TO THE EDITOR: B-cell non-Hodgkin lymphoma (B-NHL)
comprises a heterogeneous group of neoplasms [1]. Traditionally, marrow involvement of NHL has been detected by examining bone marrow (BM) samples by microscopy [2]. However, even if BM samples do not show malignant lymphoid aggregates, this may not reflect the status of the entire bone marrow. Recently, diagnostic hematology has expanded with the introduction of new molecular technologies. BIOMED-2 multiplex polymerase chain reaction (PCR) (InVivoScribe Technologies, San Diego, CA, USA) has been applied to identify immunoglobulin (Ig) genes and T cell receptor (TCR) gene clonality in clinical specimens [34].
The purpose of this study was to compare the utility of an Ig rearrangement assay based on BIOMED-2 multiplex PCR in detecting BM involvement in B-NHL with that of microscopic examination and positron emission tomography with computed tomography (PET-CT). A total of 28 patients (median age, 59 yrs; range, 37–95 yrs) who were diagnosed with B-NHL between January 2007 and March 2010 at Kangdong Sacred Heart Hospital, Seoul, Korea were enrolled in the study, which included 17 men and 11 women, whose histopathological characteristics are listed in Table 1. DNA was extracted from the BM aspirations from each patient according to a previously reported method [5].
We performed a BIOMED-2 multiplex PCR assay using an IdentiClone Ig (IgH: immunoglobulin heavy chain, IGK: immunoglobulin kappa, IGL: immunoglobulin lambda) Gene Clonality Assay Kit (InVivoScribe Technologies, San Diego, CA, USA). The full study comprised the use of five kits targeting IGH (IGHA: VHFR1-JH; IGHB: VHFR2-JH; IGHC: VHFR3-JH; IGHD:DH1–6-JH; and IGHE: DH7-JH), two kits targeting IGK (IGKA: Vκ-Jκ; IGKB: Vκ-Kde; and JκCκ intron-Kde), and one kit targeting IGL (Vλ-Jλ). When the first IGH test performed was negative, the IGK and IGL tests followed. Generally, PCR sensitivity is influenced by the primers used, and in the past, the most common PCR method for B-cell Ig genes amplified CDR3 regions, using FR3 and JH consensus primers [6]. Unlike other PCR methods that target only the FR3 region for IGH gene rearrangement, the BIOMED-2 multiplex PCR test uses variable target gene rearrangement of 5' primers to target FR1, 2, and 3 of the V-J and D-J regions of IGH. After PCR amplification, a heteroduplex analysis was performed. In this method, PCR products are heat-denatured and cold-renatured to form duplexes (hetero- or homo-duplexes). Then, polyacrylamide gels were used to visualize monoclonal bands upon electrophoresis at room temperature.
In our study, the overall concordance rate between the results of microscopic BM examination and IG rearrangement assay was 96.4% (27/28). Ten cases were found positive for Ig gene rearrangement (Table 1). Nine cases revealed microscopic BM infiltration; case 10 did not (Table 2). Eight of the 10 Ig rearrangements were IGH-positive, 5 were positive for IGHA, and 6 were positive for IGHC (Table 2). Similarly, a study by Abbas et al. [7], using a BIOMED-2 kit to assess B-cell gene rearrangements in leukemias and lymphomas, showed that 92% of cases had IGH clonality, with 74% detected by IGHA, 75.5% by IGHB, 65.1% IGHC, 26% by IGHD, and 2.1% by IGHE.
In our study, two DLBCL cases (33.3%, 2/6) with negative IGH tests showed positive results in IGK tests. This result is in line with a report by van Krieken et al. [4], which indicated that for DLBCL, an IGH test alone may not be sufficient to detect monoclonality. With IGH testing, the monoclonal detection rate was approximately 85%, and the use of additional IGK kits increased the detection rate to about 98%. Additionally, we detected monoclonality using only IGH tests in cases of nodal marginal zone B-cell lymphoma, mantle cell lymphoma, and small lymphocytic lymphoma, and these results were consistent with those of this report. Therefore, we suggest that in the case of DLBCL, both IGH and IGK tests be applied to detect BM involvement. The IGHD test was positive in two cases (cases 5 and 6) that were also positive for the IGHC test (Table 2). Two cases showed monoclonality in IGK tests, but not in IGH tests. This result showed that IGK tests are reliable and useful for the detection of Ig gene rearrangements in cases where they were not detected by IGH tests.
Therefore, we suggest that IGHA, IGHB, and IGHC IGH tests, together with IGKA, and IGKB IGK tests should be considered as efficient Ig clonality assays. In negative cases, the application of additional IGHD and IGHE IGH tests and IGL tests need to be considered.
Interestingly, one case (case 10) showed a discrepant result: it was microscopically normal and positive for monoclonality by IGH tests (IGHB and IGHC). The case also showed 18-F fluorodeoxyglucose (FDG) hot uptake in BM in a PET-CT analysis (Table 2). Therefore, PET-CT was confirmed to be helpful in determining BM involvement in lymphoma [8].
With regard to minimal residual disease (MRD), Brisco et al. [9] reported that the IGH gene rearrangement assay would be useful in monitoring of MRD in B-cell lymphoblastic leukemia, and if a case did not show BM involvement morphologically but showed monoclonality in IGH tests, it would be associated with poor prognosis and a high-risk relapse rate. We also followed one case with microscopic involvement and monoclonality detected in IGK tests but not in IGH tests (case 9). Complete hematological remission was achieved, based on BM microscopic examination, after chemotherapy. The case exhibited negative result on Ig gene rearrangement assays (IGH, IGK and IGL). Therefore, discrepancy cases need to be followed closely.
Recently, there was another study using BIOMED-2 kits and the heteroduplex method on formalin-fixed paraffin-embedded tissue from Hodgkin's lymphoma (HL) cases. IGK and IGL gene rearrangement assays were found to be reliable methods that increased the clonality detection rate. Of the HL cases tested, 94% were found positive for clonality [10].
On the whole, this study showed a high concordance rate (96.4%, 27/28) between the results of microscopic BM examination and Ig gene rearrangement assay. These results are in line with those of Shin et al. [11], which indicated a relatively high concordance rate (70.6%, 84/119) in B-cell neoplasias. We recommend simultaneous application of both BM microscopy and Ig gene rearrangement assays to more accurately diagnose and determine the prognosis of cases. Henceforth, more data on the discrepancy between BM exam and clonality assay should be accumulated; it will be helpful to make a therapeutic decision or develop a protocol. Additionally, we found a concordance rate of 96% (24/25) between results of the Ig gene rearrangement assay and PET-CT, although three cases were not examined by PET-CT (data not shown). A limitation in our research was that we could not compare our data with that of the capillary EP method by nucleotide sequencing to detect monoclonality in malignant lymphomas. We believe that application of this method might have improved the sensitivity and specificity of diagnosis of B-NHL.
In this study, we evaluated the utility of multiplex PCR-based Ig gene rearrangement assay in detecting BM involvement in malignant lymphoma. When it is difficult to detect BM involvement in malignant lymphoma based on morphology, the Ig gene rearrangement assay can provide more accurate information regarding BM involvement in malignant lymphomas.
Figures and Tables
Table 1
Concordance between morphology and PCR-determined clonality of bone marrow, based on histology in cases of non-Hodgkin lymphoma.

