TO THE EDITOR: Lymphomas with villous morphology are uncommon, and the rarest type is the splenic diffuse red pulp small B-cell lymphoma (SDRPL). Few SDRPL cases have been reported in the literature. There is considerable overlap with lymphomas that display villous lymphocytes in blood and splenomegaly, such as the rare variant hairy-cell leukemia, and splenic marginal zone lymphoma. Nonetheless, recent studies have produced clear, differentiating features regarding clinical, morphological, and immunophenotypical data. We highlight the case of a middle-aged male patient with massive splenomegaly and villous lymphocytes, diagnosed with SDRPL based on splenic histology and a characteristic immunoprofile. Diagnosis of SDRPL rests mainly on the exclusion of other lymphomas and on a correlation of bone marrow and spleen histology, and immunophenotyping. Our experience provides further support in considering this enigmatic lymphoma as a distinct entity within the WHO classification of lymphoid neoplasms.
Splenic diffuse red pulp small B-cell lymphoma (SDRPL) is an extremely uncommon lymphoma (incidence <1% of non-Hodgkin lymphoma) that is currently classified as a provisional entity under the Splenic B-cell Lymphoma/Leukemia Unclassifiable Category in the 2008 WHO edition, and in the recently published 2016 update of WHO Lymphoid neoplasms [12]. A leukemic presentation with splenomegaly, bone marrow dissemination, and hairy cells in the peripheral blood is the ‘sine qua non’ for SDRPL, however these features are far from being specific. There is a considerable amount of morphological overlap with other lymphomas that primarily afflict the spleen and also display villous lymphocytes, such as splenic marginal zone lymphoma (SMZL), hairy-cell leukemia (HCL) and, rarely, the hairy-cell leukemia-variant (HCL-V) [345]. Although these similarities may pose difficulties in diagnosis, recent literature has shown convincing differences in histological, immunophenotypical, molecular, and clinical characteristics of this rare lymphoma [567]. Characteristic spleen histology, together with a combination of immunohistochemistry (IHC) and immunophenotyping, are essential for diagnosis. Although studies show SDRPL to be an indolent malignancy, differentiation is crucial for devising therapeutic strategies for the patient [358]. SDRPL is an unfamiliar entity and we present a rare case report of a 45-year-old male who was clinically diagnosed with a splenic lymphoma.
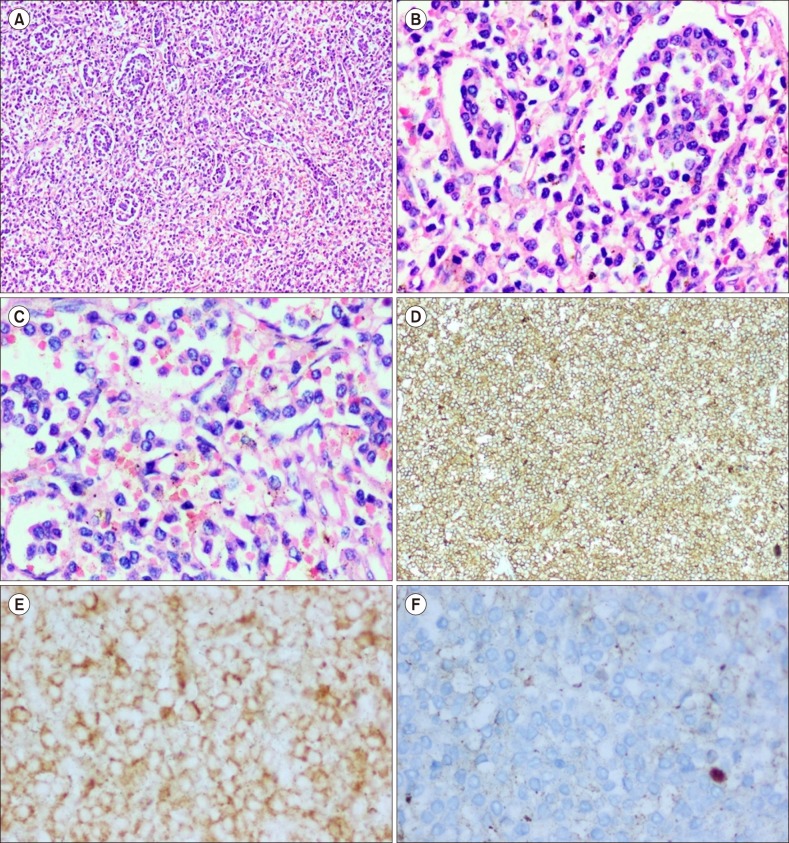
A 45-year-old male presented with abdominal swelling and generalized weakness. Co-morbidities included diabetes mellitus and alcoholic chronic liver disease. An abdominal ultrasonogram showed massive splenomegaly and mild hepatomegaly without any significant intra-abdominal lymphadenopathy. Routine blood investigations showed a total leukocyte count (TLC) count of 300×109/L, and a subsequent peripheral smear examination showed atypical lymphocytes with copious finger-like projections (Fig. 1). A