Abstract
Background
The prognosis of pediatric acute myeloid leukemia (AML) has recently improved. This study aimed to describe the epidemiology, changes in treatment strategies, and improvement of outcomes in Gwangju-Chonnam children with AML over 2 decades.
Methods
Medical records of 116 children with newly diagnosed AML were retrospectively reviewed for demographic characteristics, prognostic groups including cytogenetic risks, treatment protocols, and survival rates over the periods between 1996 and 2005 (Period I, N=53), and 2006 and 2015 (Period II, N=38).
Results
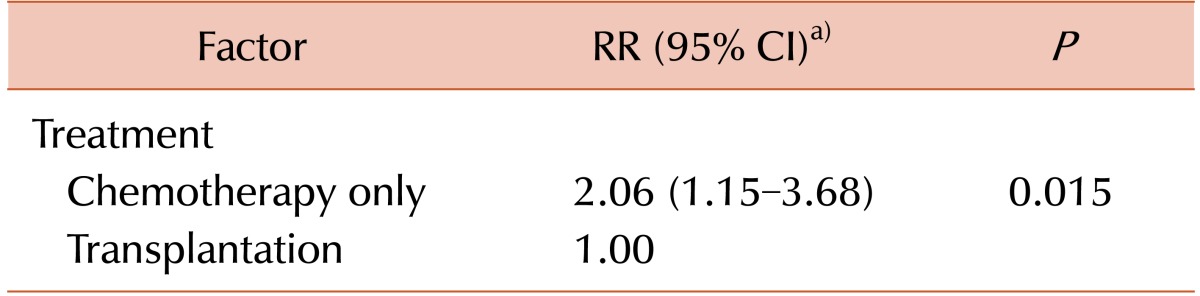
The annual incidence of AML has decreased with reduced pediatric population. The 5-year Kaplan-Meier (K-M) estimated overall survival (OS) and event-free survival (EFS) rates in 110 AML patients were 53.2±5.1% and 43.8±5.1%, respectively. The 5-year OS rate significantly improved during period II (70.3±7.0%) as compared to that during period I (40.0±6.8%) (P =0.001). The 5-year OS was not significantly different among cytogenetic risk groups (P =0.11). Fifty-eight patients underwent hematopoietic stem cell transplantation (HSCT). The K-M 5-year estimated survival for transplanted patients was 53.7±7.0%, while that for chemotherapy-only patients was 30.1±9.1% (P =0.014). Among the prognostic factors, treatment modality was the only independent factor. The chemotherapy-only group had a relative risk of 2.06 for death compared with the transplantation group (P=0.015).
Conclusion
The survival of Korean children with AML has improved to a level comparable with that of developed countries over 2 decades, owing to a change in induction strategy, better supportive care with economic growth, refinement of HSCT techniques including a better selection of patients based on prognostic groups, and stem cell donor selection.
Acute myeloid leukemia (AML) is a clonal disease of the hematopoietic tissue, characterized by abnormal proliferation of myeloid progenitor cells, resulting in insufficient generation of normal mature blood cells [1]. AML accounts for approximately 25% and 33.3% of pediatric leukemia worldwide and in Korea, respectively [234]. AML is a group of heterogeneous diseases with different biological subtypes and various clinical courses. Patients with favorable cytogenetics involving the core binding factor, such as t(8;21), inv(16) or t(16;16) are expected to have >60% probability of survival, while patients with t(15;17) have survival rates of >80% [56]. In contrast, patients with adverse risk cytogenetics, those refractory to intensive induction chemotherapy, and those with secondary leukemia that transformed from myelodysplastic syndrome (MDS) or other hematologic disorders, have poor outcomes with chemotherapy alone [78].
The dramatic improvement of outcomes in pediatric AML over the last 3 decades has been achieved with intensification of chemotherapy, improvements in supportive care, wider application of various hematopoietic stem cell transplantations (HSCT), recent advances in stratification into risk groups based on cytogenetics and more recently on molecular genetics, and early response evaluation by minimal residual disease [457]. Currently, the overall survival (OS) in pediatric AML patients ranges from 60–70% [23910].
A similar trend in AML outcomes has been observed in Korea over the decades with advancements in the field of hematology-oncology. The survival rate of Korean patients with AML was <10% prior to 1990 because of limited access to chemotherapy agents, lack of effective regimen and medical experiences, and poor supportive care [11]. Recently, survival data of 2,107 children with AML aged 0–14 diagnosed from 1993–2011, from the Korea National Cancer Incidence database of the Korea Central Cancer Registry (KCCR) have been made available. The survival of AML children showed marked improvement from 26.5% in 1993–1995 to 59.7% in 2007–2011 [3]. Nevertheless, only a few publications on survival are available for childhood AML in Korea [312].
This retrospective study was aimed at describing the epidemiology and therapeutic improvement of outcomes in childhood AML in the Gwangju and Chonnam province of Korea over 2 decades from 1996 to 2015. Socioeconomic growth has been quite remarkable in Korean over the period, and the number of children aged 0–19 has decreased by 36.4% (from 1.1 million to 0.7 million) in the Gwangju and Chonnam province according to the National Statistics Office [13]. This study aimed to evaluate recent changes in outcomes of childhood AML in Korea.
