Abstract
Objectives
This study was conducted to examine the effects of hormone therapy on serum lipid levels in postmenopausal Korean women.
Methods
This retrospective cohort study included 154 healthy postmenopausal Korean women. Seventy-nine women took oral estrogen (conjugated equine estrogen 0.625 mg/day or equivalent), and 75 applied estrogen transdermally using 0.1% 17β-estradiol gel. Micronized progesterone (MP) was added to 40 women of oral group and 49 women in transdermal group. Serum levels of triglyceride, low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C), and lipoprotein (a) were measured before, 3 and 6 month after hormone therapy.
Results
At baseline, mean body mass index (BMI) were lower (22.76 vs. 23.74 kg/m2) and proportion of family history of cardiovascular disease (CVD) (61 vs. 39%) were higher in oral group. In oral group, LDL-C and lipoprotein(a) levels decreased, and triglyceride and HDL-C levels increased significantly after 3 and 6 months. There was no significant change in lipoprotein levels compared to the baseline in transdermal group. There were also no differences with additional MP. Changing pattern of HDL-C during 6 months was significantly different by the route of estrogen administration.
Cardiovascular disease (CVD) causes about one-third of all deaths for women worldwide,12 and develops about 7 to 10 years later in women than men on average. The number of cardiovascular deaths for women increases after menopause.23 Menopause accompanies unfavorable changes in serum lipoprotein concentrations because of a decrease in serum estrogen level.4567 Postmenopausal estrogen therapy has favorable effects on serum lipid, and has contributed to a decrease in the risk of CVD by 25% to 50%8 and prevention of death by 50%.89 Serum levels of total cholesterol, low-density lipoprotein (LDL) and lipoprotein(a) were reduced, while serum levels of high-density lipoprotein (HDL) and triglyceride were increased after oral administration of estrogen.10 On the contrary, serum levels of total cholesterol, LDL and lipoprotein(a) were reduced, while serum levels of HDL and triglyceride remained the same after transdermal administration of estrogen.111213 With combined use of estrogen therapy, progestogens had different effects on HDL cholesterol depending on different types.1415 Although medroxyprogesterone acetate inhibits the effect of estrogen, micronized progesterone (MP) does not interfere with the increase of HDL level.15 However, since most previous studies were done on Western women, only a limited number of studies have investigated serum lipoprotein cholesterol according to the route of estrogen administration and a combination of progesterone with estrogen in Korean women. This study was conducted to examine the effects of oral and thermal estrogen therapies on serum lipid levels and change of lipid profile of additionally administered MP in postmenopausal Korean women.
This retrospective study included 154 healthy postmenopausal Korean women who underwent hormone replacement therapy in the Menopause Clinic, Department of Obstetrics and Gynecology, Samsung Medical Center from April 1994 to December 2013. Menopause is defined as the cessation of menstruation for more than a year or serum follicle stimulating hormone (FSH) levels of 40 IU/L or higher. We excluded subjects taking any medication that can influence lipid profile or those with past history of CVD or risk factors of CVD (hypertension, diabetes mellitus, smoking and others). As hormone therapy, 65 women without a uterus were given estrogen alone (oral: 39, non-oral: 6), and 89 women were given estrogen in combination with MP (oral estrogen: 40, non-oral: 49). Conjugated equine estrogen 0.625 mg/day or equivalent medication were administered as oral estrogen, while 0.1% 17β-estradiol gel 1.5 mg/day was applied to the forearm as non-oral estrogen.
Serum levels of triglyceride, HDL and LDL cholesterol and lipoprotein (a) were measured after 14 hours of fasting on an empty stomach, and their changes were compared before, 3 and 6 months after hormone therapy. All statistical analyses were done using SPSS version 21.0 for windows (SPSS Inc., Chicago, IL, USA), and the data were presented as the mean ± standard deviation (SD). Statistical difference between two groups was compared with two-tailed unpaired student t-tests, chi-square analysis, and two-tailed paired student t tests. P values of less than 0.05 were considered statistically significant.
Table 1 shows the baseline characteristics of estrogen alone and combined estrogen-progesterone therapy groups with oral hormone administration. Menopausal age was significantly older in the combined estrogen-progesterone therapy group. According to the analysis of lipid changes during 6 months, single administration of estrogen significantly decreased LDL and lipoprotein (a) levels and significantly increased triglyceride and HDL levels (Table 2). With combined administration of MP, serum cholesterol levels, excluding lipoprotein (a), showed same changes as single administration of estrogen. After adjusting menopausal age, changing pattern in serum cholesterol had no difference between two groups. Due to the nature of baseline characteristics of estrogen alone and combined estrogen-progesterone therapy groups with transdermal route of administration, menopausal age was significantly older in combined therapy group (Table 3). No significant change was observed in estrogen alone and combined therapy groups (Table 4).
