Abstract
Primary vaginal cancer combined with uterine prolapse is very rare. We present a case of 80-year-old postmenopausal women complaints of something coming out per vagina for the past 20 years, along with blood stained discharge, foul odor leukorrhea, and severe pelvic pain for the last 3 months. A 4 × 5 cm ulcer was present on middle third of vaginal wall with marked edema and ulceration of surrounding tissue. The prolapse was reduced under intravenous sedation in operating room. On gynecologic examination, uterus was normal in size, no adnexal mass was examined, and both parametrium were thickened. Papanicolaou smear was normal. Biopsy of the ulcer at vaginal wall revealed invasive squamous cell carcinoma of vagina. Magnetic Resonance Imaging of abdomen and pelvis showed left hydronephrosis and liver metastasis. Positron emission tomography (PET)/computed tomography (CT) revealed metastasis to lung, liver and iliac bone. She died from progression of disease one month after diagnosis.
Primary vaginal cancer is a rare condition, constituting 1-2% of all gynecologic malignancies. It usually occurs in patients over 60 years of age.1,2 It is commonly located in the posterior upper third of the vagina, and its common histological type is epidermoid carcinoma.1~4 The most frequent clinical symptom is vaginal bleeding, but dysuria and pelvic pain are also common.4 Unfortunately, the treatment of vaginal cancer is not yet completely defined, though a wide variety of treatment options is available depending on the degree of tumor infiltration and prognosis factors. Conservative treatment is effective for precancerous lesions, surgical therapy for early stage of infiltrating cancer, and radiotherapy for progression lesion.4 Although there have been a handful of international reports on uterine prolapse combined with vaginal cancer, there has been none so far domestically. With a review of related literature, we report a case of a patient presented to our hospital with uterine prolapse combined with vaginal cancer.
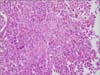
An 80-year-old patient (gravida 7, para 7) was referred from a secondary care hospital with third degree uterine prolapse and a non-healing ulcer of vagina. She had a prolapsed uterus of third degree for 20 years, vaginal bleeding for 3 months with a foul odor and severe pelvic pain. Physical examination revealed a third-degree prolapsed uterus with second-degree cystocele and rectocele. An ill-defined ulcer of 4 × 5 cm in size was present in the middle third of vaginal wall with marked edema and ulceration of surrounding tissue. Ulcer was 5 cm away from the cervix. On a bimanual examination, uterus was normal in size, mobile with free adnexa. Colposcopy was found satisfactory. It revealed coarse mosaic pattern on vaginal ulcer margin on application of 5% acetic acid, but the cervix appeared normal. Biopsy was taken from the ulcerated vaginal lesion. Histopathology showed squamous cell carcinoma of the vagina (Fig. 1). Her hemoglobin concentration dropped to 6.2 g per liter and creatinine level was elevated to 5.41 mg per liter. Magnetic resonance imaging (MRI) of the abdomen and pelvis indicated left hydronephrosis and multiple liver metastasis (Fig. 2). Positron emission tomography (PET) scan showed the multiple metastasis at lung, liver and iliac bone (Fig. 3). A diagnosis of Stage IVb primary carcinoma of vagina with third degree uterovaginal prolapse with cystocele and rectocele was made. Palliative chemotherapy was planned but the patient's performance status was not fit to undergo the treatment because blood urea nitrogen (BUN) and creatinine levels increased. After a month, the patient expired from a worsening uremia.
