1. Lang P, Teltschik HM, Feuchtinger T, et al. Transplantation of CD3/CD19 depleted allografts from haploidentical family donors in paediatric leukaemia. Br J Haematol. 2014; 165:688–698. PMID:
24588540.
2. Im HJ, Koh KN, Suh JK, et al. Refinement of treatment strategies in ex vivo T-cell-depleted haploidentical SCT for pediatric patients. Bone Marrow Transplant. 2015; 50:225–231. PMID:
25310303.

3. Airoldi I, Bertaina A, Prigione I, et al. γδT-cell reconstitution after HLA-haploidentical hematopoietic transplantation depleted of TCR-αβ+/CD19+ lymphocytes. Blood. 2015; 125:2349–2358. PMID:
25612623.
4. Chang YJ, Huang XJ. Improving the clinical outcome of unmanipulated haploidentical blood and marrow transplantation. Bone Marrow Transplant. 2015; 50(Suppl 2):S21–S23. PMID:
26039202.

5. Fuchs EJ. HLA-haploidentical blood or marrow transplantation with high-dose, post-transplantation cyclophosphamide. Bone Marrow Transplant. 2015; 50(Suppl 2):S31–S36. PMID:
26039204.

6. Apperley J, Niederwieser D, Huang XJ, et al. Reprint of: haploidentical hematopoietic stem cell transplantation: A global overview comparing Asia, the European Union, and the United States. Biol Blood Marrow Transplant. 2016; 22(Suppl 3):S15–S18. PMID:
26899273.

7. Ciurea SO, Bayraktar UD. "No donor"? Consider a haploidentical transplant. Blood Rev. 2015; 29:63–70. PMID:
25307958.

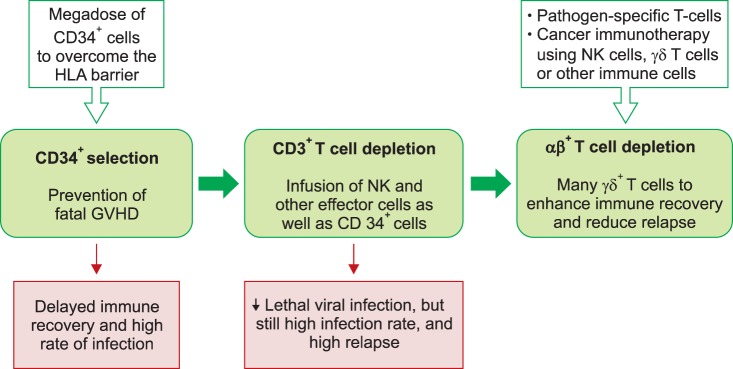
8. Or-Geva N, Reisner Y. The evolution of T-cell depletion in haploidentical stem-cell transplantation. Br J Haematol. 2016; 172:667–684. PMID:
26684279.

9. Booth C, Lawson S, Veys P. The current role of T cell depletion in paediatric stem cell transplantation. Br J Haematol. 2013; 162:177–190. PMID:
23718232.

10. Lang P, Mueller I, Greil J, et al. Retransplantation with stem cells from mismatched related donors after graft rejection in pediatric patients. Blood Cells Mol Dis. 2008; 40:33–39. PMID:
17884640.

11. Yoshihara S, Ikegame K, Taniguchi K, et al. Salvage haploidentical transplantation for graft failure using reduced-intensity conditioning. Bone Marrow Transplant. 2012; 47:369–373. PMID:
21478920.

12. Park JA, Koh KN, Choi ES, et al. Successful rescue of early graft failure in pediatric patients using T-cell-depleted haploidentical hematopoietic SCT. Bone Marrow Transplant. 2014; 49:270–275. PMID:
24141651.

13. Rådestad E, Wikell H, Engström M, et al. Alpha/beta T-cell depleted grafts as an immunological booster to treat graft failure after hematopoietic stem cell transplantation with HLA-matched related and unrelated donors. J Immunol Res. 2014; 2014:578741. PMID:
25371909.

14. Powles RL, Morgenstern GR, Kay HE, et al. Mismatched family donors for bone-marrow transplantation as treatment for acute leukaemia. Lancet. 1983; 1:612–615. PMID:
6131300.