Considering that combined use of MP did not influence the effect of estrogen on lipid profile based the above findings regardless of routes of hormone administration, a comparative analysis was performed by the route of estrogen administration by combining estrogen alone and combined estrogen-progesterone therapy groups. Although no difference was found in menopausal age between two groups, body mass index (BMI) was lower in oral administration group compared with transdermal administration group. In addition, a family history of CVD was more commonly noted in oral administration group (Table 5).
Table 6 shows the comparison of serum cholesterol levels in whole hormone therapy group by the route of estrogen. A significant decrease was found in LDL and lipoprotein (a) levels and a significant increase was detected in triglyceride and HDL levels compared to the baseline levels in oral administration group. On the other hand, no significant change was observed in lipoprotein levels in transdermal administration group. After adjusting BMI and a family history of CVD, changing pattern of HDL was significantly different between two groups by administration route (Fig. 1).
LDL cholesterol and lipoprotein (a) levels dropped and HDL and triglyceride levels increased significantly in oral administration group after 6-month hormone therapy. In contrast, no significant change was observed in transdermal administration group. In comparison of changes in lipoproteins during 6-month hormone therapy by administration route, changing pattern of HDL cholesterol was significantly different between two groups. This result is meaningful considering the fact that HDL is more important predictor of CVD than LDL in women.316 Several previous studies have verified that estrogen administration has beneficial effects on serum lipid profile and cardiovascular protective effects in postmenopausal women.891718 The effects of estrogen on serum lipid profile are affected by administration route or addition of progesterone.19 Oral estrogens are most commonly used modality, and their bioavailability is reduced, changes in serum estrogen levels are relatively large and there is the risk of side effects due to formation of by-products during gastrointestinal absorption and metabolism in the liver.20 Since transdermal estrogen not metabolized in the liver flows into the blood vessels via passive diffusion through the skin, postmenopausal symptoms can be managed at a relatively low dose. However, transdermal estrogens have less impact on the lipid profile than oral estrogens.21 According to the results of previous studies, oral estrogens have been shown to beneficially affect serum lipid profile by reducing LDL level and increasing HDL level, but may elevate serum triglyceride level. On the contrary, transdermal estrogens have less impact on lipoproteins compared to oral estrogens.
Even though the results of this study on the effects of oral administration are comparable to those of Western studies, a difference was found in the findings of previous studies that showed reduced LDL and elevated HDL levels after transdermal administration. This is thought to be attributable to racial differences in estrogen action.2223 The administration of oral estrogens might be more beneficial than transdermal hormone therapy in terms of serum lipid profile in postmenopausal Korean women.
MP co-administered with estrogen had no significant influence on estrogenic activity. Unlike medroxyprogesterone acetate, the study results aligned with the outcomes of previous studies that a significant increase of serum HDL level was maintained.1524 The combined use of MP is expected to be beneficial to endometrial protection in postmenopausal women with a uterus without attenuating the favorable effects of estrogen on serum lipid profile.
This study was meaningful in that it analyzed the effects on oral and transdermal hormone therapies on serum lipid profile in postmenopausal Korean women and the difference between with and without progesterone. This investigation was limited by the relatively small sample size as a retrospective study and a relatively short follow-up period of 6 months.
To sum up the above study result, hormone replacement therapy using oral estrogens clearly exerts favorable effects on lipoprotein metabolism in postmenopausal women. Moreover, the addition of MP does not attenuate these favorable effects of estrogen on serum lipid metabolism. Further studies with larger population samples of women are warranted.
Figures and Tables
Fig. 1
Change in high-density lipoprotein (HDL) cholesterol in whole hormone therapy group by the route of estrogen. After adjusting for body mass index and family history of cardiovascular disease, changing pattern of HDL was significantly different between the two groups (P = 0.028). TD: transdermal.
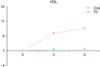
Table 2
Comparison of serum cholesterol levels in oral hormone therapy group by progesterone, adjusted by menopausal age

Table 4
Comparison of serum cholesterol levels in transdermal hormone therapy group by progesterone, adjusted by menopausal age

Acknowledgement
This work was supported in part by the Samsung Medical Center Research Fund, (PH01991081, PHX1000311, and PHO1133361) and the IN-SUNG Foundation for Medical Research (C-A5-811-1).
References
1. Mosca L, Banka CL, Benjamin EJ, Berra K, Bushnell C, Dolor RJ, et al. Evidence-based guidelines for cardiovascular disease prevention in women: 2007 update. J Am Coll Cardiol. 2007; 49:1230–1250.
2. Lloyd-Jones DM, Leip EP, Larson MG, D'Agostino RB, Beiser A, Wilson PW, et al. Prediction of lifetime risk for cardiovascular disease by risk factor burden at 50 years of age. Circulation. 2006; 113:791–798.
3. Bush TL. Evidence for primary and secondary prevention of coronary artery disease in women taking oestrogen replacement therapy. Eur Heart J. 1996; 17:Suppl D. 9–14.
