TO THE EDITOR: Phlegmasia cerulea dolens (PCD) is a severe and uncommon complication of deep vein thrombosis (DVT). It is associated in most cases with pulmonary embolism (PE) and has a high mortality rate. PCD refers to extreme cases of lower-extremity DVT that cause critical limb ischemia, and may lead to limb loss. The main complications of PCD are gangrene, compartment syndrome, local arterial compromise, and severe hypovolemic shock [1].
The main predisposing factors for the development of PCD are neoformative processes, hypercoagulable states, congestive heart failure, pregnancy, and prolonged immobilization. On a local level, other factors could be highlighted, such as anatomical abnormalities, previous history of DVT, previous femoral vein catheterization, or surgical procedures involving the affected limb [2].
The diagnosis of PCD is mainly clinical, and should be suspected in a patient manifesting four cardinal symptoms: edema, cyanosis, pain, and severe obstruction to venous flow [3]. The diagnosis of PCD should be confirmed with a doppler ultrasound of the limb. Other diagnostic tests include computed tomography angiography, magnetic resonance angiography and phlebography.
PCD management is controverted, and should be individualized. There are many modalities from anticoagulation alone to surgical thrombectomy. We present a single case report of cancer-associated PCD with conservative management treated with a direct oral anticoagulant (DOAC) which showed good clinical response including resolution of edema and no further complications in terms of bleeding or venous thromboembolism (VTE) recurrence during follow-up.
We present a case of 71-year-old male with the histories of untreated arterial hypertension, tobacco consumption and a large incarcerated umbilical hernia that requires surgical treatment. The patient came to the emergency room with a two hour history of sudden swelling, cyanosis and coldness of his left lower limb (LLL). He also complained of severe pain and functional impotence of the limb. Upon examination, he presented a blood pressure of 154/88 mmHg, pulse rate of 93 beats per minute and an oxygen saturation of 97%. Abdominal examination revealed no guarding or rebound tenderness. He also presented with cyanosis and cold skin in the LLL (Fig. 1A). The distal pulses were not palpable but there were no signs of neuronal damage.
Blood tests performed at the emergency department showed hemoglobin 15.4 g/dL, platelets 234,000/µL, leukocytes 7,700/µL. The coagulation tests were normal. Arterial blood gases showed pH 7.44 with pCO2 29 mmHg and pO2 48 mmHg. Chemistry test, including creatinine 0.78 mg/dL, glucose 106 mg/dL, alanine transaminase (ALT) 35 IU/L, and aspartate transaminase (AST) 30 IU/L, were normal. Cardiac markers were not tested. A chest X-ray showed right fibrothorax that was already present in a previous X-ray performed 7 years ago.
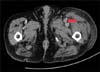
Upon admission a computerized tomography (CT) angiography of the LLL was performed (Fig. 2), which showed a hyperacute and extensive proximal DVT affecting the iliac vein, common femoral vein, femoral vein, and popliteal vein. CT also showed a partial external compression of the external iliac vein by an adenopathy. Arterial blood flow within the LLL was diminished, but there was residual flow. These findings were compatible with the clinical diagnosis of PCD. A CT of the thorax and abdomen was also performed, and revealed a segmental PE in the lower lobe of the right lung. It also confirmed the presence of retroperitoneal adenopathies and a prostatic node. A large umbilical hernia was also observed, with no signs of complication. The prostate-specific antigen (PSA) level was 124 ng/mL and antiphospholipid antibody tests yielded negative results. A transthoracic echocardiogram showed normal right ventricle function with a pulmonary artery systolic pressure of 22 mmHg.
The patient was treated with unfractionated heparin during the first 48 hours, along with Trendelenburg position and compression stockings. He was admitted to the Venous Thromboembolism Unit of the Internal Medicine Ward. Treatment was then switched to bemiparin, the low molecular weight heparin (LMWH), with a dose of 10,000 IU per day (115 IU/kg/day). The patient showed general improvement, including less pain, edema reduction, and progressive disappearance of cyanosis in the LLL.
Given the proximal extension and severity of the DVT and the patient's stability, mechanical removal of the thrombus was considered. However, the patient presented a large umbilical hernia that rendered him unable to lie in the prone position for the duration of the procedure, which was therefore dismissed.
In the fourth day of bemiparin treatment, the patient developed a drug induced rash. Allergy to LMWH was confirmed and treatment was then switched to apixaban. Nine days after admission, he was discharged on apixaban and compression stockings. Considering the local compression of the iliac vein by local adenopathy, the patient was referred with priority to the urology outpatient clinic for diagnosis and treatment of prostate cancer.
A week later, the patient underwent a prostatic biopsy, which confirmed the presence of a prostatic acinar adenocarcinoma with no bone infiltration on scintigraphy. Hormonal therapy was initiated.
After 6 months of treatment with apixaban and hormonal therapy, the patient's condition slowly improved, with a marked reduction of LLL edema and normal skin color (Fig. 1B). Levels of PSA decreased to 2.7 ng/mL six months after the initiation of hormonal therapy and reached values of 0.2 ng/mL a year later. The rapid response to hormonal therapy added to anticoagulant therapy probably contributed to the improvement of PCD. Upon examination during follow-up, he presented with incipient post-thrombotic syndrome.
PCD is a result of the complete obstruction of the venous drainage of the limb secondarily to an extensive DVT, with subsequent arterial compromise. It is three times more frequent in the left lower limb than in the right one, and is usually associated with hypercoagulable states, especially cancer [24].
Treatment differs according to the severity of the process. The first-line treatment is usually anticoagulation with unfractionated heparin, hydration, and elevation and compression of the affected limb [5].
Furthermore, in DVT (associated or not with PCD) there are strategies for the early removal of the thrombus, such as systemic fibrinolysis, not recommended because of the frequent complications such as incomplete fibrinolysis and bleeding. More direct approaches include surgical thrombectomy, catheter-directed thrombolysis (CDT) and catheter-directed thrombolysis with local fibrinolysis [6]. All these procedures have a weak degree of evidence and need further studies to support their usefulness in the treatment of acute DVT.
Surgical thrombectomy seems a reasonable option in the most severe cases of PCD with acute arterial compromise. A recent study suggested a reduction in the incidence of post-thrombotic syndrome in patients treated with surgical thrombectomy instead of anticoagulation alone [7].
Regarding CDT, patient selection is important. Both the Society for Vascular Surgery and the American Venous Forum suggest early thrombus removal in patients fulfilling the following criteria: 1) first episode of active ilio-femoral DVT, 2) symptoms lasting less than 14 days, 3) low risk of bleeding, 4) good functional status and acceptable life expectancy [8].
In our case there was a technical contraindication: the procedure has to be performed in a prone position (1–3 hr) to allow access to the deep venous system through the popliteal vein. This was not possible in our patient due to his large irreducible umbilical hernia. For this reason, and given the good evolution of the clinic with anticoagulation alone, conservative management was continued.
Finally, we would like to highlight the use of DOACs for the treatment of VTE in patients with cancer. Nowadays, first-line treatment in these patients consists in LMWH. However, recent studies seem to indicate that DOACs could be safe for the treatment of VTE in patients with cancer [9]. Further studies are needed to support the use of DOACs in these patients. In our patient, DOACs were exceptionally administrated because he was allergic to LMWH, with no evidence of bleeding or thrombosis recurrence on follow-up. To the best of our knowledge, this is the first case of cancer associated PCD successfully treated with DOACs.
Figures and Tables
References
1. Perkins JM, Magee TR, Galland RB. Phlegmasia caerulea dolens and venous gangrene. Br J Surg. 1996; 83:19–23.