15. Beatty PG, Clift RA, Mickelson EM, et al. Marrow transplantation from related donors other than HLA-identical siblings. N Engl J Med. 1985; 313:765–771. PMID:
3897863.

16. Anasetti C, Amos D, Beatty PG, et al. Effect of HLA compatibility on engraftment of bone marrow transplants in patients with leukemia or lymphoma. N Engl J Med. 1989; 320:197–204. PMID:
2643045.

17. Anasetti C, Beatty PG, Storb R, et al. Effect of HLA incompatibility on graft-versus-host disease, relapse, and survival after marrow transplantation for patients with leukemia or lymphoma. Hum Immunol. 1990; 29:79–91. PMID:
2249952.

18. Ash RC, Horowitz MM, Gale RP, et al. Bone marrow transplantation from related donors other than HLA-identical siblings: effect of T cell depletion. Bone Marrow Transplant. 1991; 7:443–452. PMID:
1873591.
19. Lang P, Schumm M, Greil J, et al. A comparison between three graft manipulation methods for haploidentical stem cell transplantation in pediatric patients: preliminary results of a pilot study. Klin Padiatr. 2005; 217:334–338. PMID:
16307419.

20. Bethge WA, Faul C, Bornhäuser M, et al. Haploidentical allogeneic hematopoietic cell transplantation in adults using CD3/CD19 depletion and reduced intensity conditioning: an update. Blood Cells Mol Dis. 2008; 40:13–19. PMID:
17869547.

21. Handgretinger R, Chen X, Pfeiffer M, et al. Feasibility and outcome of reduced-intensity conditioning in haploidentical transplantation. Ann N Y Acad Sci. 2007; 1106:279–289. PMID:
17442774.

22. Lang P, Handgretinger R. Haploidentical SCT in children: an update and future perspectives. Bone Marrow Transplant. 2008; 42(Suppl 2):S54–S59. PMID:
18978746.

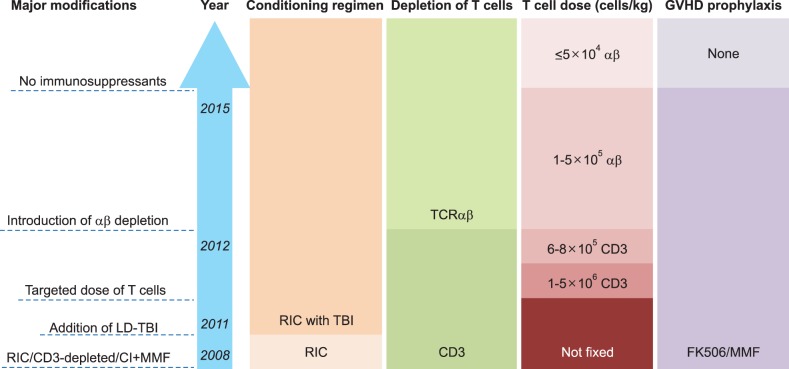
23. Handgretinger R, Lang P. The history and future prospective of haplo-identical stem cell transplantation. Cytotherapy. 2008; 10:443–451. PMID:
18615344.

24. Daniele N, Scerpa MC, Caniglia M, et al. Transplantation in the onco-hematology field: focus on the manipulation of αβ and γδ T cells. Pathol Res Pract. 2012; 208:67–73. PMID:
22115749.

25. Minculescu L, Sengeløv H. The role of gamma delta T cells in haematopoietic stem cell transplantation. Scand J Immunol. 2015; 81:459–468. PMID:
25753378.

26. Gordon PR, Leimig T, Mueller I, et al. A large-scale method for T cell depletion: towards graft engineering of mobilized peripheral blood stem cells. Bone Marrow Transplant. 2002; 30:69–74. PMID:
12132044.

27. Barfield RC, Otto M, Houston J, et al. A one-step large-scale method for T- and B-cell depletion of mobilized PBSC for allogeneic transplantation. Cytotherapy. 2004; 6:1–6. PMID:
14985161.