Medical records of all newly diagnosed pediatric AML patients younger than 19 years (N=116) who were admitted to the Departments of Pediatrics at the Chonnam National University Hospital (CNUH) and Chonnam National University Hwasun Hospital (CNUHH) from January 1, 1996 to December 31, 2015, were retrospectively reviewed. This study was an observational, retrospective, descriptive study of clinical and epidemiological aspects of childhood AML, which was approved by the Institutional Review Board (IRB) of the CNUHH.
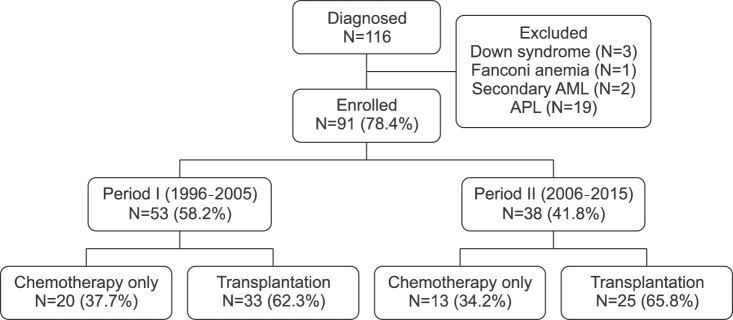
Patients with Down syndrome (N=3), Fanconi anemia (N=1), or secondary AML (N=2) were excluded. Patients with acute promyelocytic leukemia (APL; AML M3) (N=19), a distinct subtype, were included in the survival analyses, but were excluded from further subgroup analyses because of differences in treatment regimens and superior survival outcomes [6]. Thus, a total of 91 patients were evaluated in this study. Patients were subdivided into 2 groups by time frames as follows: Period I (1996–2005; N=53) and Period II (2006–2015; N=38). Patient demographics, survival outcomes, and treatment strategies were compared between the 2 subgroups. The survival rate was assessed as of December 31, 2016. Patients were censored at the time of event or last follow-up.
Diagnosis of AML was made by morphologic criteria of bone marrow (BM) using the French-American-British (FAB) classification system [14], cytogenetics, and molecular characteristics. Cytogenetic risk status of the patients was stratified according to National Comprehensive Cancer Network [15] and the Medical Research Council criteria [16]. Favorable cytogenetics included t(8;21) and inv(16); unfavorable cytogenetics included −5, −7, abnormal 3q, t(6;9), and complex karyotypes (at least 3 unrelated abnormalities); and intermediate-risk cytogenetics included other abnormalities and normal karyotypes.
The KSBRM regimen (N=76), and the Korean AML 2012 regimen (N=15) were the treatment protocols used. The KSBRM regimen is based on idarubicin plus N4-behenoyl-1-β-D-arabinofuranosyl cytosine (BHAC) chemotherapy [12]; the Korean AML 2012 regimen is a double-induction regimen consisting of idarubicin (IDA) or mitoxantrone plus cytarabine based chemotherapy.
Patients were initially treated with remission-induction therapy from either one of the above protocols. Complete remission (CR) was defined as <5% of leukemic blasts in the BM, evidence of normal hematopoiesis, and no leukemia cells in the peripheral blood (PB) or elsewhere. Induction death was defined as a fatal event occurring within the first 6 weeks of treatment. Partial remission (PR) was defined as a BM with 5–15% blast cells and evidence of regeneration of normal hematopoietic cells. Patients who did not achieve CR or PR and who survived after the first 6 weeks of treatment were defined as non-responders (NR) [12].
After achieving CR, four courses of consolidation chemotherapy consisting of anthracyclines, etoposide, and cytosine arabinoside were administered in most patients who were not candidates for HSCT. In earlier years of the study period, allogeneic HSCT was recommended to all patients in first remission with human leukocyte antigen (HLA)-matched familial or unrelated donors. In addition, autologous HSCT was offered to several patients who did not have a matched donor. In recent years, however, allogeneic HSCT was not recommended to patients with favorable cytogenetics. HLA typing for class I and class II antigens was performed using standard serologic techniques in earlier years, but by DNA typing since 2002. Donors were considered fully matched by compatibility for HLA-A, -B, -C, and -DRB1. Patients were subdivided into two groups by treatment modality after achieving remission: a transplantation group who underwent either allogeneic or autologous HSCT and a chemotherapy-only group who received consolidation chemotherapy without HSCT.
Medical records were retrospectively reviewed on demographic findings such as age, sex, white blood cell (WBC) count at diagnosis, morphologic, cytogenetic, and molecular classification of AML. The methods of treatment analyzed were as follows: remission-induction regimen, HSCT, and the donor source of HSCT. Remission induction rate, overall and event-free survival rate, and causes of deaths were compared.