Table 2
Diagnosis of review panel samples showing clonal immunoglobulin gene rearrangements.
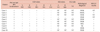
Abbreviations: DLBL, diffuse large B-cell lymphoma; IGH, immunoglobulin heavy chain gene rearrangement study; IGK, immunoglobulin light kappa chain gene rearrangement study; MALT, MALT type lymphoma; MCL, mantle cell lymphoma; NMZL, nodal marginal zone B-cell lymphoma; NT, not tested; SLL, small lymphocytic lymphoma.
References
1. Lossos IS. Molecular pathogenesis of diffuse large B-cell lymphoma. J Clin Oncol. 2005; 23:6351–6357.

2. Kang YH, Park CJ, Seo EJ, et al. Polymerase chain reaction-based diagnosis of bone marrow involvement in 170 cases of non-Hodgkin lymphoma. Cancer. 2002; 94:3073–3082.

3. Sandberg Y, van Gastel-Mol EJ, Verhaaf B, Lam KH, van Dongen JJ, Langerak AW. BIOMED-2 multiplex immunoglobulin/T-cell receptor polymerase chain reaction protocols can reliably replace Southern blot analysis in routine clonality diagnostics. J Mol Diagn. 2005; 7:495–503.

4. van Krieken JH, Langerak AW, Macintyre EA, et al. Improved reliability of lymphoma diagnostics via PCR-based clonality testing: report of the BIOMED-2 Concerted Action BHM4-CT98-3936. Leukemia. 2007; 21:201–206.

5. Fey MF, Pilkington SP, Summers C, Wainscoat JS. Molecular diagnosis of haematological disorders using DNA from stored bone marrow slides. Br J Haematol. 1987; 67:489–492.

6. Odenthal M, Siebolts U, Ernestus K, Disse D, Dienes HP, Wickenhauser C. Immunoglobulin heavy chain gene analysis in bone marrow biopsies and corresponding lymph node specimens: dependency on pre-treatment, histological subtype and extension of B-cell lymphoma. Int J Mol Med. 2008; 21:569–576.

7. Abbas F, Yazbek SN, Shammaa D, Hoteit R, Fermanian P, Mahfouz R. Invivoscribe BIOMED-2 primer mixes in B-cell immunoglobulin gene rearrangement studies: experience of a molecular diagnostics laboratory in a major tertiary care center. Genet Test Mol Biomarkers. 2014; 18:787–790.

8. Cheson BD. Role of functional imaging in the management of lymphoma. J Clin Oncol. 2011; 29:1844–1854.

9. Brisco MJ, Latham S, Sutton R, et al. Determining the repertoire of IGH gene rearrangements to develop molecular markers for minimal residual disease in B-lineage acute lymphoblastic leukemia. J Mol Diagn. 2009; 11:194–200.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download