bone marrow (BM) aspirate revealed atypical lymphoid cells (79%) with an inconspicuous nucleoli and circumferential hairy-like projections, and the TRAP (tartrate-resistant acid phosphatase) stain was negative. Flow cytometric analysis demonstrated negativity for CD103, CD123 and Annexin-A1. The BM trephine biopsy confirmed an intrasinusoidal and interstitial infiltrate of atypical lymphoid cells highlighted by CD20 and DBA-44, and non-reactive for CD5, CD23 and Annexin-A1 immunostaining (Fig. 2). A splenectomy was undertaken and the specimen measured 30×20×17 cm, with a weight of 4.1 kilograms. The cut surface was homogenous and beefy-red, displaying wedge-shaped sub-capsular infarcts, devoid of any gray-white nodules (Fig. 3). Histological examination showed a tumor growing diffusely in the red pulp sinuses and cords with extensive obliteration of the splenic white pulp. Tumor cells were monotonous, small and round with smooth nuclear contours, inconspicuous nucleoli, and scant cytoplasm. Mitotic activity was also inconspicuous. IHC showed diffuse positivity for CD20, PAX-5, CD79a and DBA-44 with a low MIB-1 proliferation index of 2% to 4% (Fig. 4). The tumor cells were negative for CD3, CD25, Cyclin-D1, CD123 and Annexin-A1. Cytogenetic analysis also did not reveal any of the known mutations associated with SMZL, HCL and HCL-V.
In view of the clinical features, splenic and BM trephine histology, immunoprofile and the cytogenetic work-up, the diagnosis was consistent with SDRPL. Following splenectomy, our patient was started on rituximab to which he was intolerant, therefore the CHOP (cyclophosphamide, Adriamycin, vincristine and prednisolone) protocol was initiated. After completing 6 cycles of chemotherapy and 22 months of regular follow-up, our patient is in remission and disease-free state with normal blood counts and bone marrow examination results.
Lymphoma is the most common malignancy of the spleen and, in the clear majority of cases, it is secondarily involved. Primary splenic lymphomas are rare, comprising approximately 1% of all lymphomas, and are usually of B-cell origin [9]. Neoplastic villous lymphocytes can be seen in a variety of chronic lymphoproliferative disorders; however, the most common splenomegalic lymphoma with villous processes is SMZL, followed by HCL and its rare variant, HCL-V.
SDRPL is the newest addition to this growing list in the latest 2008 edition of WHO classifications, as well as in the recently published 2016 WHO update of lymphoid neoplasms [2]. It is extremely rare, with an estimated incidence of less than 1% of all non-Hodgkin lymphomas, and is discussed in the published literature in the form of occasional case reports that describe its clinicopathological features [345810]. SDRPL mimics SMZL, HCL, and HCL-V, clinically and morphologically, with considerable overlap immunophenotypically.
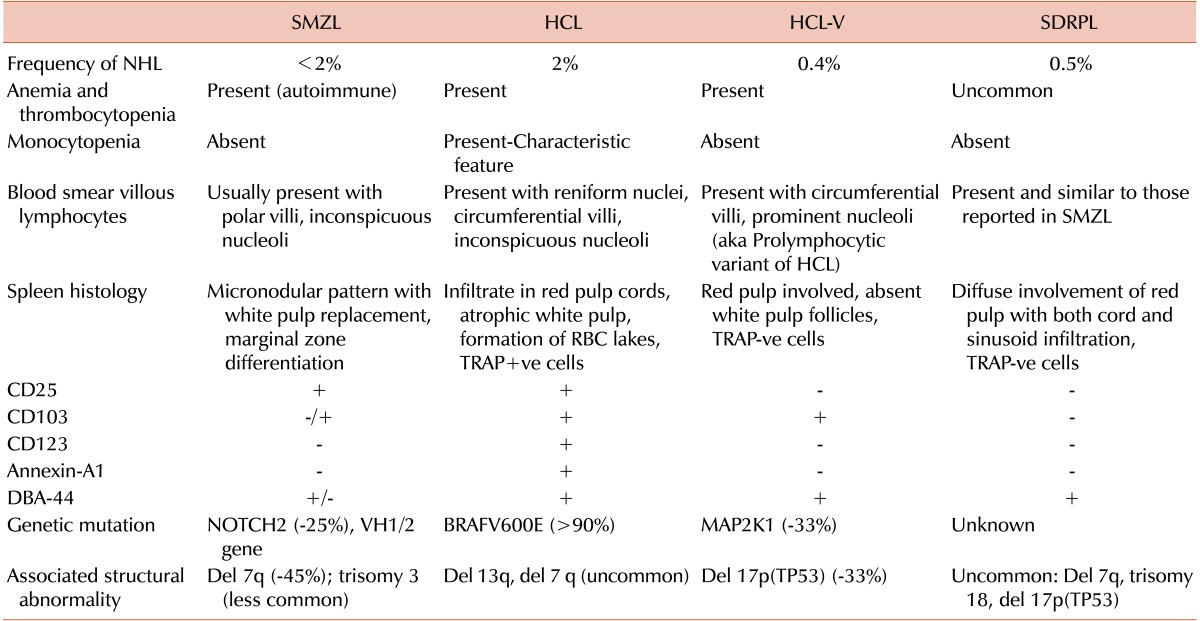
Nonetheless, emerging data and studies show clear delineating features among these neoplasms (Table 1).