Overall survival (OS) was defined as the time between diagnosis and death from any cause or time of last contact. Event-free survival (EFS) was calculated from the date of diagnosis to last follow-up or first event (failure to achieve remission, relapse, second malignancy or death due to any cause, whichever occurred first). Continuous variables were expressed as mean±standard deviation; categorical variables were expressed as numbers and percentages. Continuous variables were compared using the Student's t-test and categorical variables were compared using the chi-square test or the Fisher's exact test. Probabilities of survival were estimated using the Kaplan-Meier (K-M) method and were compared using the log-rank test. Prognostic variables were evaluated by multivariate analyses using a Cox regression proportional hazard model. P-value <0.05 was considered statistically significant. The software package SPSS version 21.0 (SPSS Inc, Chicago, IL, USA) was used for all statistical analyses.
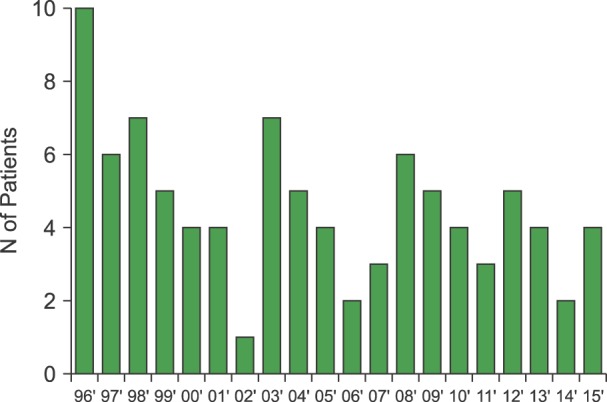
A total of 110 primary AML patients without constitutional diseases were observed over the study period. After excluding 19 patients with APL, 91 patients were enrolled (Fig. 1). The annual numbers of newly diagnosed AML cases showed a decreasing trend over 2 decades, probably due to reduced childhood population (Fig. 2).
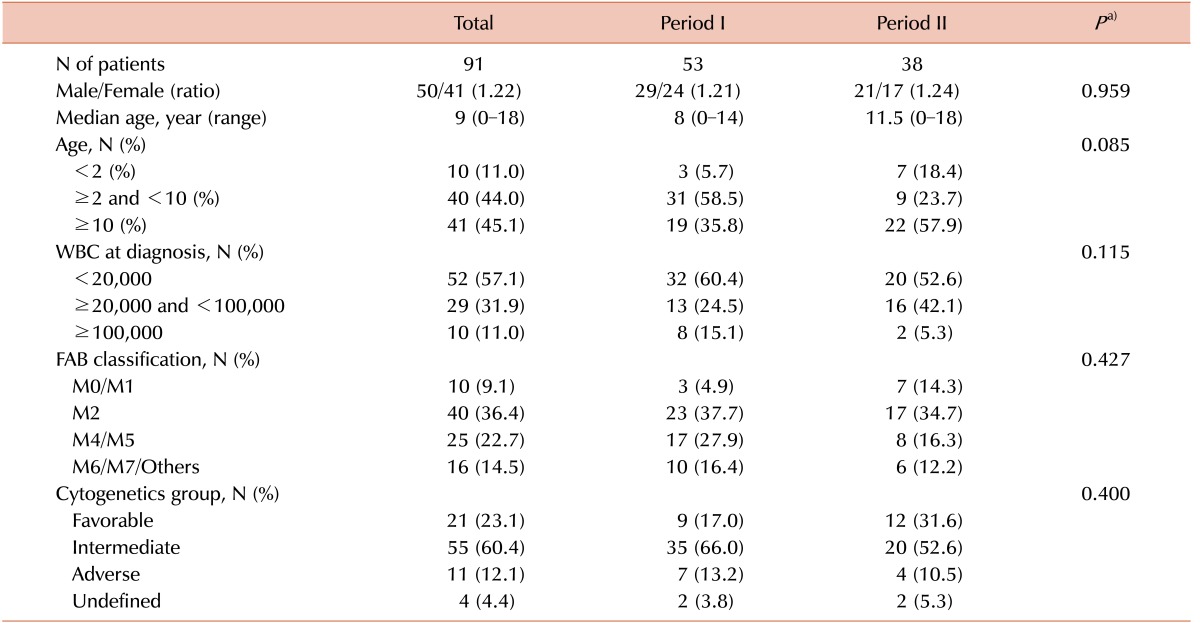
Patient characteristics of children with AML by study periods are shown in Table 1. Fifty patients (54.9%) were males (male/female ratio, 1.2:1). The median age at diagnosis was 9 years (range, 8 mo to 18 yr). Age distribution was: <2 years, 11.0%; 2–9 years, 44.0%; and ≥10 years, 45.1%. The median WBC count at diagnosis was 13,900/µL, and 10.8% of the patients had a WBC count of at least 100,000/µL. The most common subtype as per the FAB classification was AML M2. None of the above variables was significantly different between the 2 groups by study periods (Table 1).
Prognostic groups based on cytogenetics were categorized as favorable (23.1%), intermediate (60.4%), and adverse-risk (12.1%) groups. The distribution of groups was not different between the 2 study periods: favorable, 17.0% vs. 31.6%; intermediate, 66.0% vs. 52.6%; adverse, 13.2% vs. 10.5% (P=0.4). Cytogenetic data were not available in 4 patients (4.4%) due to inadequate culture or missing medical records (Table 1).
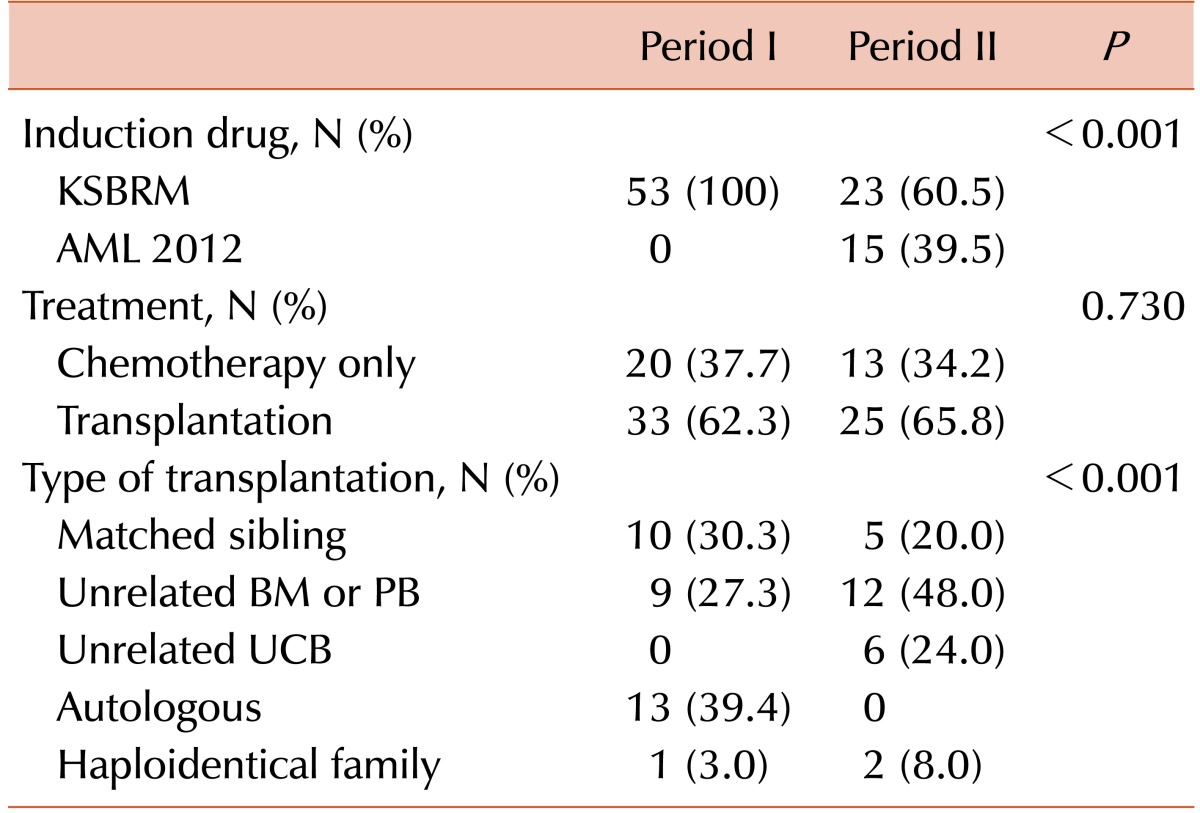
The trend of treatment policy over time is shown in Table 2. Most patients received the KSBRM induction regimen as the Korean AML 2012 regimen began to be used since 2012. The proportion of patients who underwent a HSCT was not different, but the type of transplantation was different between the 2 periods. Autologous transplantation was no more used in period II, and the proportion of unrelated donor transplants including cord blood transplants among allogeneic HSCTs increased from 45% (9/20) in period I to 72% (18/25) in period II (P=0.07).
The 5-year K-M estimated OS and EFS for 110 AML patients including APL were 53.2±5.1% and 43.8±5.1%, respectively (Fig. 3A, B). The OS and EFS were compared between the 2 study periods (Fig. 3C, D). The 5-year OS in children with AML was significantly improved during period II (70.3±7.0%) compared to that during period I (40.0±6.8%) (P=0.001), and the 5-year EFS was 56.9±7.7% and 33.3±6.5%, respectively (P=0.009).
After excluding APL, 43 among 91 enrolled patients survived with a median follow-up of 52 months. The 5-year K-M estimated OS and EFS for 91 enrolled patients were 45.3±5.7% and 35.3±5.5%, respectively (Fig. 4A, B). The 5-year OS was significantly improved during period II (61.6±8.6%) as compared to that during period I (34.1±7.3%) (P=0.007). The 5-year EFS for period I and period II were 26.1±6.9% and 47.7±8.9%, respectively (P=0.024) (Fig. 4C, D).
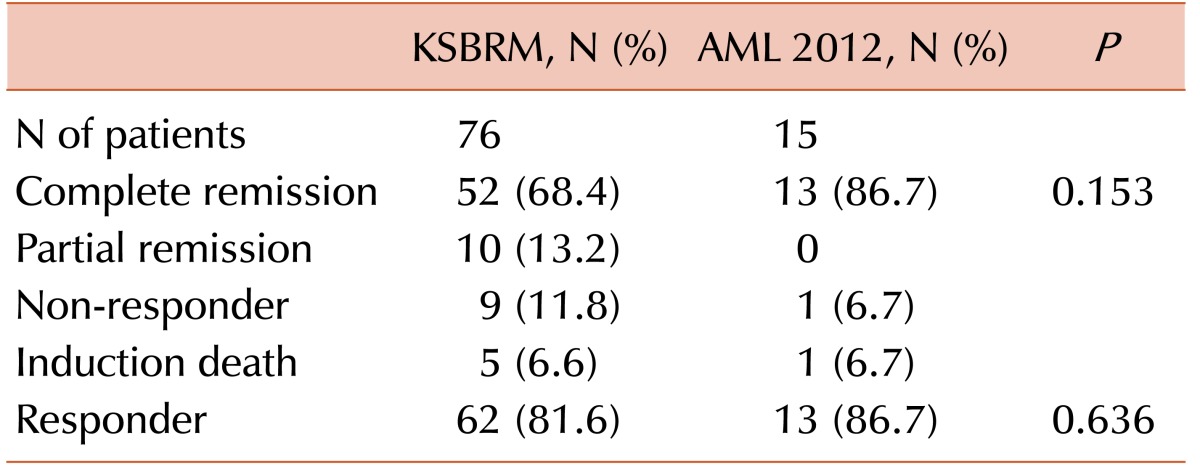
In addition, treatment outcomes were compared according to the induction regimens (Table 3). The treatment protocols used were mostly the KSBRM regimen (N=76), and the Korean AML 2012 regimen (N=15) since 2012. After remission-induction chemotherapy, 65 of 91 children (71.4%) achieved CR. The overall response rates of complete and partial remission were not significantly different (81.6% vs. 86.7%, P=0.64). The percentages of induction death were not different. The 2-year estimated OS and EFS of children were not significantly different between the 2 groups (60.3±5.6% vs. 64.6±12.9%, P=0.4 for OS; 48.2±5.8% vs. 58.7±13.0%, P=0.31 for EFS) (Fig. 5).
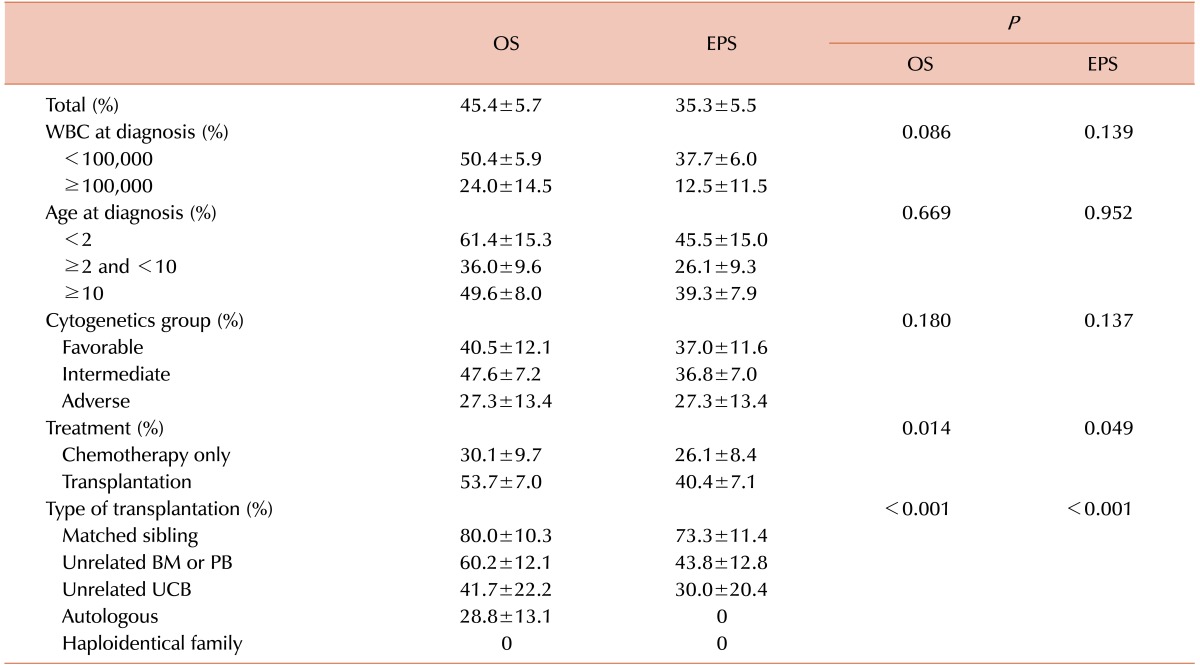
