Abstract
Background
The rectum is a relatively uncommon site for lymphoma compared with other gastrointestinal sites; no consensus regarding management of primary rectal lymphoma (PRL) has been formed due to its limited frequency. We aimed to investigate clinical characteristics and treatment outcomes in patients with PRL in a single center patient cohort.
Methods
We retrospectively analyzed the results of 16 consecutive patients with PRL, identified and treated at the Asan Medical Center, Seoul, Korea between January 1993 and December 2014.
Results
These 16 patients with PRL constituted 0.8% of all non-Hodgkin's lymphoma patients (N=1,984). B-cell lymphomas (N=14) made up the majority of the series, and half of these were extranodal marginal zone lymphomas (ENMZL, N=7). Ten patients received systemic chemotherapy with (N=3) or without rituximab (N=7), and 4 of these received additional local therapy. The others received radiotherapy (N=3) or endoscopic mucosal resection (N=3). Twelve patients (75%) achieved complete response (CR) after first-line treatment. Event-free survival (EFS) and overall survival (OS) in stages IE and IIE were significantly longer compared with stages IVE (P=0.001 and P=0.001, respectively). All patients with ENMZL (N=7) achieved CR during or after initial treatment.
Non-Hodgkin's lymphoma (NHL) originates in the lymph nodes or other lymphoid tissues. However, a significant proportion of NHL occurs in extranodal sites such as the gastrointestinal tract, skin, or central nervous system. Primary gastrointestinal (GI) NHL is the most common form of extranodal NHL, constituting around one-third of all extranodal cases in most series [1]. Primary GI NHL, which accounts for 5% of all lymphomas, involves the alimentary tract and shows symptoms of GI involvement at presentation [2]. Of note, 20–30% of cases involve the colon or the rectum [34]. Nonetheless, primary GI NHL is an uncommon disorder, accounting for 0.05% of all colonic neoplasms and 0.1% of primary rectal tumors [5].
Primary rectal lymphoma (PRL), in particular, has been insufficiently addressed due to its infrequent occurrence. While treatment strategies in nodal NHL are well established, those for GI NHL, particularly PRL, remain debatable and controversial. Because of the uncommon nature of this cancer, very few studies have investigated prognostic factors that will allow clinicians to determine outcome and risk for relapse [678].
In the current study, we reviewed our experience with PRL and aimed to investigate clinical characteristics, treatment, and outcome in patients with PRL.
We performed a retrospective review of all cases of PRL (N=16) seen at the Asan Medical Center (Seoul, Korea) since 1993. For each case, we reviewed demographic information as well as medical records regarding symptoms at presentation, diagnosis, histological features, treatment, and follow-up. This study was reviewed and approved by the Asan Medical Center Institutional Review Board.
