Abstract
Objectives
To evaluate the prevalence of premenstrual syndrome (PMS) and premenstrual dysphoric disorder (PMDD) of perimenopausal women at a university hospital along with their menstrual characters.
Methods
A questionnaire survey regarding premenstrual symptoms was carried out in 100 perimenopausal women (43 to 53, years). The pattern of menstruation and, the intensity of dysmenorrhea were assessed; and further, the symptoms were classified according to their number, intensity, and persistence. The PMS criteria of American College of Obstetrics and Gynecology (ACOG) and PMDD criteria by American Psychiatric Association (APA) were evaluated.
Results
The approximate prevalence of PMS criteria was 95% and that of PMDD criteria was 23%. The most dominant symptoms were 'breast tenderness', 'abdominal bloating', 'and headache'. PMDD was significantly associated with the severity of dysmenorrhea (P = 0.020). There was no significant relation with age, height, weight, body mass index and the cycle of menstruation.
Menstruation is a physiological phenomenon experienced by women, many of whom report premenstrual symptoms such as breast tenderness, abdominal bloating, nausea, and headache. These symptoms are usually mild and do not require special treatment in most cases; however, 20-40% of women experience severe premenstrual symptoms that cause disability.1 These severe symptoms, known as premenstrual syndrome (PMS), include physical symptoms as well as a variety of emotional symptoms, including depression, anxiety, poor concentration, and irritability. The emotional symptoms of PMS, which cause severe daily disability in 4-14% of women, are categorized as premenstrual dysphoric disorder (PMDD).2 The symptoms of PMDD persist for 5-7 days before the start of menstruation and are usually relieved when menstruation begins, although the degree varies among individuals.3 The American Psychiatric Association (APA) has recommended diagnostic criteria and aggressive treatment for severe PMS. In 1987, the diagnostic and statistical manual of mental disorders, third edition (DSM-III) defined late luteal phase dysphoric disorder (LLPDD),4 followed in 1994 by newly proposed criteria for PMDD or severe PMS in the DSM-IV.5
The first report of premenstrual tension was published in 1931 by Frank. Subsequently, the United States Institute of Obstetrics and Gynecology (American College of Obstetrics and Gynecology, ACOG) identified PMS as ten physical and emotional premenstrual symptoms occurring on one or more of the five days before menstruation, appearing in the previous three menstrual cycles, and dissipating within four days after the start of menstruation or at least thirteen days before the next menstrual cycle.
Women of all ages are increasingly participating in society, leading to an increased stress burden and additional housework. In women with PMS, additional work and stress during menstruation can cause symptoms characteristic of the menopausal transition period. In this study, we analyzed the prevalence of PMS in women who were experiencing symptoms related to the menopausal transition period.
This study included 100 perimenopausal women who had visited a university hospital within 6 months from October 2013 to March 2014 and completed a questionnaire survey regarding premenstrual symptoms after providing informed consent. The questionnaire contained basic information about age, height, and weight, and multiple-choice questions regarding the ten ACOG diagnostic criteria for PMS. Additional questions included information pertaining to menstrual regularity (cycle regularity), the duration of menstruation (cycle duration), menstrual quantity (amount of flow), menstrual cycle, menstrual pain severity, analgesic use, and visits to an obstetrician/gynecologist. The questionnaires also included screening questions regarding PMDD and describing the presence of somatic premenstrual symptoms (breast tenderness, abdominal bloating, headache, and swelling of the extremities), emotional premenstrual symptoms (depression, angry outbursts, irritability, confusion, and anxiety), and quality of life. ACOG and APA guidelines recommend that patients be prospectively evaluated at least twice before PMS and PMDD can be diagnosed; however, due to practical limitations, an accurate diagnosis of these disorders was not possible at the time the survey was administered.
The results of this study were analyzed using SPSS software version 18.0 (SPSS Inc., Chicago, IL, USA). Comparisons of the mean were performed using Student's t-tests, while comparisons of fractions were made using χ2 tests. A multiple response analysis was used for multiple responses. In all cases, P < 0.05 was considered to be statistically significant.
The average age of the respondents was 47.92 ± 1.89 years (range, 43-53 years), the average height was 1.57 ± 0.52 m, the average body weight was 55.8 ± 7.8 kg, and the mean body mass index (BMI) was 22.406 ± 2.867 kg/m2. A regular menstrual cycle was reported for 92 patients, with an average duration of 5.2 ± 1.2 days. There were 16 women who did not report experiencing dysmenorrhea, and 84 women who reported dysmenorrhea on a visual analog scale of 3.0 ± 2.4 out of 10 points. Analgesics to relieve menstrual pain were taken by 33 out of the 100 women in the study (33%) and 16 women visited the obstetrician/gynecologist for dysmenorrhea (Table 1).
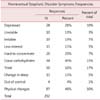
The ACOG has identified ten of the most common symptoms of PMS. In our study 'breast tenderness' was the most common (n = 56), followed by 'abdominal bloating' and 'headache' (n = 36). Reports of 'depression' (n = 28) and 'hands and feet are swelling' (n = 12) were low in the patient cohort. For the 100 women who were selected for this study, the average number of individual symptoms was 2.84 ± 2.02. The most common symptoms associated with PMDD were reported to be 'angry outbursts' (n = 33), and other symptoms of 'anxiety' (n = 22) (Table 2, 3).
Symptoms of PMS persisted for 3.1 ± 3.0 days in the patients in this study; 13 women reported that PMS affected their social activities and daily life (Table 2C).