Prognostic factors that may predict OS and EFS were analyzed (Table 4). Patients with lower initial WBC counts (<100,000/µL) tended to have better survival (P=0.09). The adverse cytogenetic group had lower OS (27.3±1.4% vs. 40.5±12.1%) and EFS (27.3±13.4% vs. 37.0±11.6%) than did the favorable cytogenetic group (not significant, P=0.18) (Fig. 6).
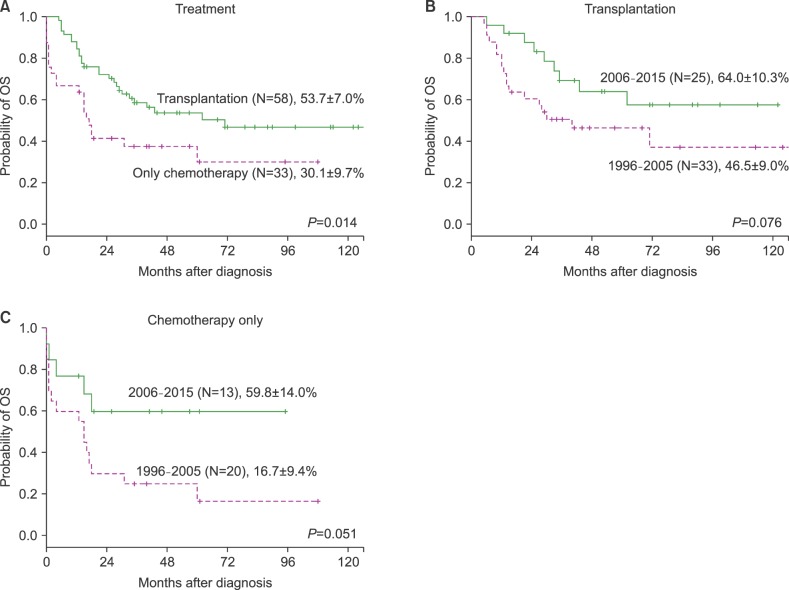
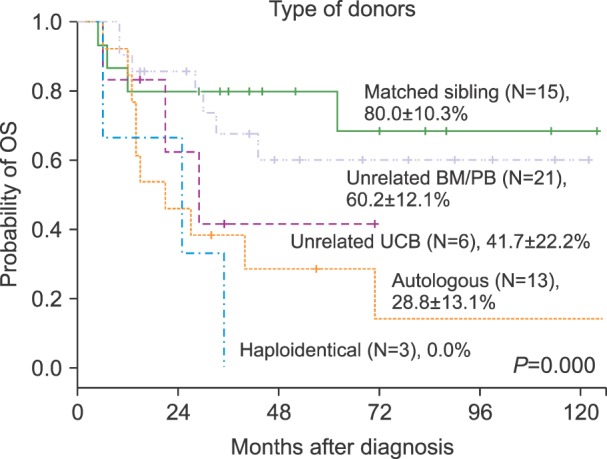
Fifty-eight patients underwent HSCTs (Table 2, 4). The proportion of patients who eventually underwent HSCTs was not different between the 2 periods (62.3% vs. 65.8%). The K-M 5-year survival for transplanted patients was 53.7±7.0%, while that of chemotherapy-only patients was 30.1±9.1% (Fig. 7A). The OS and EFS of patients tended to improve in period II as compared to that in period I (not significant in the HSCT and the chemotherapy-only groups) (Fig. 7B, C) (Data not shown for EFS). Survival was compared by stem cell sources: matched sibling donor conferred the best outcome of 80.0±10.3%, followed by unrelated BM/PB (60.2±12.1%), umbilical cord blood (41.7±22.2%), and autologous blood (28.8±13.1%) (P<0.001) (Fig. 8).
Among prognostic factors such as sex, age, WBC count at diagnosis, induction regimen and HSCT, treatment with HSCT was found to be the only independent factor (Table 5). The chemotherapy-only group had a relative risk of 2.06 for death as compared to the HSCT group (P=0.015).
In the present study, the survival rate in Korean children with AML was significantly improved during period II compared to that in period I. The survival rate of AML patients is important not only to individuals, but to the entire nation, as it is regarded as the indicator of level of care with both chemotherapy and HSCTs. Thus, improvement in AML survival rates reflects advances in medical care in general. During the period the gross national income per capita increased 240% from $11,432 to $27,300 according to the economic statistics of the Bank of Korea [17]. However, childhood AML remains a challenge because a significant portion of patients still succumb to death eventually. The overall incidence of childhood AML has been stable during recent decades worldwide [1819]. However, the annual incidence of AML has decreased with a decrease in childhood population in this study (Fig. 2). The number of children living in Gwangju and Chonnam province has decreased from 1,076,582 in 1995 to 708,804 in 2015 according to National Statistical Office [13].
Like in other studies, male sex was slightly predominant, and most patients were older than 2 years (Table 1) [20]. Patients with WBC counts ≥100,000/µL at diagnosis (11.0%) tended to have a lower 5-year OS compared to those with WBC counts <100,000/µL at diagnosis (24.0% vs. 47.8%, P=0.086). The percentage of patients with WBC counts ≥100,000/µL was between 12% and 15% [2021], and their probability of survival was only 23% according to the BFM-83 and BFM-87 treatment protocols [22]. The most prevalent morphological type was FAB M2 (36.4%), which was in close agreement with previous studies [2021].
AML with favorable cytogenetics accounted for approximately 20 to 30%, while adverse cytogenetic features made up approximately 15% of pediatric AML [5]. Children and adolescents harboring these unfavorable features had survival rates of <50%, and in many cases <20% [523]. Similar OS results were observed in patients in the adverse cytogenetic group as compared to those in the favorable cytogenetic group (27.3% vs. 40.5%) (Fig. 8, P=0.184). These results did not reach statistical significance probably due to the small number of patients in the adverse cytogenetics group (N=11), and biasing of these patients toward treatment with HSCTs.
In the present study, most of the patients received either of 2 induction regimens, the BHAC-based regimen or the Korean 2012 regimen. BHAC-based regimen, widely used since 1996 had a CR rate (75%) which was similar or superior to results obtained with cytarabine and other anthracyclines [24]. The Korean AML 2012 regimen is a double-induction strategy of re-administering 2nd induction chemotherapy on Day 28 after the first cycle, regardless of the initial response to treatment. First course of standard-dose cytarabine with IDA is followed by high-dose cytarabine with mitoxantrone. As it has been used since 2012, there have been no published reports of treatment results yet.