28. Handgretinger R, Klingebiel T, Lang P, et al. Megadose transplantation of purified peripheral blood CD34(+) progenitor cells from HLA-mismatched parental donors in children. Bone Marrow Transplant. 2001; 27:777–783. PMID:
11477433.
29. Lang P, Greil J, Bader P, et al. Long-term outcome after haploidentical stem cell transplantation in children. Blood Cells Mol Dis. 2004; 33:281–287. PMID:
15528145.

30. Locatelli F, Pende D, Maccario R, Mingari MC, Moretta A, Moretta L. Haploidentical hemopoietic stem cell transplantation for the treatment of high-risk leukemias: how NK cells make the difference. Clin Immunol. 2009; 133:171–178. PMID:
19481979.

31. Bader P, Soerensen J, Jarisch A, et al. Rapid immune recovery and low TRM in haploidentical stem cell transplantation in children and adolescence using CD3/CD19-depleted stem cells. Best Pract Res Clin Haematol. 2011; 24:331–337. PMID:
21925086.

32. Palma J, Salas L, Carrión F, et al. Haploidentical stem cell transplantation for children with high-risk leukemia. Pediatr Blood Cancer. 2012; 59:895–901. PMID:
22238059.

33. González-Vicent M, Molina B, Andión M, et al. Allogeneic hematopoietic transplantation using haploidentical donor vs. unrelated cord blood donor in pediatric patients: a single-center retrospective study. Eur J Haematol. 2011; 87:46–53. PMID:
21692851.

34. Pérez-Martínez A, González-Vicent M, Valentín J, et al. Early evaluation of immune reconstitution following allogeneic CD3/CD19-depleted grafts from alternative donors in childhood acute leukemia. Bone Marrow Transplant. 2012; 47:1419–1427. PMID:
22410752.

35. Dufort G, Pisano S, Incoronato A, et al. Feasibility and outcome of haploidentical SCT in pediatric high-risk hematologic malignancies and Fanconi anemia in Uruguay. Bone Marrow Transplant. 2012; 47:663–668. PMID:
21765479.

36. Chen X, Hale GA, Barfield R, et al. Rapid immune reconstitution after a reduced-intensity conditioning regimen and a CD3-depleted haploidentical stem cell graft for paediatric refractory haematological malignancies. Br J Haematol. 2006; 135:524–532. PMID:
17010105.

37. Vantourout P, Hayday A. Six-of-the-best: unique contributions of γδ T cells to immunology. Nat Rev Immunol. 2013; 13:88–100. PMID:
23348415.

38. Norell H, Moretta A, Silva-Santos B, Moretta L. At the Bench: Preclinical rationale for exploiting NK cells and γδ T lymphocytes for the treatment of high-risk leukemias. J Leukoc Biol. 2013; 94:1123–1139. PMID:
24108703.

39. Hu Y, Cui Q, Luo C, Luo Y, Shi J, Huang H. A promising sword of tomorrow: Human γδ T cell strategies reconcile allo-HSCT complications. Blood Rev. 2015; [Epub ahead of print].

40. Lamb LS Jr, Lopez RD. gammadelta T cells: a new frontier for immunotherapy? Biol Blood Marrow Transplant. 2005; 11:161–168. PMID:
15744234.
41. Locatelli F, Bauquet A, Palumbo G, Moretta F, Bertaina A. Negative depletion of α/β+ T cells and of CD19+ B lymphocytes: a novel frontier to optimize the effect of innate immunity in HLA-mismatched hematopoietic stem cell transplantation. Immunol Lett. 2013; 155:21–23. PMID:
24091162.

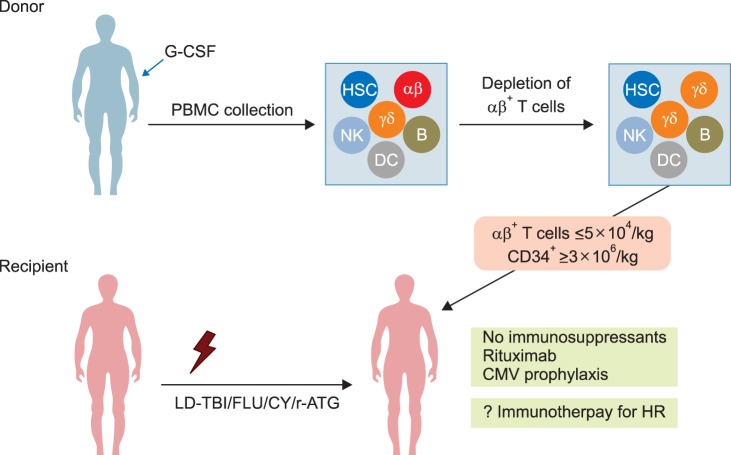
42. Handgretinger R. New approaches to graft engineering for haploidentical bone marrow transplantation. Semin Oncol. 2012; 39:664–673. PMID:
23206843.