Based on ACOG diagnostic criteria, 95 of the 100 women (95%) included in this study suffered from PMS. However, emotional and physical symptoms during the menstrual cycle that presented three times before the investigation could not be used to establish a reliable diagnosis. Based on APA diagnostic criteria for PMDD, PMDD was suspected in 23 (23%) of the women in this study. There was a significant difference in the visual analog scale for dysmenorrhea between the PMDD and non-PMDD groups, but no differences in age, weight, BMI, cycle regularity, cycle duration, or amount of flow (Table 4).
PMS symptoms are encountered repeatedly during the luteal phase of the menstrual cycle, causing adverse effects on daily life and work productivity. More than 200 PMS symptoms have been reported in the literature, and most women of childbearing age experience at least one PMS symptom, although in the vast majority medical or psychiatric treatment is not required.6 A dual diagnosis that requires medical and psychiatric treatment of PMS accounts for a small percentage of PMS cases, although the definition and diagnostic criteria for PMS do not reflect the prevalence of PMS in the literature. Based on International Classification of Diseases, Tenth Revision (ICD-10) diagnostic criteria, the incidence of PMS is ~20-30%,7 whereas it is estimated that 3-8% of women have PMDD according to APA guidelines.8 In comparison, Park et al.9,10 reported that among 200 Korean women of childbearing age the prevalence of PMDD was ~8%.
The purpose of this study was to investigate the extent and severity of menopausal transition symptoms in women who visited our university hospital. The ACOG reported that most women suffer from PMS, while the APA estimated that 23% of women suffer from PMDD. A recent survey of working women by Kim et al.11 indicated that the prevalence of PMS in women of childbearing age was higher than previously reported.
The etiology of PMS includes hormone imbalances, Na+ retention, dietary factors such as vitamin deficiency, estrogen and progesterone imbalances, normal ovarian function, neurotransmitter imbalances, and other biological, psychological, and social psychological theories. This suggests that PMS is a multifactorial neuropsychological-endocrine disorder, although a definitive conclusion has not been reached.12,13 Further study regarding the causes of PMS, including eating habits and hormonal tests, are necessary and should include an analysis of multiple factors.
Approaches for PMS treatment have been developed in various fields. Symptom relief has been demonstrated with regular exercise, self-care, and a well-balanced healthy diet. In addition, the education of patients, families, and friends and application of methods for reducing stress and increasing social support are important. While this approach is not primarily for the specific treatment of PMS, it does aid in supporting the overall health of the patient. Drug treatment with oral contraceptive pills, prostaglandin inhibitors, and spironolactone has also been used,2 although medication should not be a first-line treatment.
Women increasingly experience physical and mental stress as they enter the workplace and deal with social stressors. Women who work have a higher prevalence of PMS compared to women who do not, and the incidence of PMS among middle-aged women compared to adolescents has not been determined. It is difficult to generalize to an entire population based on a small sample size. However, it is likely that symptoms of PMS in young women persist during the menopausal transition. Those women who experience PMS and PMDD often struggle with serious social and family issues. Future studies will require a large sample size and generalized criteria for PMS and PMDD to verify the results of this study.
In this study, the prevalence of PMS was similar in perimenopausal women compared to younger women, and PMS and PMDD were diagnosed in all of the subjects regardless of age. Continued education and outreach are required to provide an accurate perception of PMS, and the implementation of effective medical treatments to improve the quality of life for patients and maximize business efficiency will be helpful in the future.
Figures and Tables
References
1. Reid RL. Premenstrual syndrome. N Engl J Med. 1991; 324:1208–1210.
2. Taylor D. Perimenstrual symptoms and syndromes: guidelines for symptom management and self care. Johns Hopkins Adv Stud Med. 2005; 5:228–241.
3. Reid RL, Yen SS. The premenstrual syndrome. Clin Obstet Gynecol. 1983; 26:710–718.
4. American Psychiatric Association. DSM III: Diagnostic and statistical manual of mental disorders. 3rd ed. Washington, DC: American Psychiatric Association;1987.
5. American Psychiatric Association. DSM IV: Diagnostic and statistical manual of mental disorders. 4th ed. Washington, DC: American Psychiatric Association;1994.
6. Sveindóttir H, Bäckström T. Prevalence of menstrual cycle symptom cyclicity and premenstrual dysphoric disorder in a random sample of women using and not using oral contraceptives. Acta Obstet Gynecol Scand. 2000; 79:405–413.
7. Janca A, Hiller W. ICD-10 checklists-a tool for clinicians' use of the ICD-10 classification of mental and behavioral disorders. Compr Psychiatry. 1996; 37:180–187.
8. Yonkers KA, O'Brien PM, Eriksson E. Premenstrual syndrome. Lancet. 2008; 371:1200–1210.
9. Park HE, Jee BC, Ku SY, Suh CS, Kim SH, Choi YM, et al. A survey on premenstrual syndrome. Korean J Obstet Gynecol. 2005; 48:401–410.
10. Park J, Kim TH, Lee HH, Lee W, Chung SH. Premenstrual syndrome in the nursing women working in a university hospital. J Reprod Endocrinol. 2012; 4:36–42.
11. Kim TH, Park HS, Lee HH, Chung SH. Premenstrual syndrome and dysmenorrhea in the career women at Bucheon City. Korean J Obstet Gynecol. 2011; 54:523–528.
12. Halbreich U, Borenstein J, Pearlstein T, Kahn LS. The prevalence, impairment, impact, and burden of premenstrual dysphoric disorder (PMS/PMDD). Psychoneuroendocrinology. 2003; 28:Suppl 3. 1–23.
13. Halbreich U, Backstrom T, Eriksson E, O'Brien S, Calil H, Ceskova E, et al. Clinical diagnostic criteria for premenstrual syndrome and guidelines for their quantification for research studies. Gynecol Endocrinol. 2007; 23:123–130.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download