The remission induction rate of the Korean AML 2012 regimen appears to be high as compared to that of the KSBRM regimen in our study (86.7% vs. 68.4%, P=0.184) (Table 3). The proportion of NR was comparable between regimens (11.8% in the KSBRM regimen group; 6.7% in the Korean AML 2012 regimen group), while the Korean AML 2012 regimen tended to confer better survival rates (P=0.4) (Fig. 5). However, the small sample size of the Korean AML 2012 regimen group and the short follow-up duration did not allow for a definitive conclusion.
The 5-year estimated OS and EFS for children appeared to be much lower in the chemotherapy-only group than that in the HSCT group (Fig. 5). The majority of the clinical trials have demonstrated a consistent advantage for allogeneic HSCT in terms of disease-free survival (DFS), but not always for OS. The BFS 87 and 93 studies showed comparable DFS in high-risk patients receiving an allogeneic matched related donor HSCT in first CR and those receiving non-HSCT treatment (64.1% vs. 62.0%) [22]. A CCG 2891 study showed a significant survival advantage for allogenic transplantation compared to that for autologous transplantation (60% vs. 48%, P=0.002) and chemotherapy (60% vs. 53%, P=0.05) as post-remission treatment, but there was no advantage for autologous transplantation over intensive chemotherapy [25].
A myeloablative combination of chemotherapy followed by rescue with an infusion of HLA-matched stem cells to reconstitute the patient's BM is an effective approach to treat AML. However, this option is often not available, because HLA-matched family donors are found for only approximately 25% of patients. Recently, the results with HLA-matched unrelated donors are virtually equivalent to those with HLA-matched family donors [26]. Among 584 patients with AML in first CR having adverse cytogenetics at diagnosis, the 3-year leukemia-free survival was 42% for matched sibling donor, 34% for HLA-matched unrelated donor, and 29% for partially matched unrelated donor transplantation (P=0.08) [26].
In addition, unrelated cord blood transplantation is used as a therapeutic option in pediatric AML cases with extremely poor-prognosis and an absence of a HLA-identical sibling. The 5-year leukemia-free survival in the cord blood transplantation group was slightly better than that in the allogeneic matched sibling transplantation group in a Chinese study of children with high-risk or advanced AML (55.7% vs. 32.7%, P=0.08) [27].
In this study, matched sibling donor transplantation showed the best outcome followed by unrelated BM/PB, umbilical cord blood, and autologous blood transplantation modalities (Fig. 8). Since unrelated BM/PB or umbilical cord blood HSCT had better survival than did the chemotherapy-only group (Table 4), patients with adverse prognostic features may benefit from HSCTs, if any of the above HSCT donor modalities are available.
In this study, the 5-year OS was 70.3% for 2006–2015 (Fig. 3). This rate was similar to that of developed countries such as Japan (75%) [2], Europe (69%) [10] and the United States (64%) [9], but higher compared with that of developing countries in Asia, such as China (7-yr OS, 33%) [28] and Thailand (5-yr OS, 35%) [29] (although the study periods and follow-up durations were slightly different among these studies). These disparities may be caused by multiple factors, with the country's economic status being one contributor. During the last 2 decades in Korea, the gross national income per capita has increased by 240% [17]. With economic growth, children are more likely to have access to health insurance and to receive a timely diagnosis, high quality treatment, and supportive care, and parents are more likely to adhere to therapy, all of which contribute to improved survival rate of children with AML [30].
This study had several limitations, although “period” was included as an independent factor for multivariate analysis, unknown confounders might not be controlled because of the retrospective nature of the study. Another limitation was that the results may not represent Korean data because they were obtained from a single institution. Since childhood AML is a rare disease, further studies with a prospective, randomized, multi-institutional cohort are required to validate outcomes in Korean children with AML. Additional studies on genome-based, risk-directed treatment strategies for childhood AML are warranted.
References
1. Gamis AS, Alonzo TA, Perentesis JP, Meshinchi S. COG Acute Myeloid Leukemia Committee. Children's Oncology Group's 2013 blueprint for research: acute myeloid leukemia. Pediatr Blood Cancer. 2013; 60:964–971. PMID: 23255301.

