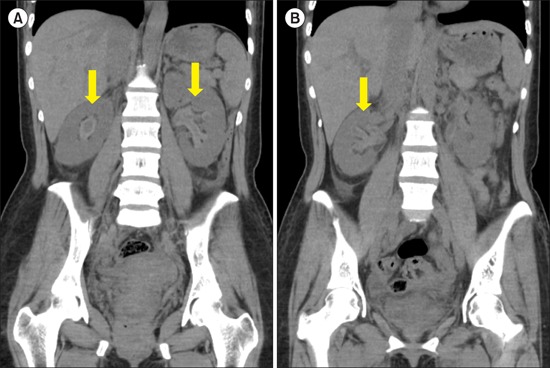
A 40-year-old woman presented to our emergency room with a bleeding tendency and thrombocytopenia. Ten days ago, she was diagnosed with immune thrombocytopenic purpura (ITP) at another hospital after a complete hematologic work-up, including bone marrow biopsy. Despite high-dose steroid treatment (dexamethasone 40 mg/day for 4 days), the platelet count did not rise. Even after administering intravenous immunoglobulin (120 g/day for 2 days) the platelet count declined to 5,000/mm3. She received single-dose vincristine (1 mg) for gross hematuria and was then transferred to our hospital. Upon admission, she showed anuria and a sharp increase in creatinine levels but no evidence of microangiopathic hemolytic anemia. Abdominopelvic computed tomography (CT) revealed hyperdensity at the bilateral renal pelvis extending into the upper ureters (A, B). We performed hemodialysis and prescribed eltrombopag 25 mg/day. The platelet count gradually increased with recovery of urine output 7 days later. Follow-up CT showed regression of the hyperdensity occupying the bilateral renal pelvis. Spontaneous suburothelial hemorrhage usually occurs in patients with coagulopathy and hereditary bleeding diathesis and has never occurred in ITP patients. However, in cases of anuria followed by gross hematuria in ITP patients, postrenal acute renal failure caused by bilateral suburothelial hemorrhage should be considered. Herein, hyperdensity at and thickening of the renal pelvis and ureteral wall on non-enhanced CT served as diagnostic indicators.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download