Primary GI NHL was defined according to the Lewin criteria [2]: patients were required to present with GI symptoms of or predominant lesions in the GI tract. A staging evaluation was performed according to the Ann Arbor staging system. This involved performing a physical examination; determining complete blood counts and differential white blood cell counts; assessing the biochemical profile including serum lactate dehydrogenase (LDH) levels; and performing a bilateral bone marrow aspiration and biopsy, a computed tomography (CT) scan of the neck, thorax, abdomen and pelvis, and whole-body positron emission tomography. Esophagogastroduodenoscopy, colonoscopy, and lumbar puncture were performed when indicated based on clinical suspicion.
Response criteria and endpoints are reported according to published guidelines [9]. Event-free survival (EFS) was calculated as the period of time from the date of diagnosis to the date of recurrence or death from any cause. Overall survival (OS) was calculated as the period from the date of diagnosis to the date of death from any cause. Both EFS and OS were estimated using the Kaplan-Meier method. Two-sided P-values less than 0.05 were considered significant. All statistical analyses were performed with SPSS, version 18.0 (SPSS Inc., Chicago, IL, USA).
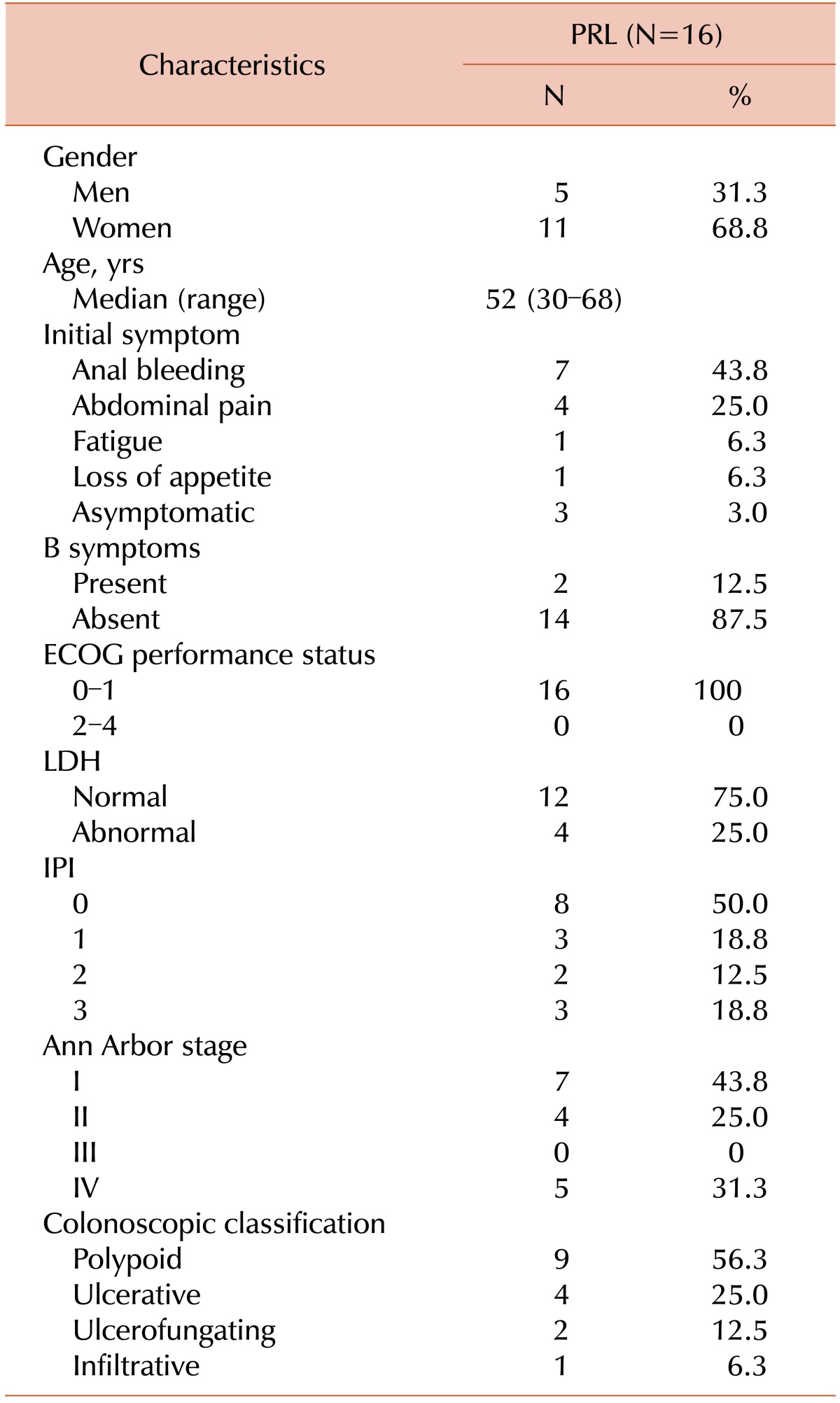
A total of 16 patients with PRL were included in this study. The median follow-up time was 30.4 months (range, 4.5 to 126.8 mo) from the first day of diagnosis. During this time, 1984 cases of NHL were diagnosed within the registry of the Asan Medical Center; thus, the PRL cases represented 0.8% of all NHL cases. The median age at presentation was 52 years (range, 30 to 68 yrs). Women represented the majority of patients (68.8%). The clinical features of all patients are listed in Table 1.
Anal bleeding that required the patient to seek medical attention was a predominant finding on presentation (43.8%). “B” symptoms occurred in only 12.5% of patients.
Colonoscopic examinations were performed in all patients. We classified colonoscopic tumor morphologies into four categories as follows: polypoid (56.3%), ulcerative (25.0%), ulcerofungating (12.5%), and infiltrative lesions (6.3%). For extranodal marginal zone lymphoma, the most common colonoscopic classification was the polypoid lesion (85.7%). For other histological subtypes, however, the most common cases were ulcerative or ulcerofungating lesions (55.6%).