2. Horibe K, Saito AM, Takimoto T, et al. Incidence and survival rates of hematological malignancies in Japanese children and adolescents (2006-2010): based on registry data from the Japanese Society of Pediatric Hematology. Int J Hematol. 2013; 98:74–88. PMID: 23702913.

3. Park HJ, Moon EK, Yoon JY, et al. Incidence and survival of childhood cancer in Korea. Cancer Res Treat. 2016; 48:869–882. PMID: 26790965.

4. Kömür M, Erbey F, Bayram I, Tanyeli A. Incidence and prognostic importance of molecular genetic defects in children with acute myeloblastic leukemia. Asian Pac J Cancer Prev. 2010; 11:1393–1395. PMID: 21198299.
5. Grimwade D, Walker H, Oliver F, et al. The importance of diagnostic cytogenetics on outcome in AML: analysis of 1,612 patients entered into the MRC AML 10 trial. The Medical Research Council Adult and Children's Leukaemia Working Parties. Blood. 1998; 92:2322–2333. PMID: 9746770.
6. Kim G, Lee HO, Choi JS, Baek HJ, Kook H. Characteristics and therapeutic outcomes of acute promyelocytic leukemia in children and adolescents. Clin Pediatr Hematol Oncol. 2016; 23:105–115.

7. ter Bals E, Kaspers GJ. Treatment of childhood acute myeloid leukemia. Expert Rev Anticancer Ther. 2005; 5:917–929. PMID: 16221060.

