TO THE EDITOR: We would like to share the following intriguing case with readers of Blood Research. A 72-year-old HIV-negative man presented with a 2-month history of gradual-onset generalized weakness, low-grade fever, and loss of weight and appetite. On examination, he had pallor and hepatosplenomegaly. His hemogram findings revealed a nearly normal hemoglobin level (11.8 g/dL), leukocytosis (15.8×109/L), and thrombocytopenia (78×109/L). Differential counts showed 3% circulating blasts apart from 6% immature myeloid cells, 4% basophils, and 2% monocytes. A bone marrow aspirate was hypercellular with 5% blasts along with dyserythropoiesis (36%, including 32% ring sideroblasts), dysgranulopoiesis (11%), and dysmegakaryopoiesis (40%). The trephine biopsy showed dyshemopoiesis along with World Health Organization grade 2 reticulin fibrosis. Tests for the detection of BCR-ABL1 fusion gene and JAK2 mutations were negative. A diagnosis of myelodysplastic syndrome/myeloproliferative neoplasm-unclassifiable (MDS/MPN-U) was made [1].
Subsequently, the patient was lost to follow-up, but 7 months later, he visited the emergency room with a high-grade fever with chills and rigors, altered sensorium, and irrelevant talking. On examination, he had neck rigidity, a positive Kernig sign, and right lower limb monoparesis along with hepatosplenomegaly. A computed tomographic scan of his head and cerebrospinal fluid examination were normal. Blood and urine bacterial cultures were sterile. At this time, the hemogram revealed anemia (hemoglobin level, 6.0 g/dL), thrombocytopenia (19×109/L), and leukocytosis (63.5×109/L) with a differential similar to that obtained 7 months previously. A bone marrow aspirate also revealed a picture similar to that of the previous marrow aspirate. The striking finding noticed at the time of peripheral blood and marrow evaluation was the presence of intracytoplasmic yeast forms (within neutrophils) conforming to Histoplasma species (Fig. 1). These were confirmed to be Histoplasma capsulatum based on fungal culture studies from peripheral blood (Fig. 1) as well as gene sequencing of the internal transcribed spacer region of the fungus. The patient died on the same day as the bone marrow procedure.
We present this case because this patient highlights an unusual morphological coexistence of a neoplastic and infective disorder [2]. A predisposing factor might have been the dysplastic neutrophils with defective phagocytic and microbicidal activity [3]. The case illustrates the importance of morphology in the era of genomics as well as the value of close interdisciplinary cooperation in diagnostic hematology. It also reinforces the dictum that hematopathologists must always stay on the alert for uncommon infections in unusual specimens, especially in tropical countries.
References
1. Vardiman JW, Bennett JM, Bain BJ, Baumann I, Thiele J, Orazi A. Myelodysplastic/myeloproliferative neoplasms, unclassifiable. In : Swerdlow SH, Campo E, Harris NL, editors. WHO classification of tumours of haematopoietic and lymphoid tissues. Lyon, France: IARC Press;2008. p. 85–86.
2. Sharma P, Tyagi S. An unusual cause of eosinophilia in aml-m4 without the Inv(16) abnormality. J Blood Disord Transfus. 2010; 1:104.

3. Mazzone A, Porta C, Fossati G, Gritti D, Mazzucchelli I, Ricevuti G. Granulocyte dysplasia and dysfunction, and CD11/CD18 defects in myelodysplastic syndromes. Leuk Lymphoma. 1996; 23:267–275. PMID: 9031107.

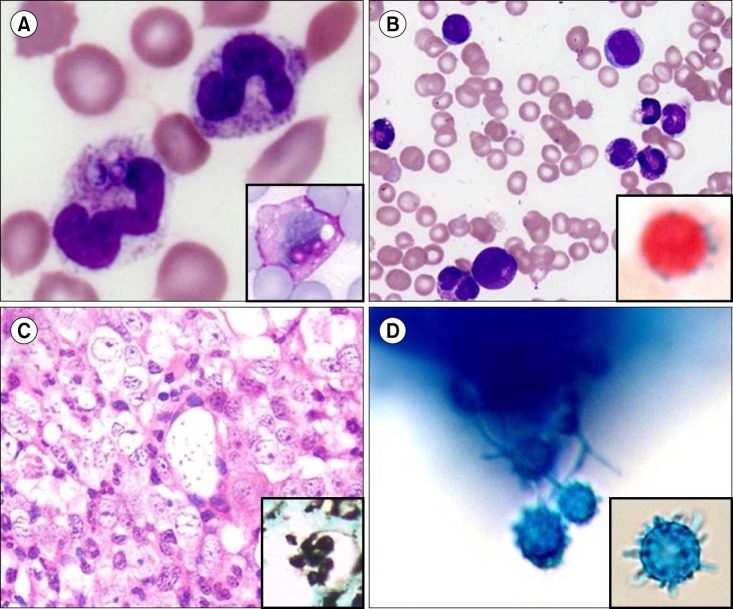
Fig. 1
(A) Peripheral blood shows neutrophils with toxic granules and two intra-cytoplasmic yeast forms of Histoplasma capsulatum in the cell on the left (May-Grunwald Giemsa, ×1,000). Inset: The fungus was brightly positive for periodic acid–Schiff stain (hematoxylin counterstain, ×1,000). (B) Hemodilute bone marrow smears showed dysgranulopoiesis with 5% blasts (May-Grunwald Giemsa, ×1,000). Inset: Ring sideroblasts comprised 32% of all cells (Perls' Prussian Blue reaction with neutral red counterstain, ×1,000). (C) Bone marrow biopsy showed intracellular yeast forms (hematoxylin and eosin, ×400). Inset: These were positive for Grocott's silver methenamine stain (methyl green counterstain, ×1,000). (D) Lactophenol cotton blue wet-mount preparation of the isolated mold shows thick-walled and tuberculate macroconidia, with a close-up in the inset (lactophenol cotton blue stain, ×1,000).




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download