43. Schumm M, Lang P, Bethge W, et al. Depletion of T-cell receptor alpha/beta and CD19 positive cells from apheresis products with the CliniMACS device. Cytotherapy. 2013; 15:1253–1258. PMID:
23993299.

44. Bertaina A, Merli P, Rutella S, et al. HLA-haploidentical stem cell transplantation after removal of αβ+ T and B cells in children with nonmalignant disorders. Blood. 2014; 124:822–826. PMID:
24869942.

45. Maschan M, Shelikhova L, Ilushina M, et al. TCR-alpha/beta and CD19 depletion and treosulfan-based conditioning regimen in unrelated and haploidentical transplantation in children with acute myeloid leukemia. Bone Marrow Transplant. 2016; [Epub ahead of print].

46. Lang P, Feuchtinger T, Teltschik HM, et al. Improved immune recovery after transplantation of TCRαβ/CD19-depleted allografts from haploidentical donors in pediatric patients. Bone Marrow Transplant. 2015; 50(Suppl 2):S6–S10. PMID:
26039210.

47. Sarkodee-Adoo C, Sotirescu D, Sensenbrenner L, et al. Thrombotic microangiopathy in blood and marrow transplant patients receiving tacrolimus or cyclosporine A. Transfusion. 2003; 43:78–84. PMID:
12519434.
48. Ho VT, Cutler C, Carter S, et al. Blood and marrow transplant clinical trials network toxicity committee consensus summary: thrombotic microangiopathy after hematopoietic stem cell transplantation. Biol Blood Marrow Transplant. 2005; 11:571–575. PMID:
16041306.

49. Hinchey J, Chaves C, Appignani B, et al. A reversible posterior leukoencephalopathy syndrome. N Engl J Med. 1996; 334:494–500. PMID:
8559202.

50. Koh KN, Park M, Kim BE, Im HJ, Seo JJ. Early central nervous system complications after allogeneic hematopoietic stem cell transplantation in children. Korean J Hematol. 2010; 45:164–170. PMID:
21120204.

51. Ciceri F, Lupo-Stanghellini MT, Korthof ET. Haploidentical transplantation in patients with acquired aplastic anemia. Bone Marrow Transplant. 2013; 48:183–185. PMID:
23292235.

52. Im HJ, Koh KN, Choi ES, et al. Excellent outcome of haploidentical hematopoietic stem cell transplantation in children and adolescents with acquired severe aplastic anemia. Biol Blood Marrow Transplant. 2013; 19:754–759. PMID:
23380343.
53. Clay J, Kulasekararaj AG, Potter V, et al. Nonmyeloablative peripheral blood haploidentical stem cell transplantation for refractory severe aplastic anemia. Biol Blood Marrow Transplant. 2014; 20:1711–1716. PMID:
25016195.

54. Gao L, Li Y, Zhang Y, et al. Long-term outcome of HLA-haploidentical hematopoietic SCT without in vitro T-cell depletion for adult severe aplastic anemia after modified conditioning and supportive therapy. Bone Marrow Transplant. 2014; 49:519–524. PMID:
24464145.

55. Wang Z, Zheng X, Yan H, Li D, Wang H. Good outcome of haploidentical hematopoietic SCT as a salvage therapy in children and adolescents with acquired severe aplastic anemia. Bone Marrow Transplant. 2014; 49:1481–1485. PMID:
25133891.

56. Esteves I, Bonfim C, Pasquini R, et al. Haploidentical BMT and post-transplant Cy for severe aplastic anemia: a multicenter retrospective study. Bone Marrow Transplant. 2015; 50:685–689. PMID:
25730184.