8. Gupta V. Alternative donor transplants for high-risk acute myeloid leukemia. Curr Opin Hematol. 2008; 15:115–120. PMID: 18300757.

9. Ward E, DeSantis C, Robbins A, Kohler B, Jemal A. Childhood and adolescent cancer statistics, 2014. CA Cancer J Clin. 2014; 64:83–103. PMID: 24488779.

10. Dama E, Pastore G, Mosso ML, et al. Time trends and prognostic factors for survival from childhood cancer: a report from the Childhood Cancer Registry of Piedmont (Italy). Eur J Pediatr. 2006; 165:240–249. PMID: 16411094.

11. Kang KS, Park JH, Lee JT, Lee KB. Survival rates of acute leukemia patients by FAB classification. Korean J Hematol. 1992; 27:239–247.
12. Lee DH, Chung NG, Cho B, et al. Idarubicin plus behenoyl cytarabine and 6-thioguanine compares favorably with idarubicin plus cytarabine-based regimen for children with previously untreated acute myeloid leukemia: 10-year retrospective, multicenter study in Korea. J Korean Med Sci. 2010; 25:9–15. PMID: 20052341.

13. Korean Statistical Information Service. The population census by age in Gwangju and Chonnam province of Korea (1996-2015). Daejeon, Korea: Korean Statistical Information Service;2015. Accessed February 2, 2016. at http://kosis.kr/eng/statisticsList/statisticsList_01List.jsp?vwcd=MT_ETITLE&parentId=A#SubCont.
14. Bennett JM, Catovsky D, Daniel MT, et al. Proposed revised criteria for the classification of acute myeloid leukemia. A report of the French-American-British Cooperative Group. Ann Intern Med. 1985; 103:620–625. PMID: 3862359.
15. O'Donnell MR, Abboud CN, Altman J, et al. NCCN Clinical Practice Guidelines acute myeloid leukemia. J Natl Compr Canc Netw. 2012; 10:984–1021. PMID: 22878824.
16. Burnett AK, Wheatley K, Goldstone AH, et al. The value of allogeneic bone marrow transplant in patients with acute myeloid leukaemia at differing risk of relapse: results of the UK MRC AML 10 trial. Br J Haematol. 2002; 118:385–400. PMID: 12139722.

17. Economic Statistics System. Annual gross national income per capita (1996-2015). Seoul, Korea: the Bank of Korea;2015. Accessed December 31, 2016. at http://ecos.bok.or.kr/jsp/vis/keystat/#/detail.
18. Park EH, Lee H, Won YJ, et al. Nationwide statistical analysis of myeloid malignancies in Korea: incidence and survival rate from 1999 to 2012. Blood Res. 2015; 50:204–217. PMID: 26770948.

19. Hjalgrim LL, Rostgaard K, Schmiegelow K, et al. Age- and sex-specific incidence of childhood leukemia by immunophenotype in the Nordic countries. J Natl Cancer Inst. 2003; 95:1539–1544. PMID: 14559876.

20. Viana MB, Cunha KC, Ramos G, Murao M. Acute myeloid leukemia in childhood: 15-year experience in a single institution. J Pediatr (Rio J). 2003; 79:489–496. PMID: 14685445.
21. Imamura T, Iwamoto S, Kanai R, et al. Outcome in 146 patients with paediatric acute myeloid leukaemia treated according to the AML99 protocol in the period 2003-06 from the Japan Association of Childhood Leukaemia Study. Br J Haematol. 2012; 159:204–210. PMID: 22924344.

22. Creutzig U, Zimmermann M, Ritter J, et al. Treatment strategies and long-term results in paediatric patients treated in four consecutive AML-BFM trials. Leukemia. 2005; 19:2030–2042. PMID: 16304570.

23. Klein K, Kaspers G, Harrison CJ, et al. Clinical impact of additional cytogenetic aberrations, cKIT and ras mutations, and treatment elements in pediatric t(8;21)-AML: results from an International Retrospective Study by the International Berlin-Frankfurt-Münster Study Group. J Clin Oncol. 2015; 33:4247–4258. PMID: 26573082.

24. Park HS, Kim DW, Kim CC, et al. Induction chemotherapy with idarubicin plus N4-behenoyl-1-beta-D-arabinofuranosylcytosine in acute myelogenous leukemia: a newly designed induction regimen--a prospective, cooperative multicenter study. Semin Hematol. 1996; 33(4 Suppl 3):24–29.
25. Woods WG, Neudorf S, Gold S, et al. A comparison of allogeneic bone marrow transplantation, autologous bone marrow transplantation, and aggressive chemotherapy in children with acute myeloid leukemia in remission. Blood. 2001; 97:56–62. PMID: 11133742.
26. Gupta V, Tallman MS, He W, et al. Comparable survival after HLA-well-matched unrelated or matched sibling donor transplantation for acute myeloid leukemia in first remission with unfavorable cytogenetics at diagnosis. Blood. 2010; 116:1839–1848. PMID: 20538804.

27. Zheng C, Zhu X, Tang B, et al. Comparative analysis of unrelated cord blood transplantation and HLA-matched sibling hematopoietic stem cell transplantation in children with high-risk or advanced acute leukemia. Ann Hematol. 2015; 94:473–480. PMID: 25217231.

28. Xu XJ, Tang YM, Song H, Yang SL, Shi SW, Wei J. Long-term outcome of childhood acute myeloid leukemia in a developing country: experience from a children's hospital in China. Leuk Lymphoma. 2010; 51:2262–2269. PMID: 20929322.

