1. Martinez-Lopez A, Curiel-Olmo S, Mollejo M, et al. MYD88 (L265P) somatic mutation in marginal zone B-cell lymphoma. Am J Surg Pathol. 2015; 39:644–651. PMID:
25723115.

2. Chong Y, Kang CS, Oh WJ, Kim TJ, Lee EJ. Nodal involvement of extranodal marginal zone lymphoma with extreme plasmacytic differentiation (Mott cell formation) simulating plasma cell neoplasm and lymphoplasmacytic lymphoma. Blood Res. 2014; 49:275–285. PMID:
25548763.

3. Xu L, Hunter ZR, Yang G, et al. Detection of MYD88 L265P in peripheral blood of patients with Waldenström's Macroglobulinemia and IgM monoclonal gammopathy of undetermined significance. Leukemia. 2014; 28:1698–1704. PMID:
24509637.

4. Staiger AM, Ott MM, Parmentier S, et al. Allele-specific PCR is a powerful tool for the detection of the MYD88 L265P mutation in diffuse large B cell lymphoma and decalcified bone marrow samples. Br J Haematol. 2015; 171:145–148. PMID:
25816840.
5. Jiménez C, Sebastián E, Chillón MC, et al. MYD88 L265P is a marker highly characteristic of, but not restricted to, Waldenström's macroglobulinemia. Leukemia. 2013; 27:1722–1728. PMID:
23446312.

6. Ko YH, Kim CW, Park CS, et al. REAL classification of malignant lymphomas in the Republic of Korea: incidence of recently recognized entities and changes in clinicopathologic features. Hematolymphoreticular Study Group of the Korean Society of Pathologists. Revised European-American lymphoma. Cancer. 1998; 83:806–812. PMID:
9708949.
7. Kim JA, Im K, Park SN, et al. MYD88 L265P mutations are correlated with 6q deletion in Korean patients with Waldenström macroglobulinemia. Biomed Res Int. 2014; 2014:363540. PMID:
24895570.

8. Kim Y, Ju H, Kim DH, et al. CD79B and MYD88 mutations in diffuse large B-cell lymphoma. Hum Pathol. 2014; 45:556–564. PMID:
24444466.

9. Choi JW, Kim Y, Lee JH, Kim YS. MYD88 expression and L265P mutation in diffuse large B-cell lymphoma. Hum Pathol. 2013; 44:1375–1381. PMID:
23380077.

10. Xu L, Hunter ZR, Yang G, et al. MYD88 L265P in Waldenström macroglobulinemia, immunoglobulin M monoclonal gammopathy, and other B-cell lymphoproliferative disorders using conventional and quantitative allele-specific polymerase chain reaction. Blood. 2013; 121:2051–2058. PMID:
23321251.

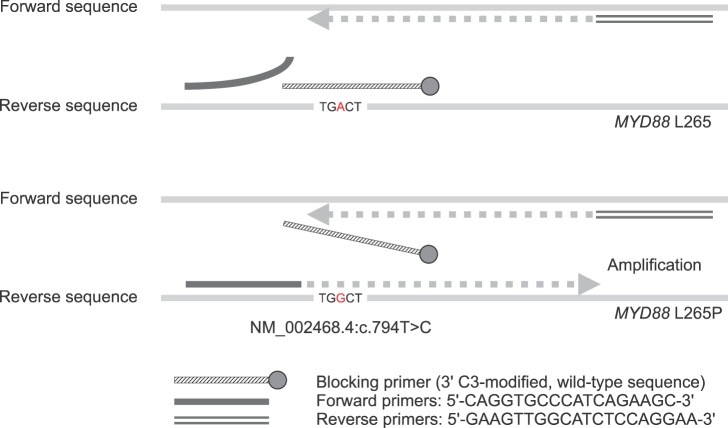
11. Lee ST, Kim JY, Kown MJ, et al. Mutant enrichment with 3'-modified oligonucleotides a practical PCR method for detecting trace mutant DNAs. J Mol Diagn. 2011; 13:657–668. PMID:
21979247.
12. Shin SY, Ki CS, Kim HJ, Kim JW, Kim SH, Lee ST. Mutant enrichment with 3'-modified oligonucleotides (MEMO)-quantitative PCR for detection of NPM1 mutations in acute myeloid leukemia. J Clin Lab Anal. 2015; 29:361–365. PMID:
25384962.
13. Lee ST, Kim SW, Ki CS, et al. Clinical implication of highly sensitive detection of the BRAF V600E mutation in fine-needle aspirations of thyroid nodules: a comparative analysis of three molecular assays in 4585 consecutive cases in a BRAF V600E mutation-prevalent area. J Clin Endocrinol Metab. 2012; 97:2299–2306. PMID:
22500044.