4. Lee KS, Roh JS, Kim JG, Kim SH, Choi YM, Shin CJ, et al. The effect of ipriflavone on serum lipid profiles in postmenopausal women. J Korean Soc Menopause. 1996; 2:27–35.
5. Heo J, Park Y, Park HM. Dietary intake of nutrients and food in postmenopausal Korean women. J Korean Soc Menopause. 2011; 17:12–20.
6. Kwon OS, Kim JH, Cho SH, Park HM, Sung EJ. The association between subclinical hypothyroidism and cardiovascular risk factors in post-menopausal women. J Korean Soc Menopause. 2012; 18:193–198.
7. Lee SR, Cho SB, Jeong KA. Serum lipid profiles and thyroid function tests in elderly women. J Korean Soc Menopause. 2009; 15:186–192.
8. Barrett-Connor E, Bush TL. Estrogen and coronary heart disease in women. JAMA. 1991; 265:1861–1867.
9. Stampfer MJ, Colditz GA. Estrogen replacement therapy and coronary heart disease: a quantitative assessment of the epidemiologic evidence. Prev Med. 1991; 20:47–63.
10. Soma MR, Osnago-Gadda I, Paoletti R, Fumagalli R, Morrisett JD, Meschia M, et al. The lowering of lipoprotein[a] induced by estrogen plus progesterone replacement therapy in postmenopausal women. Arch Intern Med. 1993; 153:1462–1468.
11. Crook D, Stevenson JC. Transdermal hormone replacement therapy, serum lipids and lipoproteins. Br J Clin Pract Suppl. 1996; 86:17–21.
12. Jensen J, Riis BJ, Strøm V, Nilas L, Christiansen C. Long-term effects of percutaneous estrogens and oral progesterone on serum lipoproteins in postmenopausal women. Am J Obstet Gynecol. 1987; 156:66–71.
13. Meschia M, Bruschi F, Soma M, Amicarelli F, Paoletti R, Crosignani P. Effects of oral and transdermal hormone replacement therapy on lipoprotein(A) and lipids: a randomized controlled trial. Menopause. 1998; 5:157–162.
14. Rosano GM, Fini M. Comparative cardiovascular effects of different progestins in menopause. Int J Fertil Womens Med. 2001; 46:248–256.
15. The Writing Group for the PEPI Trial. Effects of estrogen or estrogen/progestin regimens on heart disease risk factors in postmenopausal women. The Postmenopausal Estrogen/Progestin Interventions (PEPI) Trial. The Writing Group for the PEPI Trial. JAMA. 1995; 273:199–208.
16. Jacobs DR Jr, Mebane IL, Bangdiwala SI, Criqui MH, Tyroler HA. , Mebane IL, Bangdiwala SI, Criqui MH, Tyroler HA. High density lipoprotein cholesterol as a predictor of cardiovascular disease mortality in men and women: the follow-up study of the Lipid Research Clinics Prevalence Study. Am J Epidemiol. 1990; 131:32–47.
17. Stampfer MJ, Colditz GA, Willett WC, Manson JE, Rosner B, Speizer FE, et al. Postmenopausal estrogen therapy and cardiovascular disease. Ten-year follow-up from the nurses' health study. N Engl J Med. 1991; 325:756–762.
18. Jeon GH, Cho HJ, Chun S, Ji YI, Jeong CH, Suh MH, et al. The occurrence of glaucoma and association with serum estradiol level in postmenopausal women. J Korean Soc Menopause. 2013; 19:106–111.
19. Namkung J, Kim JH, Jo HH, Oh EK, Cheon K, Kwon DJ, et al. Comparison of the effects of hormone replacement therapy on bone mineral density, lipid profiles, and biochemical markers of bone metabolism. J Korean Soc Menopause. 2010; 16:107–115.
20. Karjalainen A, Heikkinen J, Savolainen MJ, Bäckström AC, Salinto M, Kesäniemi YA. Metabolic changes induced by peroral oestrogen and transdermal oestradiol gel therapy. Br J Obstet Gynaecol. 1997; 104:Suppl 16. 38–43.
21. Padwick ML, Endacott J, Whitehead MI. Efficacy, acceptability, and metabolic effects of transdermal estradiol in the management of postmenopausal women. Am J Obstet Gynecol. 1985; 152:1085–1091.
22. Kim HJ, Oh YK, Lee JS, Lee DY, Choi D, Yoon BK. Effect of transdermal estrogen therapy on bone mineral density in postmenopausal korean women. J Menopausal Med. 2014; 20:111–117.
23. Vora AN, Ouyang P, Bittner V, Tardif JC, Waters DD, Vaidya D. Racial differences of lipoprotein subclass distributions in postmenopausal women. Ethn Dis. 2008; 18:176–180.
24. Espeland MA, Marcovina SM, Miller V, Wood PD, Wasilauskas C, Sherwin R, et al. Effect of postmenopausal hormone therapy on lipoprotein (a) concentration. PEPI Investigators. Postmenopausal Estrogen/Progestin Interventions. Circulation. 1998; 97:979–986.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download