Patients are typically older than 40 years of age, and there is a slightly higher representation of males than females [8]. The leukemic presentation is typical, with massive splenomegaly and a varying magnitude of cytopenias, but B-symptoms are not encountered. Peripheral smears show the characteristic villous morphology mimicking HCL and SMZL, however, nucleoli are inconspicuous [8]. Bone marrow involvement has been seen in all reported cases to date, with an intrasinusoidal and interstitial growth pattern [4810]. Unlike SMZL, HCL and HCL-V, which can be diagnosed on peripheral blood/BM trephine biopsy, SDRPL requires splenectomy for confirmation of the diagnosis [4]. Spleen histology shows diffuse infiltration of the red pulp due to small monotonous lymphocytes causing virtual obliteration of the white pulp [4810], a feature in contrast to SMZL which involves only the white pulp.
SDRPL accounts for approximately 10% of lymphomas diagnosed solely on splenectomy [19], necessitating the use of ancillary tests for correlation and confirmation. The immunoprofile involves characteristic tumor cells being consistently positive for CD20, DBA-44, and IgG. SDRPL is negative for CD3, CD5, CD10, CD11c, CD23, CD25, CD103, CD123, Cyclin-D1, and Annexin-A1 [3467810].
No specific genetic mutation or chromosomal abnormality has been identified, based on the studies so far, although occasional cases have shown del 7q, del 17p(TP53) and trisomy 18 [810]. Mutations seen in HCL, such as BRAF-V600E (>90% of cases) and the VH1.2 gene, or Chromosome 7q loss as seen in SMZL, have never been observed [11].
SDRPL follows a clinically benign course with a favorable long-term survival rate. The diagnosis of SDRPL should be made based on a constellation of clinical features, peripheral smear morphology, marrow and spleen histology, immunophenotyping, and cytogenetics. Differentiation is essential as SDRPL has a good prognosis and is resistant to conventional chemotherapy that is usually effective for the treatment of HCL, HCL-V and SMZL. This is an indolent but incurable disease with a good response after splenectomy.
Acknowledgments
The authors wish to thank Dr Sukesh Nair and Dr Joy Mammen, Department of Transfusion Medicine & Immunohematology, for providing high quality images of peripheral smear.
References
1. Piris MA, Foucar KM, Mollejo M, Campo E, Falini B. Splenic lymphoma/leukemia, unclassifiable. In : Swerdlow SH, Campo E, Harris NL, editors. WHO classification of tumors of hematopoietic and lymphoid tissues. 4th ed. Lyon, France: IARC Press;2008. p. 191–193.
2. Swerdlow SH, Campo E, Pileri SA, et al. The 2016 revision of the World Health Organization classification of lymphoid neoplasms. Blood. 2016; 127:2375–2390. PMID: 26980727.

3. Ponzoni M, Kanellis G, Pouliou E, et al. Bone marrow histopathology in the diagnostic evaluation of splenic marginal-zone and splenic diffuse red pulp small B-cell lymphoma: a reliable substitute for spleen histopathology? Am J Surg Pathol. 2012; 36:1609–1618. PMID: 23073320.
4. Behdad A, Bailey NG. Diagnosis of splenic B-cell lymphomas in the bone marrow: a review of histopathologic, immunophenotypic, and genetic findings. Arch Pathol Lab Med. 2014; 138:1295–1301. PMID: 25268192.

5. Cessna MH, Hartung L, Tripp S, Perkins SL, Bahler DW. Hairy cell leukemia variant: fact or fiction. Am J Clin Pathol. 2005; 123:132–138. PMID: 15762289.