14. Treon SP, Xu L, Yang G, et al. MYD88 L265P somatic mutation in Waldenström's macroglobulinemia. N Engl J Med. 2012; 367:826–833. PMID:
22931316.

15. Varettoni M, Arcaini L, Zibellini S, et al. Prevalence and clinical significance of the MYD88 (L265P) somatic mutation in Waldenstrom's macroglobulinemia and related lymphoid neoplasms. Blood. 2013; 121:2522–2528. PMID:
23355535.
16. Varettoni M, Zibellini S, Arcaini L, et al. MYD88 (L265P) mutation is an independent risk factor for progression in patients with IgM monoclonal gammopathy of undetermined significance. Blood. 2013; 122:2284–2285. PMID:
24072850.

17. Kyle RA, Therneau TM, Rajkumar SV, et al. Long-term follow-up of IgM monoclonal gammopathy of undetermined significance. Blood. 2003; 102:3759–3764. PMID:
12881316.

18. Ngo VN, Young RM, Schmitz R, et al. Oncogenically active MYD88 mutations in human lymphoma. Nature. 2011; 470:115–119. PMID:
21179087.

19. Bonzheim I, Giese S, Deuter C, et al. High frequency of MYD88 mutations in vitreoretinal B-cell lymphoma: a valuable tool to improve diagnostic yield of vitreous aspirates. Blood. 2015; 126:76–79. PMID:
25900979.

20. Patkar N, Subramanian PG, Deshpande P, et al. MYD88 mutant lymphoplasmacytic lymphoma/Waldenström macroglobulinemia has distinct clinical and pathological features as compared to its mutation negative counterpart. Leuk Lymphoma. 2015; 56:420–425. PMID:
24828863.
21. Schmidt J, Federmann B, Schindler N, et al. MYD88 L265P and CXCR4 mutations in lymphoplasmacytic lymphoma identify cases with high disease activity. Br J Haematol. 2015; 169:795–803. PMID:
25819228.
22. Braggio E, Dogan A, Keats JJ, et al. Genomic analysis of marginal zone and lymphoplasmacytic lymphomas identified common and disease-specific abnormalities. Mod Pathol. 2012; 25:651–660. PMID:
22301699.

23. Farinha P, Gascoyne RD. Molecular pathogenesis of mucosa-associated lymphoid tissue lymphoma. J Clin Oncol. 2005; 23:6370–6378. PMID:
16155022.

24. Ondrejka SL, Lin JJ, Warden DW, Durkin L, Cook JR, Hsi ED. MYD88 L265P somatic mutation: its usefulness in the differential diagnosis of bone marrow involvement by B-cell lymphoproliferative disorders. Am J Clin Pathol. 2013; 140:387–394. PMID:
23955458.
25. Capaldi IB, May AM, Schmitt-Graeff A, et al. Detection of MYD88 L265P mutations in formalin-fixed and decalcified BM biopsies from patients with lymphoplasmacytic lymphoma. Exp Mol Pathol. 2014; 97:57–65. PMID:
24842316.

26. Newton CR, Graham A, Heptinstall LE, et al. Analysis of any point mutation in DNA. The amplification refractory mutation system (ARMS). Nucleic Acids Res. 1989; 17:2503–2516. PMID:
2785681.

27. Jang MA, Lee ST, Oh YL, et al. Identification of a rare 3 bp BRAF gene deletion in a thyroid nodule by mutant enrichment with 3'-modified oligonucleotides polymerase chain reaction. Ann Lab Med. 2012; 32:238–241. PMID:
22563563.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download