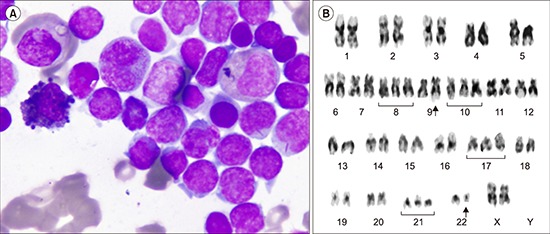
A 35-year-old woman had 2-month history of fever and bone pain, with an 8-kg weight loss in one month. Physical examination revealed 7-cm palpable spleen (splenomegaly). On admission, her hemoglobin level was 13.4 g/dL, white blood cell count was 144×109/L, and platelet count was 71×109/L. Bone marrow biopsy showed diffuse infiltration with blast cells. However, two populations of blast cells was observed; one population was large-sized, had abundant granular cytoplasm, and a few had Auer rods; the other population was comprised of medium-sized blast cells with scant and agranular cytoplasm (A). Flow cytometry was performed. Gating on CD45-positive cells revealed: TdT, 84%; CD79a, 79%; CD13, 68%; CD33, 88%; cMPO, 60%; and CD34, 96%. This cell population was negative for CD3, CD5, CD7, IgM, Kappa and Lambda. Bone marrow cytogenetics showed a complex karyotype in which t(9;22) and trisomies 8, 10, 17, and 21 were present (B). The diagnosis of mixed-phenotype acute leukemia with t(9;22) was made. Induction chemotherapy included vincristine, daunorubicin, cytarabine, cyclophosphamide, methotrexate, and imatinib; however, she died due to neutropenic sepsis after induction. Mixed-phenotype acute leukemia accounts for 3–5% of all cases of acute leukemia and is associated with a worse outcome.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download