29. Wiangnon S, Veerakul G, Nuchprayoon I, et al. Childhood cancer incidence and survival 2003-2005, Thailand: study from the Thai Pediatric Oncology Group. Asian Pac J Cancer Prev. 2011; 12:2215–2220. PMID: 22296359.
30. Chow EJ, Puumala SE, Mueller BA, et al. Childhood cancer in relation to parental race and ethnicity: a 5-state pooled analysis. Cancer. 2010; 116:3045–3053. PMID: 20564410.
Fig. 3
The 5-year Kaplan-Meier estimated (K-M) overall survival (OS) (A) and event-free survival (EFS) (B) for 110 childhood acute myeloid leukemia cases acute promyelocytic leukemia. The OS (C) and EFS (D) were compared according to study period.
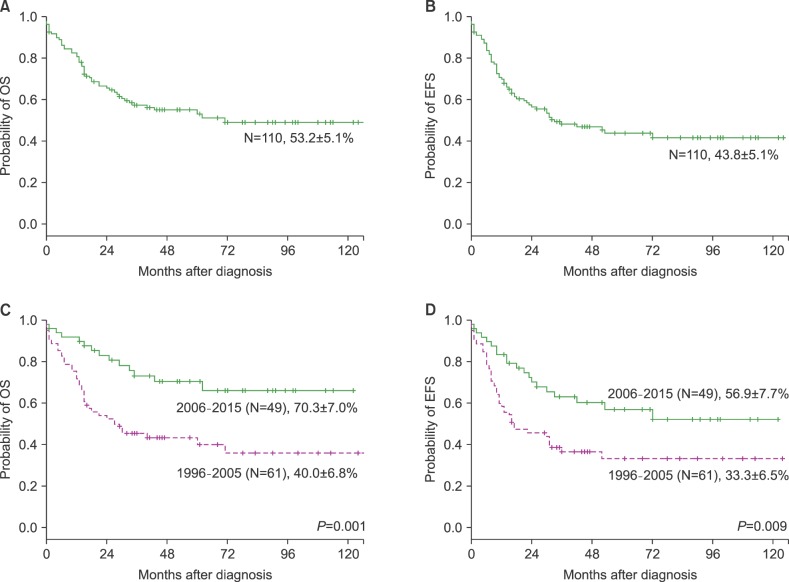
Fig. 4
The 5-year Kaplan-Meier overall survival (K-M OS) (A) and event-free survival (EFS) (B) for 91 childhood acute myeloid leukemia cases, excluding acute promyelocytic leukemia. The OS (C) and EFS (D) were compared according to study period.
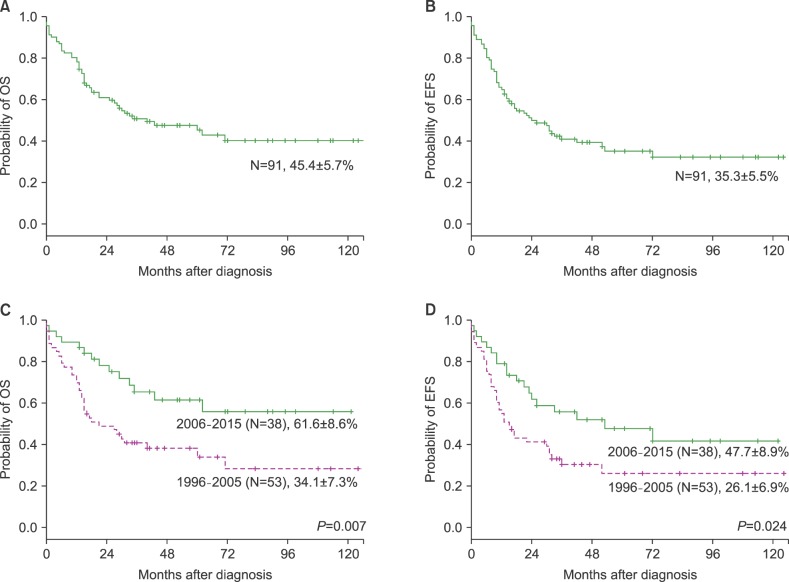
Fig. 5
The 2-year Kaplan-Meier overall survival (K-M OS) (A) and event-free survival (EFS) (B) for 91 childhood acute myeloid leukemia cases by induction regimen.
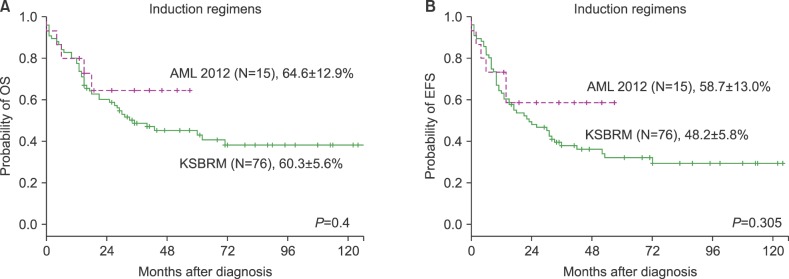
Fig. 6
The 5-year Kaplan-Meier overall survival (K-M OS) (A) and event-free survival (EFS) (B) for 91 childhood acute myeloid leukemia cases by cytogenetic prognostic group.
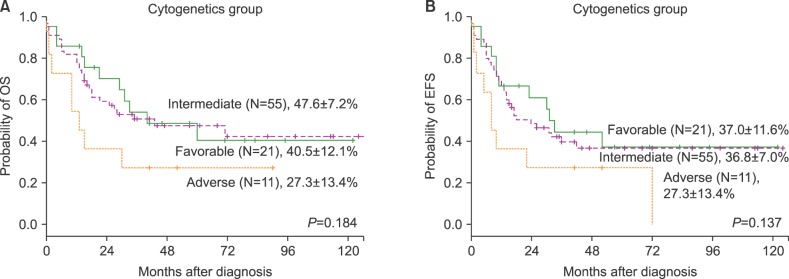
Fig. 7
The 5-year Kaplan-Meier overall survival (K-M OS) for 91 childhood acute myeloid leukemia cases by treatment modality.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download