57. Im HJ, Koh KN, Seo JJ. Haploidentical hematopoietic stem cell transplantation in children and adolescents with acquired severe aplastic anemia. Korean J Pediatr. 2015; 58:199–205. PMID:
26213547.

58. Liu L, Wang X, Jin S, et al. Haploidentical hematopoietic stem cell transplantation for nonresponders to immunosuppressive therapy against acquired severe aplastic anemia. Bone Marrow Transplant. 2016; 51:424–427. PMID:
26479978.

59. Teschner D, Distler E, Wehler D, et al. Depletion of naive T cells using clinical grade magnetic CD45RA beads: a new approach for GVHD prophylaxis. Bone Marrow Transplant. 2014; 49:138–144. PMID:
23933765.

60. Triplett BM, Shook DR, Eldridge P, et al. Rapid memory T-cell reconstitution recapitulating CD45RA-depleted haploidentical transplant graft content in patients with hematologic malignancies. Bone Marrow Transplant. 2015; 50:968–977. PMID:
25665048.

61. Bleakley M, Heimfeld S, Loeb KR, et al. Outcomes of acute leukemia patients transplanted with naive T cell-depleted stem cell grafts. J Clin Invest. 2015; 125:2677–2689. PMID:
26053664.

62. Feuchtinger T, Opherk K, Bethge WA, et al. Adoptive transfer of pp65-specific T cells for the treatment of chemorefractory cytomegalovirus disease or reactivation after haploidentical and matched unrelated stem cell transplantation. Blood. 2010; 116:4360–4367. PMID:
20625005.

63. Feucht J, Joachim L, Lang P, Feuchtinger T. Adoptive T-cell transfer for refractory viral infections with cytomegalovirus, Epstein-Barr virus or adenovirus after allogeneic stem cell transplantation. Klin Padiatr. 2013; 225:164–169. PMID:
23700092.

64. Gerdemann U, Katari UL, Papadopoulou A, et al. Safety and clinical efficacy of rapidly-generated trivirus-directed T cells as treatment for adenovirus, EBV, and CMV infections after allogeneic hematopoietic stem cell transplant. Mol Ther. 2013; 21:2113–2121. PMID:
23783429.

65. Icheva V, Kayser S, Wolff D, et al. Adoptive transfer of epsteinbarr virus (EBV) nuclear antigen 1-specific t cells as treatment for EBV reactivation and lymphoproliferative disorders after allogeneic stem-cell transplantation. J Clin Oncol. 2013; 31:39–48. PMID:
23169501.

66. Wilhelm M, Kunzmann V, Eckstein S, et al. Gammadelta T cells for immune therapy of patients with lymphoid malignancies. Blood. 2003; 102:200–206. PMID:
12623838.
67. Gomes AQ, Martins DS, Silva-Santos B. Targeting γδ T lymphocytes for cancer immunotherapy: from novel mechanistic insight to clinical application. Cancer Res. 2010; 70:10024–10027. PMID:
21159627.
68. Fisher JP, Heuijerjans J, Yan M, Gustafsson K, Anderson J. γδ T cells for cancer immunotherapy: A systematic review of clinical trials. Oncoimmunology. 2014; 3:e27572. PMID:
24734216.
69. Wilhelm M, Smetak M, Schaefer-Eckart K, et al. Successful adoptive transfer and in vivo expansion of haploidentical γδ T cells. J Transl Med. 2014; 12:45. PMID:
24528541.

70. Rubnitz JE, Inaba H, Ribeiro RC, et al. NKAML: a pilot study to determine the safety and feasibility of haploidentical natural killer cell transplantation in childhood acute myeloid leukemia. J Clin Oncol. 2010; 28:955–959. PMID:
20085940.

71. Choi I, Yoon SR, Park SY, et al. Donor-derived natural killer cells infused after human leukocyte antigen-haploidentical hematopoietic cell transplantation: a dose-escalation study. Biol Blood Marrow Transplant. 2014; 20:696–704. PMID:
24525278.

72. Shah NN, Baird K, Delbrook CP, et al. Acute GVHD in patients receiving IL-15/4-1BBL activated NK cells following T-cell-depleted stem cell transplantation. Blood. 2015; 125:784–792. PMID:
25452614.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download