Review of pathology reports revealed that B-cell lymphomas (N=14) made up majority of the series. Half (N=7) of these B-cell lymphomas were extranodal marginal zone lymphomas (ENMZL). The others were diffuse large B-cell lymphomas (DLBCL, N=4) and mantle cell lymphomas (MCL, N=3). A small number of patients had features of T-cell lymphomas (N=2). One was found to be enteropathy-associated T-cell lymphoma (EATL), and the other was NK/T-cell lymphoma (NKTCL).
The proportion of stage I disease (limited to the rectal wall, without nodal involvement) was 43.8%, and that of stage II disease (limited to the rectal wall, with nodal involvement) was 25%. ENMZL and DLBCL were localized in all cases (stage IE: 7, stage IIE: 4). A tendency toward greater spread could be observed in MCL and T-cell lymphoma, which were predominantly stage IVE (N=5).
Involvement of non-lymphatic or non-GI sites occurred in 5 patients (stage IVE). The most frequently involved site was the spleen (N=3), followed by the bone marrow (N=2).
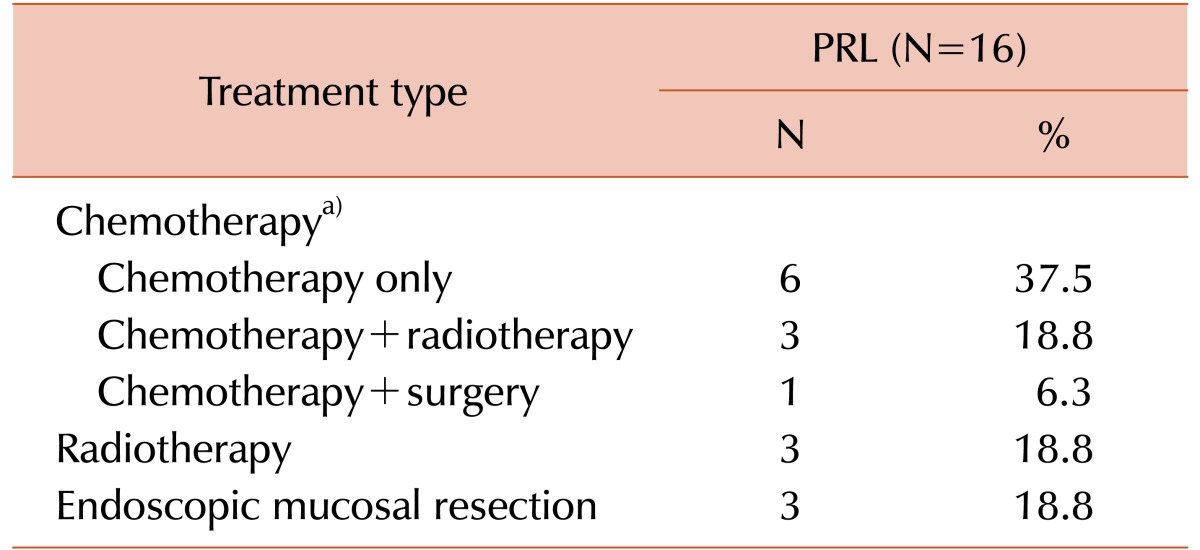
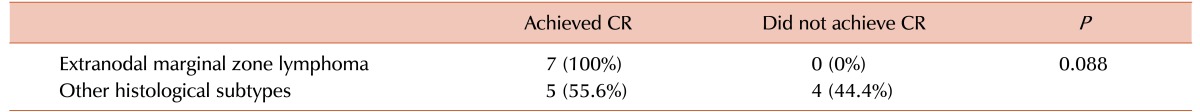
Ten patients were administered systemic chemotherapy with (N=3) or without rituximab (N=7), and 4 of these patients received additional local therapy including radiotherapy (N=3) or surgical resection (N=1). The other patients were treated with radiotherapy (N=3) or endoscopic mucosal resection (N=3) as their first-line therapies, sparing systemic chemotherapy (Table 2). Twelve patients (75%) achieved complete response (CR) following first-line treatment. In particular, all patients with ENMZL (N=7) achieved CR during or after initial treatment, while 5 of 9 patients with the other histologic subtypes achieved CR (100% vs. 55.6%, respectively; P=0.088, Table 3).
After the median follow-up of 77.9 months (range, 4.5–174.4 mo), 4 patients died and 4 patients experienced progression. Among all patients, the 5-year event-free survival (EFS) rate was 73.7% and the 5-year overall survival (OS) rate was 67.7%.
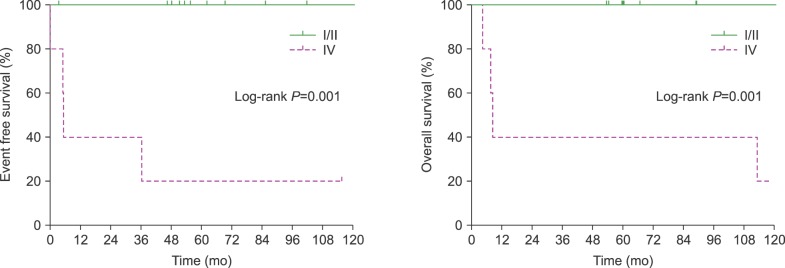
The EFS and OS for patients in stages IE and IIE were significantly longer compared with those of patients in stage IVE (P=0.001 and P=0.001, respectively, Fig. 1). The median EFS and OS for patients in stage IVE were 5.3 months and 8.5 months, respectively. Neither median EFS nor OS was reached in patients with stage IE/IIE disease.
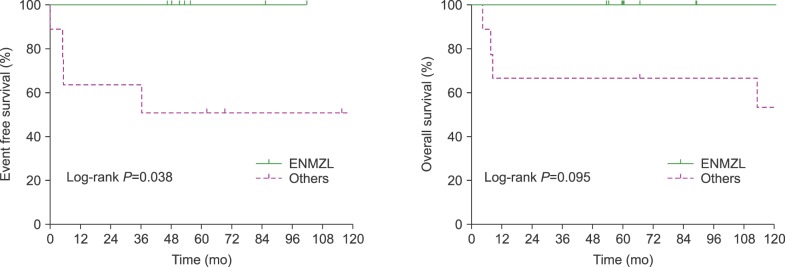
It was possible to detect an influence of histologic subtype in PRL. Considered according to histological subtype, EFS and OS tended to be longer in patients with ENMZL than in those with other histologic subtypes (Fig. 2).
PRL usually presents with signs and symptoms suggestive of primary rectal carcinoma. Patient with rectal lymphoma usually seek treatment because of anal bleeding or abdominal pain. It has been reported that the majority of patients who have symptoms report abdominal pain, nausea, vomiting, fever, and weight loss [45].