6. Dong HY, Weisberger J, Liu Z, Tugulea S. Immunophenotypic analysis of CD103+ B-lymphoproliferative disorders: hairy cell leukemia and its mimics. Am J Clin Pathol. 2009; 131:586–595. PMID: 19289595.
7. Traverse-Glehen A, Baseggio L, Bauchu EC, et al. Splenic red pulp lymphoma with numerous basophilic villous lymphocytes: a distinct clinicopathologic and molecular entity? Blood. 2008; 111:2253–2260. PMID: 18042795.

8. Kanellis G, Mollejo M, Montes-Moreno S, et al. Splenic diffuse red pulp small B-cell lymphoma: revision of a series of cases reveals characteristic clinico-pathological features. Haematologica. 2010; 95:1122–1129. PMID: 20220064.

9. Gujral S, Lad P, Subramanian PG, et al. Histopathological audit of splenectomies received at a cancer hospital. Indian J Pathol Microbiol. 2011; 54:487–496. PMID: 21934208.

10. Traverse-Glehen A, Baseggio L, Salles G, Coiffier B, Felman P, Berger F. Splenic diffuse red pulp small-B cell lymphoma: toward the emergence of a new lymphoma entity. Discov Med. 2012; 13:253–265. PMID: 22541613.
11. Tiacci E, Trifonov V, Schiavoni G, et al. BRAF mutations in hairy-cell leukemia. N Engl J Med. 2011; 364:2305–2315. PMID: 21663470.
Fig. 1
Peripheral blood smear showed the presence of atypical lymphoid cells with numerous circumferential hair-like processes and inconspicuous nucleoli. Inset shows a neoplastic lymphocyte with appreciable villous processes.
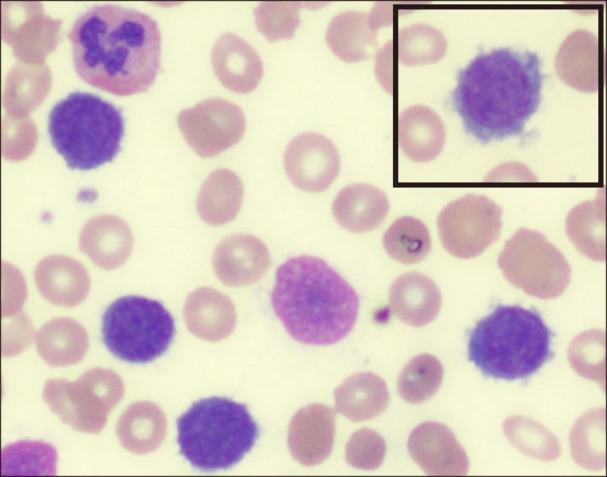
Fig. 2
Bone marrow trephine biopsy. (A–C) There is an interstitial and sinusoidal infiltrate due to a small lymphoid population (H&E, magnification ×100, ×400 and ×400). (D) Immunostaining for CD20 highlights the intrasinusoidal infiltrate (×40 magnification).
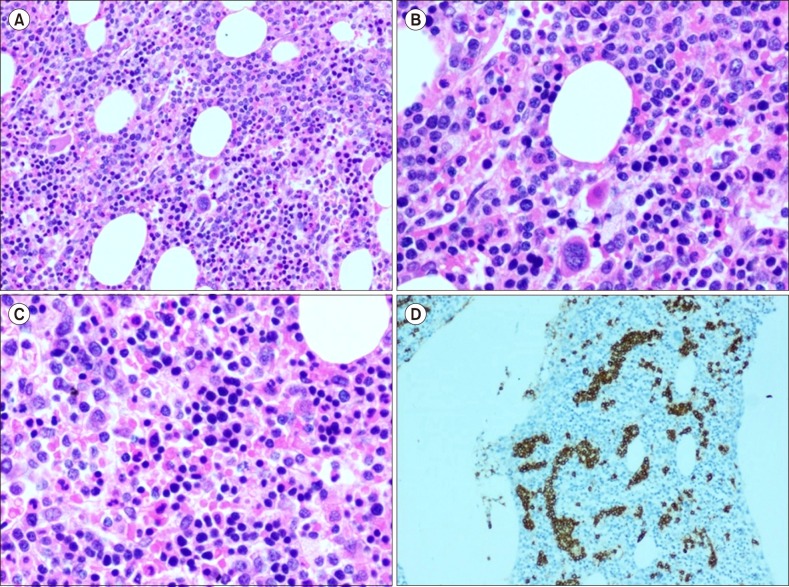
Fig. 3
Splenectomy specimen shows diffusely enlarged spleen with a beefy red homogenous cut surface and wedge-shaped subcapsular infarcts.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download