Meigs' syndrome with elevated CA125. J Obstet Gynaecol Res. 2003; 29:132–135.
5. Gücer F, Ozyilmaz F, Balkanli-Kaplan P, Mlayim N, Aydin O. Ovarian hemangioma presenting with hyperandrogenism and endometrial cancer: a case report. Gynecol Oncol. 2004; 94:821–824.
6. Akbulut M, Bir F, Colakoğlu N, Soysal ME, Düzcan SE. Ovarian hemangioma occurring synchronously with serous papillary carcinoma of the ovary and benign endometrial polyp. Ann Saudi Med. 2008; 28:128–131.
7. Carder PJ, Gouldesbrough DR. Ovarian haemangiomas and stromal luteinization. Histopathology. 1995; 26:585–586.
8. Uppal S, Heller DS, Majmudar B. Ovarian hemangioma--report of three cases and review of the literature. Arch Gynecol Obstet. 2004; 270:1–5.
9. Prat J. Pathology of the ovary. Philadelphia, PA: Saunders;2004.
10. Itoh H, Wada T, Michikata K, Sato Y, Seguchi T, Akiyama Y, et al. Ovarian teratoma showing a predominant hemangiomatous element with stromal luteinization: report of a case and review of the literature. Pathol Int. 2004; 54:279–283.
11. Talerman A. Nonspecific tumors of the ovary, including mesenchymal tumors and malignant lymphoma. In : Kurman RJ, editor. Blaustein's pathology of the female genital tract. 5th ed. New York, NY: Springer;1987. p. 1035–1062.
12. Lee Y. Calcified cavernous hemangioma of the ovary: a case report. J Korean Radiol Soc. 2000; 43:751–754.
13. Park CH. Cavernous hemangioma of the ovary. Korean J Obstet Gynecol. 2000; 43:1302–1307.
14. Gehrig PA, Fowler WC Jr, Lininger RA. Ovarian capillary hemangioma presenting as an adnexal mass with massive ascites and elevated CA-125. Gynecol Oncol. 2000; 76:130–132.
15. Yamawaki T, Hirai Y, Takeshima N, Hasumi K. Ovarian hemangioma associated with concomitant stromal luteinization and ascites. Gynecol Oncol. 1996; 61:438–441.
16. Shitsukawa K, Shinomiya S, Tanaka Y, Okada M, Kamada M. Ovarian haemangioma with hyperandrogenism: a case report. J Obstet Gynaecol. 2015; 35:214–215.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download