Kim et al. [10] conducted a study on primary colon lymphoma in Korea. They analyzed the colonoscopic images and classified them into five categories. For B-cell lymphomas, the most common endoscopic type was the fungating mass, whereas for T-cell lymphomas, the most common types were ulcerative or ulceroinfiltrative lesions. In the present study, the colonoscopic appearance differed between ENMZL and other histological subtypes.
The treatment for gastrointestinal lymphomas remains uncertain. Some studies have suggested that the appropriate primary treatment is to attempt resection when the disease is judged to be resectable, because patients with residual disease had a poor prognosis [111213]. Other series have suggested radiotherapy or chemotherapy as the treatment of choice, because patients with residual diseases after surgery had a poor prognosis, and adjuvant treatment will increase EFS [1415].
In the present study, the most frequent subtype was ENMZL, and the second most common subtype was DLBCL, which was observed in 25% of cases. We analyzed the effect of variable subtypes on prognosis. Although the univariate analyses revealed no significant differences related to survival, the prognosis of patients with ENMZL tended to be better than that of others.
We observed a significant difference in survival between patients with early disease, stages I through II, compared with those with late disease, stage IV. We can assume that stage is a good predictor of survival in PRL.
Malignant lymphoma of the rectum should be considered a different clinicopathological entity with different behavior and clinical presentation, and treatment should be defined based on this special clinical condition. The therapeutic experience in this selected group of patients is limited, because even in large tertiary referral centers, the number of cases is small (0.8% in our institution).
There are some limitations of our study. First, the number of cases in this study was relatively small. Owing to the rarity of this malignancy, nationwide, international, or multicenter enrollment over a longer period may be required to obtain sufficient patient numbers for adequate statistical analysis. Secondly, all of the patients received CHOP-based chemotherapy regimens. Further studies with long-term follow-up are needed to clarify the role of CHOP or other systemic regimens in PRL.
In summary, in the present study, PRL was seen to be very rare, and appeared to be mostly B-cell type. Stage is the most important prognostic factor, with significantly better survival observed with localized disease. ENMZL may be one of the most common types of PRL, with favorable treatment outcome.
References
1. Zucca E, Roggero E, Bertoni F, Cavalli F. Primary extranodal non-Hodgkin's lymphomas. Part 1: Gastrointestinal, cutaneous and genitourinary lymphomas. Ann Oncol. 1997; 8:727–737. PMID: 9332679.