Even among diseases that occur after menopause, vaginal cancer is very rare.5 The appropriate diagnosis of vaginal cancer begins with the exclusion of other coexistent gynecologic cancers. Moreover, for patients with a history of gynecologic cancers, it requires no recurrence for the past 5 years. If vaginal lesions are connected to the cervix or vulva, it is primarily diagnosed as either cervical cancer or vulvar cancer. The choice of treatments for vaginal cancer is determined by the prognosis factors, which include the lesion's size, location, and degree of infiltration, age, clinical stage and histology. The most preferred treatment is radiotherapy. Size and location of the lesion must be well established to determine the dose and type of radiation therapy. Lesions located in the lower region of the vagina wall at clinical Stage I are treated with a combination of external beam and intracavitary radiation therapy. On the other hand, the same lesions located in the upper region are treated with a similar dose of radiation and therapeutic range as applied to cervical carcinoma.6 Surgical therapy may be effective for treatment purposes at Stage I. It is essentially the same surgical treatment of early Stage II cervical cancer which invaded the upper 1/3 of the vagina. The surgical approach primarily consists of radical hysterectomy and pelvic lymph nodes dissection. Lesions in the lower vagina are treated by a resection of inguinofemoral lymph nodes including external genitalia. A conservative treatment approach is recommended for young patients with microinvasive carcinoma or verrucous carcinoma. Verrucous carcinoma is a slowly growing, locally infiltrating and rarely metastasizing cancer. Therefore, it is not appropriate to perform a radical operation only based on the size or location of a lesion.7
In general, uterine prolapse combined with vaginal cancer is a very uncommon condition. After Howat et al.8 reported a patient with an entero-vaginal fistula, several other reports were published subsequently.2,3,8~11 However, there has been no such report domestically. Additionally, there has been no report of a case similar to ours that exhibits progressive vaginal cancer associated with multiple organ metastasis. It is common that ulcerating lesions is a presenting symptom of uterine prolapse combined with vaginal cancer. It assumes that vagina may be exposed to inflammatory response and chronic irritation.7 Fonseca et al.12 examined cytologic, colposcopic and histological findings in patients with uterine prolapse. The report showed chronic cervicitis in 97.9%, cervix decubital ulcer in 13.6% and carcinoma in situ in 1%.12 It suggests the importance of preoperative evaluation of cervix on uterine prolapse in order to exclude the possibility of cervical carcinoma. Cho et al.13 analyzed a total of 154 patients with uterine prolapse who underwent hysterectomy and two patients were found to have cervical carcinoma. As with concerns of possibility of vaginal cancer if any changes in the epithelium or ulcer are suspected, preoperative biopsies are highly required. In our case, the patient had suffered for 20 years from uterine prolapse. A patient with a long history of uterine prolapse must be treated with care due to the risk potential for malignant change. It is essential to pay careful attention to patients with uterine prolapse by performing various tests to discover malignant lesions before surgical treatment.
The authors conclude that on these unfavorable changes in the condition, including vaginal bleeding, coldness with foul odor and ulcerating lesions, biopsies must be performed before treatment.
Figures and Tables
Fig. 1
Histopathology of biopsied specimen showing squamous cell carcinoma of the vagina (H & E, × 200).
References
1. Benedet JL, Bender H, Jones H 3rd, Ngan HY, Pecorelli S. FIGO Committee on Gynecologic Oncology. FIGO staging classifications and clinical practice guidelines in the management of gynecologic cancers. Int J Gynaecol Obstet. 2000; 70:209–262.
2. Iavazzo C, Vorgias G, Vecchini G, Katsoulis M, Akrivos T. Vaginal carcinoma in a completely prolapsed uterus. A case report. Arch Gynecol Obstet. 2007; 275:503–505.
3. Karateke A, Tugrul S, Yakut Y, Gürbüz A, Cam C. Management of a case of primary vaginal cancer with irreducible massive uterine prolapse--a case report. Eur J Gynaecol Oncol. 2006; 27:528–530.
4. Creasman WT. Vaginal cancers. Curr Opin Obstet Gynecol. 2005; 17:71–76.
5. Park J, Kim TH, Lee HH, Lee W, Chung SH. Lichen sclerosus in a post-menopausal woman: a case report. J Korean Soc Menopause. 2012; 18:70–73.
6. Berek JS, Hacker NF. Berek and Hacker's gynecologic oncology. 5th ed. Philadelphia, PA: Lippincott Williams & Wilkins;2010.
7. Barakat RR, Markman M, Randall ME. Principles and practice of gynecologic oncology. 5th ed. Philadelphia, PA: Lippincott Williams & Wilkins;2009.
8. Howat JM, Stassan L, Mohandas I, Daw E. Carcinoma of the vagina presenting as a ruptured procidentia with an entero-vaginal fistula and prolapse of the small bowel. Postgrad Med J. 1984; 60:435–436.
9. Ghosh SB, Tripathi R, Mala YM, Khurana N. Primary invasive carcinoma of vagina with third degree uterovaginal prolapse: a case report and review of literature. Arch Gynecol Obstet. 2009; 279:91–93.
10. Gupta N, Mittal S, Dalmia S, Misra R. A rare case of primary invasive carcinoma of vagina associated with irreducible third degree uterovaginal prolapse. Arch Gynecol Obstet. 2007; 276:563–564.
11. Rao K, Kumar NP, Geetha AS. Primary carcinoma of vagina with uterine prolapse. J Indian Med Assoc. 1989; 87:10–12.
12. Fonseca AM, Pereyra EAG, Valente SE, Assoni L, Souza AZ. Colposcopic, cytologic and histologic findings in patients with uterine prolapse of second and third degree. Arq Bras Med. 1988; 62:273–275.
13. Cho KI, Prk CH, Choi GS, Huh CK. To cases of uterine prolapse combined with cervical carcinoma. Korean J Obstet Gynecol. 1993; 36:3351–3357.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download