2. Galanaud JP, Sevestre-Pietri MA, Bosson JL, et al. Comparative study on risk factors and early outcome of symptomatic distal versus proximal deep vein thrombosis: results from the OPTIMEV study. Thromb Haemost. 2009; 102:493–500.

3. Mumoli N, Invernizzi C, Luschi R, Carmignani G, Camaiti A, Cei M. Phlegmasia cerulea dolens. Circulation. 2012; 125:1056–1057.

4. Tung CS, Soliman PT, Wallace MJ, Wolf JK, Bodurka DC. Successful catheter-directed venous thrombolysis in phlegmasia cerulea dolens. Gynecol Oncol. 2007; 107:140–142.

5. Schweizer J, Kirch W, Koch R, et al. Short- and long-term results after thrombolytic treatment of deep venous thrombosis. J Am Coll Cardiol. 2000; 36:1336–1343.

6. Fahrni J, Engelberger RP, Kucher N, Willenberg T, Baumgartner I. Catheter-based treatment of ilio-femoral deep vein thrombosis - an update on current evidence. Vasa. 2013; 42:161–167.

7. Casey ET, Murad MH, Zumaeta-Garcia M, et al. Treatment of acute iliofemoral deep vein thrombosis. J Vasc Surg. 2012; 55:1463–1473.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download