2. Lewin KJ, Ranchod M, Dorfman RF. Lymphomas of the gastrointestinal tract: a study of 117 cases presenting with gastrointestinal disease. Cancer. 1978; 42:693–707. PMID: 354774.
3. Dragosics B, Bauer P, Radaszkiewicz T. Primary gastrointestinal non-Hodgkin's lymphomas. A retrospective clinicopathologic study of 150 cases. Cancer. 1985; 55:1060–1073. PMID: 3881161.

4. Henry CA, Berry RE. Primary lymphoma of the large intestine. Am Surg. 1988; 54:262–266. PMID: 3364860.
5. Dodd GD. Lymphoma of the hollow abdominal viscera. Radiol Clin North Am. 1990; 28:771–783. PMID: 2190270.
6. Chihara D, Kagami Y, Oki Y, et al. R-CHOP therapy for MALT lymphoma of the rectum. Eur J Haematol. 2010; 84:84–86. PMID: 19737307.

7. Unal B, Karabeyoglu M, Erel S, Bozkurt B, Kocer B, Cengiz O. Primary rectal lymphoma: an unusual treatment for a rare case. Postgrad Med J. 2008; 84:333–335. PMID: 18644928.

8. Bilsel Y, Balik E, Yamaner S, Bugra D. Clinical and therapeutic considerations of rectal lymphoma: a case report and literature review. World J Gastroenterol. 2005; 11:460–461. PMID: 15637770.

9. Cheson BD, Horning SJ, Coiffier B, et al. NCI Sponsored International Working Group. Report of an international workshop to standardize response criteria for non-Hodgkin's lymphomas. J Clin Oncol. 1999; 17:1244. PMID: 10561185.

10. Kim YH, Lee JH, Yang SK, et al. Primary colon lymphoma in Korea: a KASID (Korean Association for the Study of Intestinal Diseases) Study. Dig Dis Sci. 2005; 50:2243–2247. PMID: 16416168.

11. Fan CW, Changchien CR, Wang JY, et al. Primary colorectal lymphoma. Dis Colon Rectum. 2000; 43:1277–1282. PMID: 11005497.

12. Shepherd FA, Evans WK, Kutas G, et al. Chemotherapy following surgery for stages IE and IIE non-Hodgkin's lymphoma of the gastrointestinal tract. J Clin Oncol. 1988; 6:253–260. PMID: 3339394.

13. Lai YL, Lin JK, Liang WY, Huang YC, Chang SC. Surgical resection combined with chemotherapy can help achieve better outcomes in patients with primary colonic lymphoma. J Surg Oncol. 2011; 104:265–268. PMID: 21472731.

14. Bellesi G, Alterini R, Messori A, et al. Combined surgery and chemotherapy for the treatment of primary gastrointestinal intermediate- or high-grade non-Hodgkin's lymphomas. Br J Cancer. 1989; 60:244–248. PMID: 2765374.

15. Rackner VL, Thirlby RC, Ryan JA Jr. Role of surgery in multimodality therapy for gastrointestinal lymphoma. Am J Surg. 1991; 161:570–575. PMID: 2031540.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download